9 Importance of Vascularity and Selecting the Recipient Vessels in Lower Extremity Reconstruction
Summary
Successful lower extremity reconstruction using free flaps begins by identifying a good recipient vessel and understanding the surrounding environment of the defect. One should consider multiple factors when selecting the recipient vessel, such as the status of the axial arteries, trying to preserve flow as much as possible, extent and severity of the defect, and ultimately choosing the ideal type of anastomosis. However, the ultimate decision should be made on the operating table during surgery when the actual artery or vein is exposed and it shows signs of good pulsation and flow.
Keywords: Microsurgery, selecting recipient vessels, vascular status of extremity
9.1 Introduction
Reconstructive microsurgery has played a pivotal role in achieving results where limb salvage reconstruction outcomes are similar to primary amputations.1,2 Nevertheless, lower extremity reconstruction remains difficult due to multiple factors involved during reconstruction such as timing, wide zone of injury, infection, status of vascularity, and the long and complex process of healing till complete weight bearing. Now with the concept of reconstructive elevator to reach the ideal rung of reconstruction providing the best possible timely option to achieve aesthetic as well as functional outcome, it often requires the thinking and use of complex microsurgical procedures.3 Despite the fact that normal function and appearance can be difficult to achieve, it may be warranted to support successful reconstruction leading to successful salvage of the extremity. Furthermore, microsurgical reconstruction of the lower extremity is now accepted as a safe process with acceptable rate of flap failures according to a meta-analysis by Xiong et al.4
The classical approach for lower extremity reconstruction using free flaps dictates the following: anastomose the vessel outside the zone of injury, make end-to-side arterial anastomosis and end-to-side or end-to-end venous anastomosis, and reconstruct the soft tissues first and then restore the skeletal support.5 Although these teachings are still very valuable, they may not always be applicable to complex situations where vascular structures are poor and the zone of injury is complex and wide, making selection of recipient vessels complicated and confusing.
Once the decision is made for reconstructive microsurgery, complex or simple, selection of recipient vessels is one of the key factors in achieving successful outcomes. Once the recipient site is secured, one can choose the type of flap based on the pedicle length.6 Inversely, one should consider where to select the recipient in regard to the flap that is chosen. In this chapter, we will review how to evaluate the lower extremity in regard to major vessels, select the recipient site, and the method of anastomosis.
9.2 Factors to Consider
9.2.1 Evaluating the Lower Extremity Vascular Status
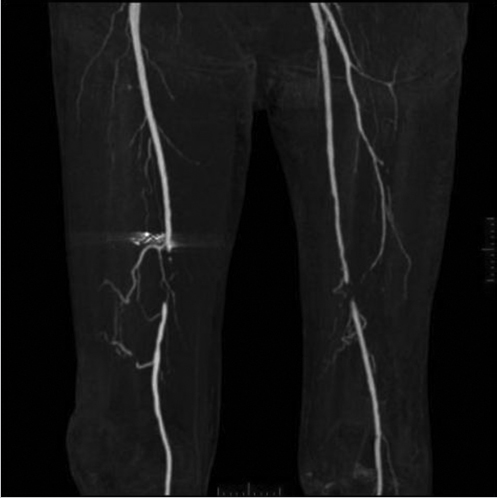
After the decision is made to reconstruct the lower extremity, the first preoperative evaluation should start with vascular status. Without adequate vascular supply, microsurgical reconstruction will not be possible. This is especially true for ischemic conditions after trauma and ischemic chronic wounds. Most often, physical examination of palpable pulse, color, capillary refill, and turgor of the extremity allows us to assess the initial status. With the handheld Doppler examination, further information can be obtained.7 The use of preoperative arteriography for lower extremity reconstruction is considered when physical/Doppler examination reveals inconclusive vascular status or chronic vascular disease is suspected. It is usually performed for patients who have loss of one or more peripheral pulses, a neurologic deficit secondary to the injury, or a compound fracture of the extremity that has undergone reduction and either external or internal fixation.8 In association with prior injuries to the lower extremity, the routine preoperative use of angiogram is controversial.7,8,9,10,11,12,13 However, in our experience, 75 to 80% of lower extremity reconstruction that involves trauma, chronic wounds, and oncologic reconstruction may be indicated for detailed vascular evaluation. If angiogram is required, the simpler way is to obtain the vascular status by computed tomography (CT) angiography of the recipient region without the risk of complications from arterial puncture of the groin. In addition, it can provide vascular information of the donor flap when selected from the extremity, facilitating the planning and the surgical procedure.11,14,15▶ Fig. 9.1 shows a patient with a diabetic foot having obstruction of both femoral artery and distal circulation being supplied by collateral vessels. This patient exhibited normal handheld Doppler findings and thus justifies the angiogram in patients with chronic conditions such as diabetes. It also shows the quality of the artery whether or not it is calcified proximal to the lesion, which may warrant angioplasty to improve distal flow. This can be frequently seen in patients with diabetes or other peripheral artery disease. Furthermore, it shows you whether or not calcification is present on the recipient artery, thus helping you to decide on selection of the artery near the defect. Finally, the CT angiogram when programed can see though the venous phase, detecting the superficial veins and the presence of deep vein thrombosis. However, in the cases where hardware is applied, it may distort the image. In these cases, although more invasive, classical angiogram will help the surgeon to determine the vascular status.
At this phase of evaluation, one should consider which major vessels are available to anastomose the flap: the anterior, posterior, or peroneal artery. One should remember that multiple variations of major vessels may be present. Some frequent variations are peroneus magna and distally intact (proximal injured) posterior or anterior artery by connecting the collaterals.16 Taking all this into account, preoperative radiological evaluation of the major vessels will allow you to obtain good information and thus will allow you to facilitate the reconstruction process.
Fig. 9.1 A patient with a diabetic foot having obstruction of both femoral artery and distal circulation being supplied by collateral vessels. This patient exhibited normal hand-held Doppler findings and thus justifies the angiogram in patients with chronic condition such as diabetes. If one would harvest the anterolateral thigh flap without this knowledge, it would be catastrophic for the limb circulation as the major collateral vessel is the descending branch of the lateral circumflex femoral artery.
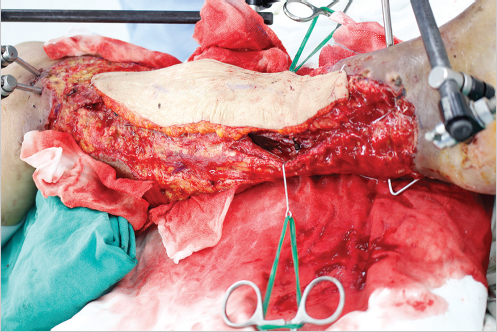
Fig. 9.2 One of the most important factors in selecting the recipient vessel may be the vascular quality itself and as long as the recipient vessels are healthy with pulsation and adequate outflow after opening the vessel, it can be presumed to be usable as seen in this figure where circumflex iliac artery perforator flap was used to anastomose end-to-side on the anterior tibial artery within the zone of injury.
9.2.2 Zone of Injury
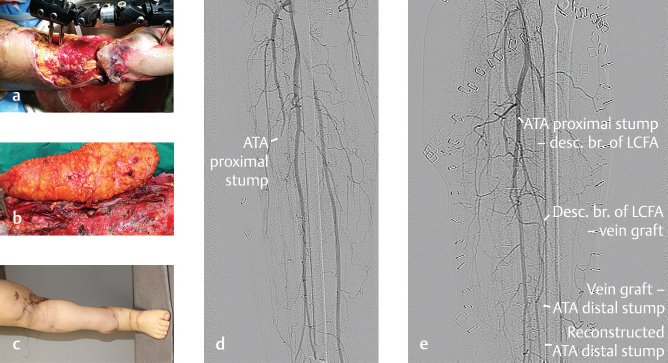
While burn and radiation injury may have a more definable zone of injury, many lower extremity wounds resulting from high-energy trauma have obscured zones of injury. The exact definition of the zone of injury still remains unclear and unreproducible.17 However, this concept is clinically important as the thrombogenic zone is known to extend beyond what is macroscopically evident and failure to recognize the true extent of this zone is cited as a leading cause of microsurgical anastomotic failure.9 This is more evident in the subacute period when usually the reconstructive consultation/transfer is made. Within this zone, perivascular changes such as increased friability of vessels and increased perivascular scar tissue may lead to difficult dissection of recipient vessels and higher incidence of thrombosis after anastomosis.18 There have been many reports on how to avoid the zone of injury by going proximal to the zone of injury. Searching for the recipient vessel proximal to the zone makes a lot of sense as the vascular injury is usually within the zone and proximal vessels can be assumed to be normal.19,20,21 Some studies even advocate using bypass grafts or arteriovenous (AV) loops linked to the proximal vessels to supply the vascularity to the flap to cover the defect.22,23,24 If there are injured major vessel stumps close to the injury, one can explore the stump and often can see that it is quite usable. Using this stump will allow you to preserve maximal flow to the foot by avoiding sacrifice to the other major vessels, thus reducing the risk of developing ischemia in later life.24,25,26 However, multiple studies show that anastomosing the flap distal to the zone of injury really makes no difference in outcome.26,27,28,29 Thus, one must ask if one can make anastomosis in the zone of injury. Again, it is clinically very difficult to realize how extensive and what the zone of injury is. The zone of injury is not a two-dimensional concept but rather a three-dimensional concept and frequently deeper structures may be spared from injury with minimal or no injury to the vascular structures. The study by Isenberg and Sherman demonstrated that clinical presentation of the recipient vessel such as vessel wall pliability and the quality of blood from the transected end of the vessel was more important than the distance from the wound.30 Park et al also concluded that the site of injury and vascular status of the lower extremity were the most important factors in choosing a recipient vessel.28 This idea was further supported by successful anastomosis of the perforator adjacent to or within the zone of injury.31 With advances in microscopes, microsurgery instruments, and techniques, one can dissect the scarred vessels within the zone of injury and utilize them. Based on these findings, one of the most important factors in selecting the recipient vessel may be the vascular quality itself and as long as the recipient vessels are healthy with pulsation and adequate outflow after opening the vessel, it can be presumed to be usable (▶ Fig. 9.2).
9.2.3 Type of Anastomosis
The classical debate on end-to-end versus end-to-side anastomosis has been shown to have no difference in achieving flap success and has been found to be equally effective.25,32,33 If there is no difference in outcome, one should ask which one has more benefits for lower extremity reconstruction. Godina has advocated end-to-side anastomosis on extremity reconstruction based on advantages such as preservation of distal vasculature, avoidance of retraction and spasm of the recipient artery, and avoidance of flow disturbances from vessel mismatch.17,34 Our practice has found this to be true and that it allows a better solution when there is anastomotic problem and increases the revision options by preserving the axial artery. Furthermore, the flap’s vascular resistance plays a role in flap success. Reports have shown that muscle has less vascular resistance, while skin flaps have higher resistance, which implies when end-to-end anastomosis is performed one should use flaps with less resistance allowing the absorption of a high amount of flow into the flap.35,36,37 In the days of perforator flaps and skin flaps, one should take this fact into consideration and perform end-to-side anastomosis to allow the best possible physiologic flow. Other than these two major types of anastomosis, T-shaped or flow-through anastomosis also plays an important role to preserve or to reconstruct distal flow.38,39 In our experience, an extreme flow-through to reconstruct the injured major artery has shown to have a positive effect to combat infected wounds such as chronic osteomyelitis.40 Thus, if a gap is noted in the axial artery, flow-through anastomosis or bypass for the artery defect should be considered for the best possible reconstruction41,42 (▶ Fig. 9.3).