Immediate and Delayed Breast Reconstruction with Shaped Adjustable Implants
Michael Scheflan
Although some surgeons perform breast reconstruction with a tissue expander as the first and final implant choice for a second procedure, during the past 12 years, I have used an adjustable shaped implant as the final and permanent implant in most immediate and delayed breast reconstructions (1,2,3,4,5,6,7,8). I have also been using the same implant for surgical management of developmental breast asymmetries (9,10,11). This permanent anatomic shaped adjustable (McGhan style 150) implant is a “soft” expander. Although unable to stretch thick, indurated, and nonelastic chest walls (in which case I use a tissue expander), it is effective in stretching soft, elastic, and supple tissues, achieving volume and soft-tissue envelope symmetry in almost all breast reconstructions following mastectomy, including patients following radiotherapy (12,13). This approach is effective in reconstructions following skin-sparing and modified radical mastectomies in immediate and delayed settings (14).
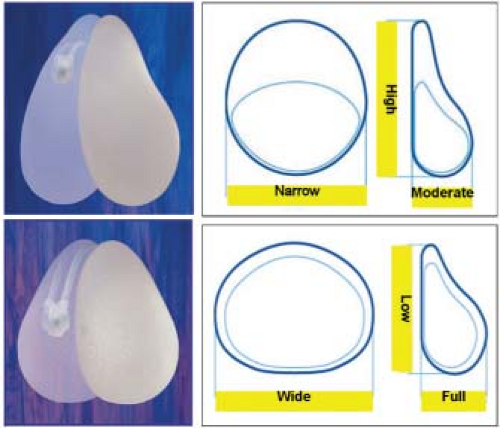
The device is an anatomic, half pear-shaped implant with 30% highly cohesive silicone gel in the outer envelope and 70% saline in the inner chamber, adjustable through a permanent filling tube attached to a small remote valve (Fig. 31.1). If at the end of the reconstructive project the valve proves objectionable to the patient, it maybe removed under local anesthesia, and the filling tube shortened and “corked” with a solid silicone plug (McGhan fill tube plug kit).
In general, I prefer to leave the port in place permanently because it helps manage an occasional capsule contracture or subtle volume adjustments. Nipple-areola reconstruction is usually performed at a second stage, under local anesthesia (15). Some patients require a secondary procedure for shape adjustments, such as enhancing the fold or adjusting the envelope or lipostructure of the upper pole of the breast. This is sometimes necessary to obtain a natural, oblique breast slope and a soft, gradual transmission from chest wall to breast (Figs. 31.2A–C and 31.3).
Planning the Reconstruction
The width of the base of the breast to be reconstructed and the desired height of the breast are easy to determine at the outset. This is accomplished by measuring the breast, the other breast (with or without its planned modification), and chest wall characteristics. The final volume of the future breast and the soft-tissue “yield” and reaction to any implant/expander device are unpredictable. It makes sense, therefore, whenever possible, to place a final adjustable implant in the first procedure, by determining width and height first and final volume later (16). Base width, breast height, and approximated desired projection and volumes can often be decided when planning the surgery. Skin expansion, overexpansion, and final volume may be reached with incremental weekly or biweekly injections of sterile saline through the remote port.
Shaped adjustable implant choices vary between two basic designs: (a) short height, wide base, and full projection; and (b) full height, narrow base, and moderate projection. Seven different sizes are available for each style (Fig. 31.4). The final volume should approximate the saline fill range recommended by the manufacturer. Overfill will result in “scalloping,” whereas underfill may cause rippling (17). Before proceeding with nipple-areola reconstruction in the second stage, the surgeon should assess and examine his or her patient with the following questions in mind: Does it look like a breast? Does it look like the other breast? Are volumes, shapes, and slopes comparable? Are widths and heights comparable? Are the inframammary folds at the same level and depth? Are the soft-tissue envelopes adequate? Is the implant visible? If additional steps are indicated, they should be taken prior to nipple reconstruction or at the same procedure, providing the surgeon can determine nipple location while changing the other parameters simultaneously.
Surgical Considerations in Immediate Breast Reconstructions
The surgeon should plan the location, orientation, and length of the incision together with the general surgeon, following oncologic and surgical principles (18,19). The necessity to excise the nipple-areola complex, often together with the biopsy scar and enblock with the breast, presents a unique challenge, as well as an opportunity, to the reconstructive surgeon (20) (Figs. 31.5A–C).
A variety of options is available to determine the mode of excision, which requires judgment, creativity, and “imagineering.” Whenever possible, however, a version of an oblique excision is preferred because it maintains breast shape best and places a scar in the upper outer quadrant of the reconstructed breast. Following mastectomy, the pectoralis muscle is detached from its origins inferiorly and partially released from the low sternal origins to allow forward and upward displacement of the muscle. Laterally, a pectoralis minor/serratus flap is elevated to accommodate the desired base width of the implant. The lateral pectoral muscle edge is sutured with a running suture to the medial edge of the serratus muscle flap. The anatomic adjustable implant is placed with its two upper thirds covered with muscle and its lower third subcutaneously.
The filling port is positioned subcutaneously at the mid- or posterior axillary line, and the inner chamber is gradually filled to allow closure without tension (Figs. 31.6 and 31.7). When the lower mastectomy skin flap is draped over the implant, the muscle may be anchored to the undersurface of the flap, using marionette sutures looping from skin through the muscle and back through the skin, and secured untied with a fine transparent tape to the skin (Tagaderm, 3M Healthcare). There should always, whenever possible, be muscle between the implant and the skin underneath the closure. This way any minor delays in wound healing, stitch granulomas, wound edge necrosis, or local infection remain distant from the implant.
This dual plain placement of the implant follows aesthetic principles of breast augmentation of partial retromuscular and partial premuscular sites. These guidelines are even more critical in breast reconstructions. Two-thirds upper pole muscle coverage provides padding of the upper pole of the implant and a soft transition from chest wall to implant, as well as a well-vascularized protective barrier between the incision and the implant. Subcutaneous lower pole placement enhances projection, roundness, and fold definition. In immediate reconstructions of large-breasted patients, the skin-sparing mastectomy is undertaken through an inverted “T” breast reduction pattern (21). The skin at the inframammary fold between the legs of the Wise pattern is de-epithelialized, separated from the breast tissues, and hinged on the inframamary fold. During closure, this flap is draped over the lower center pole of the implant and sutured to the free edge of the pectoralis muscle as an additional support layer under the skin closure (Figs. 31.8 and 31.9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree