Fig. 34.1
Mammary asymmetry: a 60-year-old patient who had in situ ductal carcinoma in the left breast in 2003 and who underwent conservative surgery, radiotherapy, and mastoplasty in the opposite breast. Photograph taken in 2012 showing asymmetric volume and position of the inframammary fold (photograph from Rodrigo Cericatto)
It is important to preserve the inframammary fold in oncologic breast surgical procedures whenever possible. In certain situations, the fold can be moved to a lower or upper position. Therefore, during a mastectomy, surgeons should prevent the dissection from extending far beyond the inframammary fold, thus preventing the creation of an undefined fold. For this reason, special attention should be paid to the ptosis of the reconstructed breast and inframammary fold positioning in postmastectomy reconstructions [3, 4].
34.2 When Should Reconstruction Be Performed?
In general, inframammary fold reconstruction should only be performed after the skin overlying the chest wall achieves good mobility. Thus, fold reconstruction should be performed 4–6 months after late postmastectomy breast reconstruction, using a tissue expander, a direct prosthesis or a myocutaneous flap. In surgical procedures initially using a tissue expander, fold reconstruction should be performed only when the expander is replaced with the prosthesis. The need to improve fold definition is then considered [1, 4, 5].
34.3 Indications for Inframammary Fold Reconstruction
Inframammary fold reconstruction is mainly performed in the case of late postmastectomy breast reconstruction. The anatomical landmark of the original fold site cannot be preserved because of large skin excision and upward dislocation of the inframammary fold as a result of skin closure. A poorly defined inframammary fold is usually created as a consequence of the use of a tissue expander or direct prosthesis placement (in the case of smaller breast volume), or even when using myocutaneous flaps, resulting in an unnatural appearance of the new breast in terms of shape and ptosis. Late effects of additional radiotherapy may also interfere with the position and the definition of the inframammary fold (Fig. 34.2). The result often seems satisfactory when each breast is assessed individually, but not when considering the symmetry with the opposite breast [4].
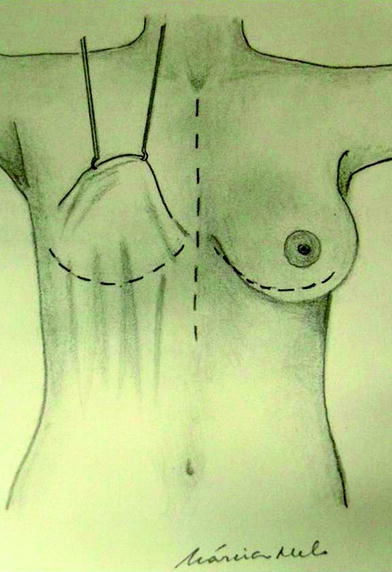
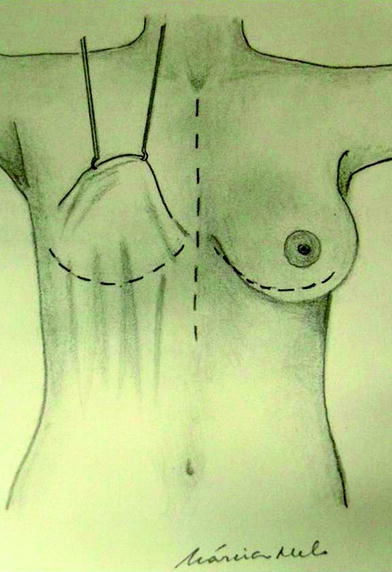
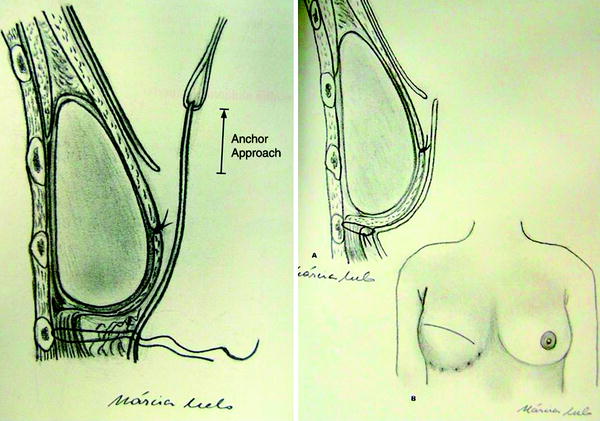
Fig. 34.2
Planning late breast reconstruction and inframammary fold projection (from Biazús et al. [6])
34.4 Surgical Planning
After the technique to be used for inframammary fold reconstruction has been chosen, skin marking is performed with the patient in a sitting or standing position, in the preoperative setting (Fig. 34.3) [3, 6].
The patient can be instructed to bring her external prosthesis bra to assist with the skin marking of the fold site. After the fold position has been marked with the patient wearing her bra, it is taken off, and the marked breast is compared with the contralateral breast. Marking is usually located on or immediately below the sixth rib along the breast meridian line [4].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree