Advances in Autologous Breast Reconstruction with Pedicled Perforator Flaps
Keywords
• Perforator flap • Pedicled perforator flap • Breast conservation therapy • Partial mastectomy • Autologous breast augmentation • Fat grafting • Tissue scaffold • Tissue matrix
Overview
BCT is the surgical excision of a breast cancer with a tumor-free margin while preserving the remainder of the uninvolved breast. Adjuvant breast irradiation is mandatory. This treatment modality has become the first choice for patients with early breast cancers because it has proved oncologically sound with survival rates similar to that of total mastectomy while providing associated aesthetic and psychological benefits.1,2 Patient selection, however, is important. A relative contraindication is a woman with a large tumor in a small breast; in these patients, the aesthetic outcome of BCT is poor.3,4 To overcome this, oncoplastic techniques that resect the tumor along breast reduction patterns or redistribute the remaining parenchyma via breast rearrangement may be used, along with reduction or mastopexy of the contralateral breast for symmetry.5–10 There is a limit, however, to how much volume displacement techniques are able to achieve in masking the volume discrepancy and contour abnormality from tumor resection. Patients with larger tumor-to-breast ratios were not considered suitable candidates for this procedure and were treated with total mastectomy with or without reconstruction. Volume replacement techniques import tissues, mainly from the regions surrounding the breast. The latissimus dorsi (LD) flap is a prime example of a musculocutaneous flap that has been used for partial breast reconstruction.11,12 The sacrifice of a substantial muscle, however, results in significant donor site morbidity, in particular, seroma formation and detrimental effects on shoulder function.
PPFs are a recent development in the field of breast reconstruction.13–15 Their main role is in the reconstruction of partial mastectomy defects with minimal donor site morbidity by preservation of the underlying muscles. They allow breast surgeons to resect a tumor with as much margins as oncologically necessary without fear of a poor cosmetic result.16,17 Moreover, these flaps act as a vascularized tissue scaffold that support the survival of free fat grafts. This is especially important given that adjuvant breast irradiation is mandatory in BCT, and fat transfer may be used to reverse the late sequelae of radiation and function as filler to correct residual volume and contour abnormalities.
Pedicled perforator flaps in breast surgery
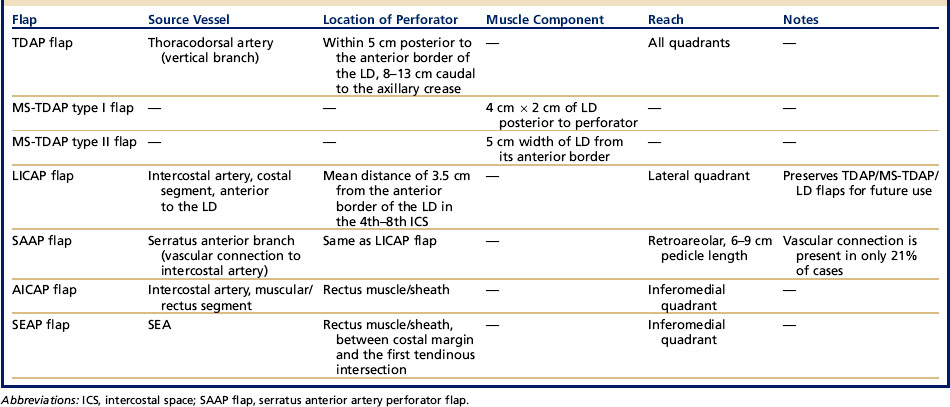
The PPFs that are useful for breast reconstruction may be classified according to the source vessel the perforator arises from, namely the thoracodorsal artery, the intercostal artery, the branch to the serratus anterior, and the superior epigastric artery (SEA) (Table 1).15–20
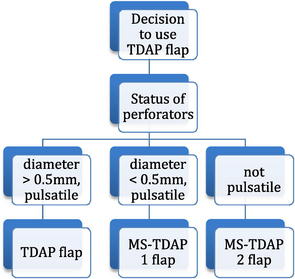
A variable segment of the LD muscle may need to be included due to anatomic variations that become apparent only intraoperatively. In these cases, the thoracodorsal artery perforator (TDAP) flap is converted to a muscle-sparing TDAP (MS-TDAP). The flap is harvested based on the status of the TDAPs,16,18 as indicated in the following algorithm.
When there are multiple perforators but are of small caliber, or when the perforators are nonpulsatile, then the MS-TDAP type II flap is harvested. A larger segment of muscle (up to 5 cm width) at the anterior border of the LD is included with the flap. This serves to capture the maximum number of perforators from the vertical branch of the thoracodorsal artery, which are located within the anterior 5 cm of the LD muscle between 8 cm and 13 cm caudal to the axillary crease. An MS-TDAP type II flap may also be used when a segment of the LD muscle is needed, such as when more bulk is required or to cover an implant. A similar technique can be used by surgeons with limited experience in perforator flaps during their initial cases of TDAP flaps. Isolating the perforator with the anterior cuff of the LD muscle enables breast surgeons to achieve a satisfactory reconstruction expediently and safely, with limited donor site morbidity, even in difficult cases.16,18
Indications and contraindications
Current indications for PPFs in breast surgery are summarized in (Box 1).
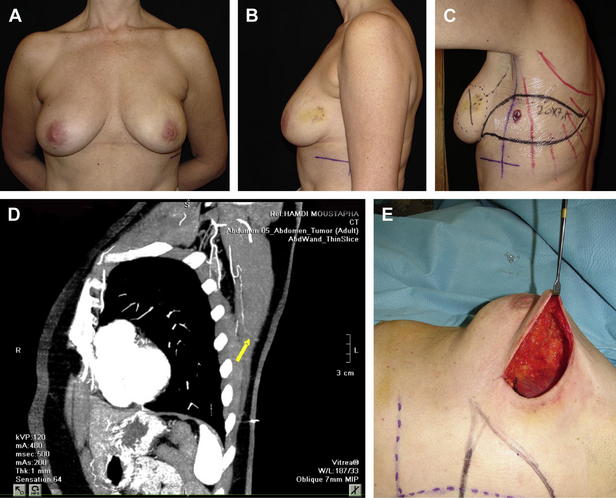
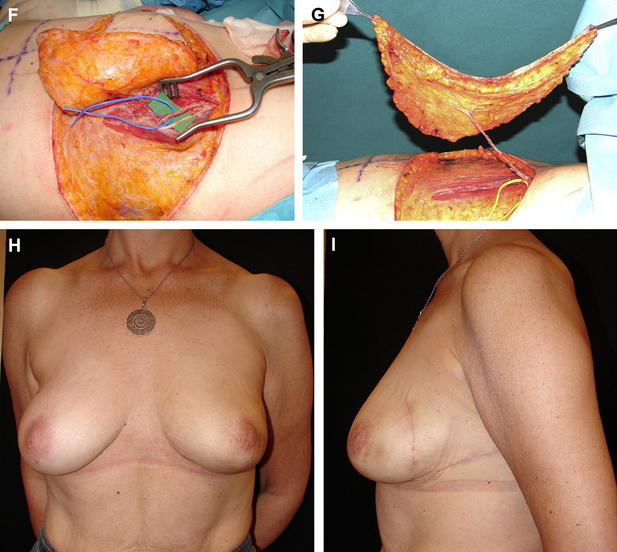
Immediate Partial Breast Reconstruction
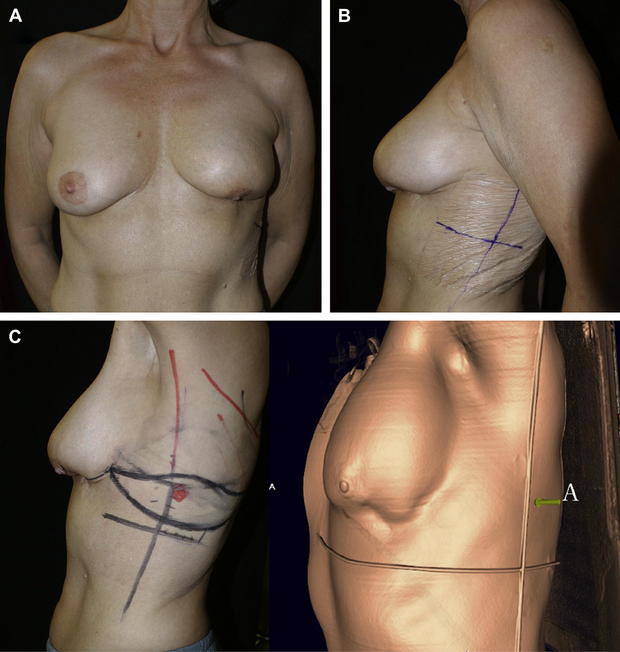
PPFs replace volume by recruiting well-vascularized tissues from around the breast. They therefore expand the indications of breast conservation surgery to include women with larger tumor-to-breast volume ratios than was previously possible while maximizing aesthetic outcome. The major indications of the PPFs are defects that are larger than 30% of the breast or in cases where the tumor resection results in unacceptable aesthetic result (Fig. 1). Another relative indication is in women who, despite having adequate tissue for breast rearrangement (volume displacement) surgery, prefer to maintain their original breast volume without reducing the contralateral breast.
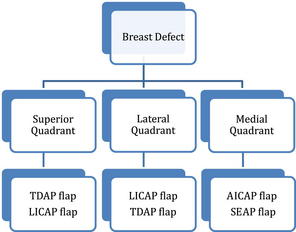
The choice of flap depends on the location of the tissue defect, the available donor sites, and the volume and type of tissue to be replaced.16,17 From an anatomic standpoint, the breast is divided into quadrants relative to a horizontal and a vertical line passing through the nipple. This is also a useful description when planning reconstruction. The LICAP flap is primarily indicated for lateral defects because of its short pedicle.15,16,19,21 The TDAP flap with its longer pedicle is usually able to cover all quadrants. Medial quadrants may be reconstructed with the anterior intercostal artery perforator (AICAP) or SEA perforator (SEAP) flaps, which are harvested from the upper abdominal areas.15,19,20 The following algorithm shows flap choice as related to breast quadrants.
Delayed Partial Breast Reconstruction
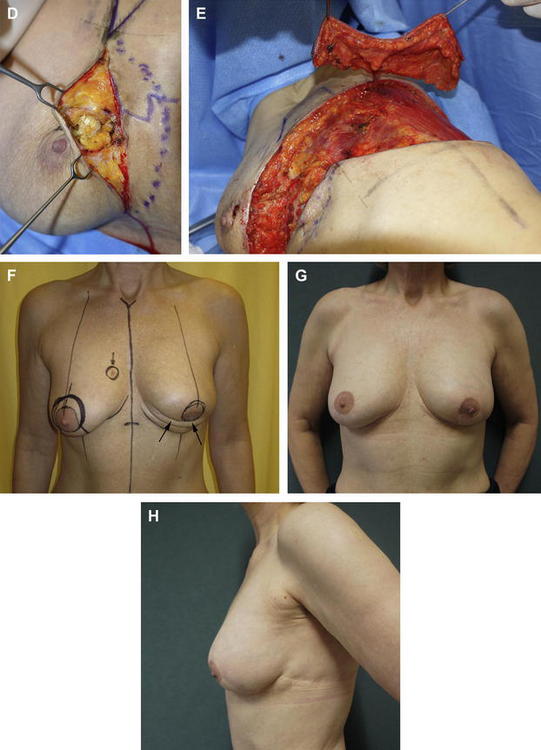
Delayed partial breast reconstruction should be considered when post-BCT deformities occur. Several classification systems have been developed to characterize delayed breast deformities and their suggested reconstructive options.3,10,17 Most of these deformities can be treated with serial fat injections. However, when moderate to severe radiation sequelae are associated with major deformity involving 2 or more breast quadrants or are larger than 20% of the initial breast size, then PPFs are indicated (Fig. 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree