32 Implants and biomaterials
Synopsis
 What is a biomaterial? In order to discuss biomaterials, we must first define this term.
What is a biomaterial? In order to discuss biomaterials, we must first define this term.
 There are many definitions of biomaterials but a widely used one from the National Institutes of Health defines a biomaterial as “any substance (other than a drug) or combination of substances synthetic or natural in origin, which can be used for any period of time, as a whole or part of a system which treats, augments, or replaces tissue, organ, or function of the body.”1
There are many definitions of biomaterials but a widely used one from the National Institutes of Health defines a biomaterial as “any substance (other than a drug) or combination of substances synthetic or natural in origin, which can be used for any period of time, as a whole or part of a system which treats, augments, or replaces tissue, organ, or function of the body.”1
 With the advent of tissue engineering and regenerative medicine in recent years, the definition has broadened to include “any material used in a medical device intended to interact with biological systems,” allowing for structures and combination devices that actively interact with the body to be included in the field.2
With the advent of tissue engineering and regenerative medicine in recent years, the definition has broadened to include “any material used in a medical device intended to interact with biological systems,” allowing for structures and combination devices that actively interact with the body to be included in the field.2
 Biomaterials can be synthetic (i.e., those made by humans) or biological (i.e., those produced by a biological system).
Biomaterials can be synthetic (i.e., those made by humans) or biological (i.e., those produced by a biological system).
 Further classifications based on development stage or material characteristics are also common but are beyond the scope of this chapter.
Further classifications based on development stage or material characteristics are also common but are beyond the scope of this chapter.
Historical perspective
The development of biomaterials has exploded over the past 50 years. In fact, prior to World War II, the term “biomaterials” did not exist. Although there have been reports of biomaterials being used, in the form of sutures, 32 000 years ago,2,3 the vast majority of biomaterials have been developed in the last 60 years. The modern era of medical implants might be attributed to a British ophthalmologist, Harold Ridley, in the late 1940s. He noticed that shards of canopy plastic that had been unintentionally implanted in the eyes of Spitfire fighter pilots who had been shot at by enemy machine guns seemed to heal without any adverse reaction. He concluded that the plastic used to make the Spitfire canopy, poly(methyl-methacrylate), might be used to make implant lenses for patients with cataracts. In 1949 he implanted the first artificial lens into a human. This observation and innovation were the precursors to the modern intraocular lenses that are now used over 10 million times/year for patients with cataracts.2
Around the same time, several independent groups of surgeons and engineers developed biomaterial-based implants such as vascular grafts, hip replacements, and heart valves. These innovators defined the foundations of biomaterial science in an era before principles for medical materials were established. By the 1950s, as surgeons, engineers, and scientists continued to create these new implant materials, it became clear that there were certain properties that an ideal implant would impart. Cumberland4 and Scales5 described the properties of an ideal implant (Box 32.1).
Box 32.1
Properties of an ideal implant
Promotes permanent tissue repair
Tolerates infected environment
(Modified from Cumberland VH. A preliminary report on the use of prefabricated nylon weave in the repair of ventral hernia. Med J Aust. 1952;1:143–144; and Scales JT. Materials for hernia repair. Proc R Soc Med. 1953;46:647–652.)
Metals
Stainless steel
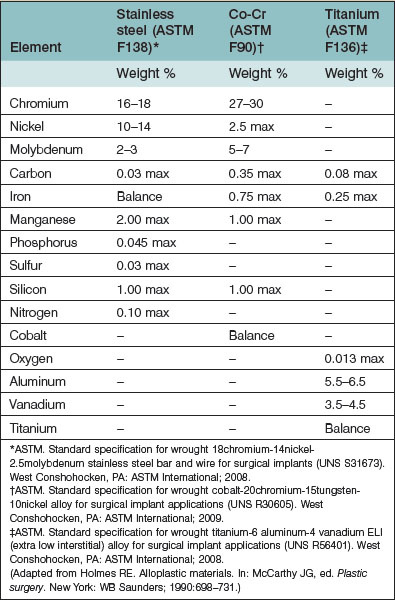
Stainless steel has been used as a biological implant since the 1920s.6 Stainless steel was designed to prevent corrosion and consists of over 10 individual compounds which provide it with the desired chemical and mechanical properties. The stainless steel used in medical applications are iron-chromium-nickel alloys with at least 17% chromium (Table 32.1). The chromium creates a protective surface, which contributes to the alloy’s anticorrosive properties. The most commonly used stainless steel alloy in medical applications is “316L” which, in addition to the chromium composition, has a low carbon content to prevent carbide formation, and a high nickel content to increase the strength and hardness of the alloy. Stainless steel has a relatively high tensile strength but is easily deformed (bent). While this is useful in some applications, such as the application of arch bars for maxillomandibular fixation, overall these mechanical properties are less desirable than other currently available materials such as cobalt-chromium and titanium. In addition, stainless steel can leach metallic ions into the surrounding tissues, causing a severe inflammatory reaction and pain, which may require surgical removal of the implants in some patients. Stainless steel is currently used in surgical wire and in arch bars. Historically rigid fixation systems utilized stainless steel but other alloys have replaced stainless steel in this application.
Cobalt-chromium
Historically, cobalt-chromium alloys have been one of the most significant biomaterials used in humans. Vitallium, a cobalt-chromium-molybdenum (Co-Cr-Mo) alloy (ASTM 75), was first described in 1932 to address some of the problems experienced with stainless steel. These alloys replace the iron with cobalt (~60% of the composition), increase the chromium to 25–30% for additional corrosion resistance, and contain 5–7% molybdenum for additional strength (Table 32.1). Co-Cr-Mo alloy was used in some of the early craniofacial miniplates and screws and helped to revolutionize that field. The major disadvantage of Co-Cr-Mo alloys is the scatter artifact on computed tomography (CT) imaging. Because of this, and several other benefits, titanium has essentially replaced Co-Cr-Mo alloys in most biomedical applications.7 However, it is still used in dental applications.
Titanium
Titanium alloys were introduced into medical applications in the early 1980s.6,8 Since that time these alloys have almost entirely replaced the other alloys in medical applications. This is because the titanium alloys are stronger, lighter, have higher resistance to corrosion, and generally cause less inflammation. Titanium also has less stress shielding (localized osteopenia secondary to the implant protecting the bone from normal loading) than other metal implants because they have less stiffness. Titanium alloys have less than 0.5% iron in them (Table 32.1), which provides them with two additional beneficial properties: they do not set off metal detectors, and they do not create a significant artifact on CT or magnetic resonance imaging studies. Finally, titanium can form chemical bonds with the surrounding mineralized bone without the typical fibrous tissue forming between the implant and bone. This unique characteristic allows titanium to be used to create osteointegrated implants. Plastic surgery applications of these alloys include plates and screws for rigid fixation of bone and mesh for use in applications such as orbital wall reconstruction (Fig. 32.1).
Gold
Although gold is chemically inert, in its pure form it has poor mechanical properties. Thus, when some strength is needed (for example, in dental fillings), a gold alloy is used. For applications such as eyelid weights in patients with lagophthalmos,9 where strength is less of an issue, 24-carat gold alloy (99.9% w/w purity) is commonly used to insure chemical inertness.
Platinum
Platinum is also used as a catalyst in the formation of some polymers. Platinum black, a fine powder (1 nm–1 µm) form of platinum, is used in many of these reactions.10 Platinum black catalyzes the addition of hydrogen to unsaturated organic compounds and is used in the production of silicone gel breast implants (see below).
Platinum complexes have also been used as chemotherapy and show good activity against some tumors. Cisplatin, the best-known platinum chemotherapeutic agent, has activity against multiple types of cancer. However, it has some significant side-effects, including cumulative irreversible kidney damage and deafness.11,12
Polymers
Silicone
Silicone is probably the most maligned and misunderstood biomaterial used in medicine today. This is likely due to the controversy revolving around the use of silicone in breast implants. Silicone gel-filled breast implants were first introduced in the US in 1962 and consisted of two shells made of thick, smooth-walled silicone elastomer, filled with a viscous silicone gel material (dimethylsiloxane) and glued together. Multiple variations and modifications to the shell and gel were made over the years in an attempt to improve the outcomes of breast augmentation and reduce the associated complications. In 1988, the US Food and Drug Administration (FDA), out of concerns from reports of implant failure and allegations of resultant complications and illness, relabeled breast implants as class III medical devices, and called for data from manufacturers showing the safety and effectiveness of these devices.13,14
In 1992, the FDA claimed that there was “inadequate information to demonstrate that breast implants were safe and effective” and placed a moratorium on silicone gel breast implants for cosmetic purposes but allowed their continued use for reconstruction after mastectomy, correction of congenital deformities, or replacement of ruptured silicone gel-filled implants due to medical or surgical reasons. In order to address this concern, the Department of Health and Human Services appointed the Institute of Medicine of the National Academy of Science (IOM) to begin one of the most extensive research studies in medical history. Their charge was to examine potential complications during or after silicone-based breast implant surgeries. In 1999, after reviewing years of evidence and research concerning silicone gel-filled breast implants, the IOM released a comprehensive report on both saline-filled and silicone gel-filled breast implants entitled Safety of Silicone Breast Implants.15 The IOM found that “evidence suggests diseases or conditions such as connective tissue diseases, cancer, neurological diseases or other systemic complaints or conditions are no more common in women with breast implants than in women without implants.” Most individual studies and all systemic review studies have also subsequently failed to find a link between silicone breast implants and disease.13,14
In 2006, the ban imposed by the FDA was lifted and restrictions on the use of silicone gel-filled breast implants produced by the two manufacturers for breast reconstruction and for cosmetic breast augmentation ended. The FDA approval required a complete 10-year study on women who have already received the implants and a 10-year study on the safety of the devices in 40 000 women. It was also mandated that patients be given brochures explaining the risks.13,14
So what is silicone? It is important to understand this question in light of the history of breast implants. Silicone is a family of polymers consisting of alternating silicon (Si) and oxygen (O) molecules. Table 32.2 shows the nomenclature of silicone. Siloxane, the basic repeating unit of silicone, consists of silicon, oxygen, and a saturated hydrocarbon (alkane) side group. Poly-dimethylsiloxane (PDMS) |(CH3)2SiO|n is the polymer used in most medical applications. PDMS is a very pure polymer that consists of the silicone backbone (silicon and oxygen) with two methyl side chains. It is one of the most inert biomaterials available for use in medical devices. Altering the length and molecular weight of the PDMS changes the mechanical properties and behavior of the silicone gel. PDMS molecules with less than 30 monomers are defined as low-molecular-weight formulations and have a viscosity similar to baby oil. High-molecular-weight formulations contain more than 3000 monomers and are solids. Controlling the degree of cross-linking, changing additives, and adjusting the curing process can also modify the mechanical properties of silicone. For example, the silicone gel found in breast implants is cured in a hydrosilation reaction where some of the methyl side chains (CH3) are replaced by vinyl side chains (CH CH2) that then allow the silicone chains to cross-link with each other. This reaction is catalyzed by platinum and some residual platinum can be found in silicone gel breast implants. The silicone shell on breast implants is made of fully polymerized silicone with an amorphous (noncrystalline) silica filler added for strength (Fig. 32.2).
CH2) that then allow the silicone chains to cross-link with each other. This reaction is catalyzed by platinum and some residual platinum can be found in silicone gel breast implants. The silicone shell on breast implants is made of fully polymerized silicone with an amorphous (noncrystalline) silica filler added for strength (Fig. 32.2).
Table 32.2 Silicone nomenclature
| Term | Chemical formula | Description |
|---|---|---|
| Silicon | Si | Most abundant element on earth Does not occur naturally in its metallic state |
| Silica | SiO2 | Sand, marble, or quartz |
| Silicate | Na2SiO3 | In one form, used as a desiccant (e.g., in anesthesia machines) |
| Siloxane | R2SiO | Monomer of silicon and oxygen |
| Silicone | |R2SiO|n | Polymers of silicon and oxygen |
| Poly-dimethylsiloxane | |(CH3)2SiO|n | The building block for most medical-grade silicone products, including breast implants |
(Adapted from Miller MJ, Ogunleye OT. Biomaterials. In: Guyuron B, Eriksson E, Persing JA, et al., eds. Plastic surgery indications and practice. New York: Saunders Elsevier; 2009:57–66.)
Silicones are also found in some medications. If a medication contains an ingredient with the name “methicone” (e.g., simethicone), this is a silicone that has been modified for human consumption. Silicones are also used in household items such as lipstick, suntan/hand lotion, hairspray, processed foods, and chewing gum. Medical-grade silicones invoke a nonspecific foreign-body response, resulting in typical macrophage invasion, giant cell formation, and eventual scarring.16
Extensive investigations by several prestigious scientific bodies (e.g., the IOM,17,18 and the UK Department of Health19) have failed to show that systemic illness is definitively attributed to silicones.
Polytetrafluoroethylene
Polytetrafluoroethylene (PTFE), also known as Teflon, was accidentally invented by Roy Plunkett in 1938 while he was trying to develop a refrigerant.20 It consists of a carbon backbone with fluorine side chains. Expanded PTFE (ePTFE or Gore-Tex®
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree