Introduction
The imaging support of hidradenitis suppurativa (HS) has been increasing in the last decade due to the development of high-axial-resolution devices that can detect simultaneously and with high definition abnormalities of the skin and deeper layers. Nowadays, the spatial axial resolution, which allows the discrimination of two adjacent reflector points, is much higher on ultrasound than MRI or CT. It should be kept in mind that the type of treatment in HS is decided according to the severity stage ; therefore, an accurate diagnosis and scoring of the severity of the HS patients’ are critical for their management. To date, multiple reports from different groups, countries, and racial backgrounds confirm the clinical underestimation of the severity of the disease and the lack of good inter-rater correlations of the clinical parameters. The objectives of using HS imaging are to detect early the disease and adequately score the severity and activity, guide percutaneous and surgical procedures, and monitor the treatment.
Essential Concepts on Imaging in Dermatology
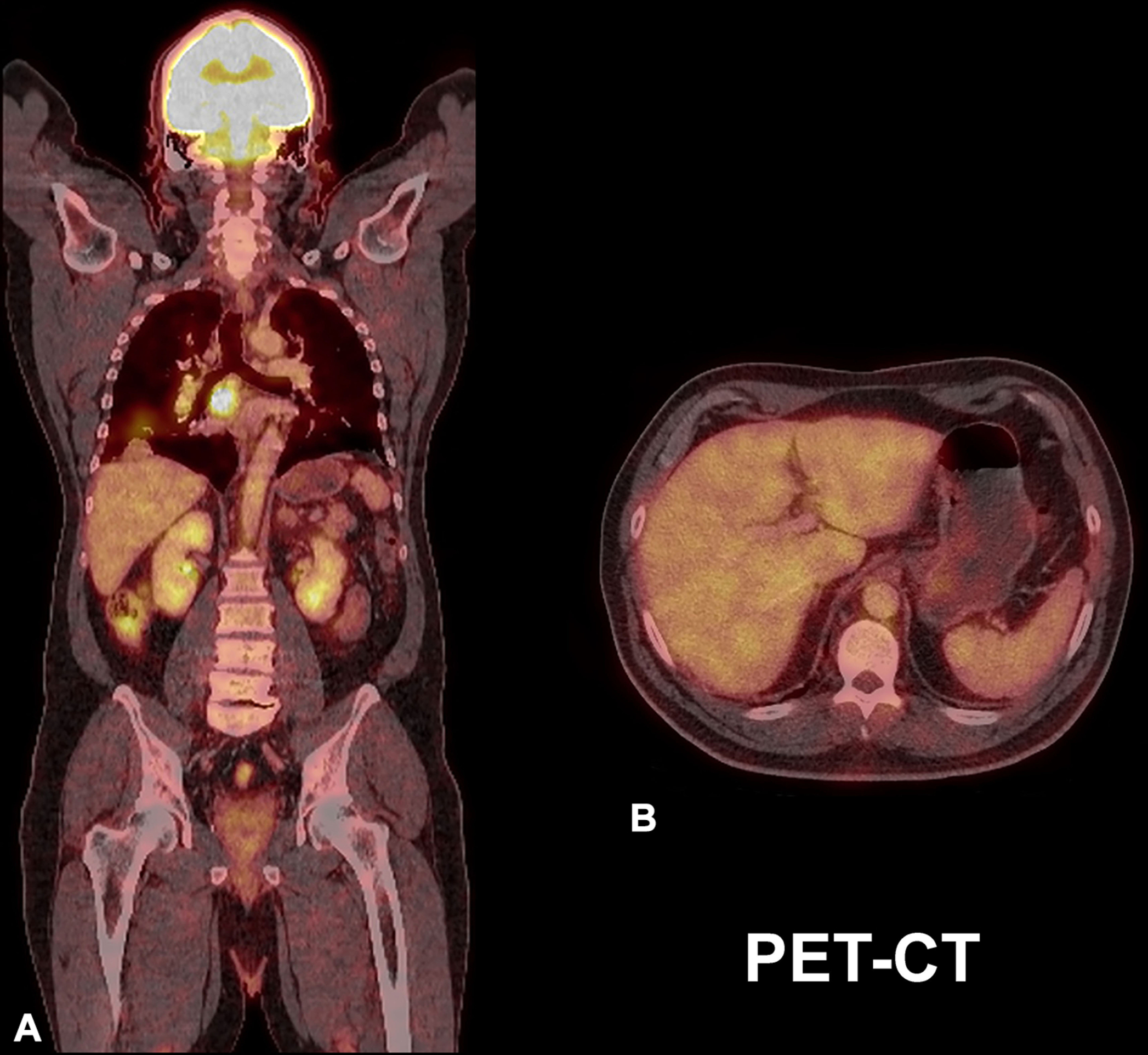
Significant advances in HS have been made with ultrasound, which provides a significantly higher number of publications than the rest of the imaging techniques. Particularly in dermatology, ultrasound has followed the validation sequence of any imaging modality and has been suggested as a standard of care for HS patients. This process includes the description of the accuracy of the method, the standardization of the image acquisition process, the reference of normal patterns and values, the qualification and quantification of abnormalities, the design of the forms used for reporting the examinations, a description of the limits of the detection, and the assessment of multicentric reproducibility.
Moreover, the guidelines for performing dermatologic ultrasound examinations have defined the need for adequate and updated machines as well as trained operators.
The axial spatial resolution of ultrasound can vary from 100 microns at 15 MHz to 30 microns at 70 MHz, which means that ultrasonographically, it is possible to detect submillimetric changes that can be as small as 0.1 mm at 15 MHz and 0.03 mm at 70 MHz. Furthermore, there are ultrasonographic criteria for diagnosing HS, and a sonographic scoring system of HS (SOS-HS) has been reported.
To date, magnetic resonance imaging (MRI) has been mainly used to detect the perianal fistulous tracts and subcutaneous or more profound inflammatory signs in HS. However, considering the commercially available devices, MRI still presents a lower axial spatial resolution than ultrasound. This resolution can go up to 500 microns using 1.5 Tesla and up to 100 microns only in experimental machines of 7 Tesla. The latter features mean that on MRI, the abnormalities of the skin or superficial layers that measure less than 3 mm may be challenging to discriminate. Moreover, to date, there are no reports on specific patterns of HS on MRI.
Regarding the discrimination between HS and Crohn’s disease, the MRI characteristics rely mostly on clinical findings such as the intertriginous location and bilateral involvement of the inflammatory HS lesions. Nevertheless, it should be remembered that these two conditions can be concurrent. Another relevant difference between ultrasound and MRI is that ultrasonography does not usually require contrast media. In contrast, MRI frequently requires the intravenous injection of contrast media (gadolinium), which is potentially nephrotoxic and may rarely generate nephrogenic systemic fibrosis.
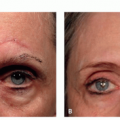
Ultrasound can detect submillimeter subclinical alterations in HS and characterize the blood flow, including type (arterial or venous) and velocity of the vessels noninvasively through color Doppler. The detection of vascularity patterns allows monitoring the degree of inflammation in HS; therefore, it can support activity level discrimination. Furthermore, ultrasound is considered a safe and non-radiating imaging technique that is commonly used in pregnant women ( Fig. 6.1 ).
Medical infrared thermography (MIT) has also been used in HS to detect inflammation; however, it lacks anatomical details. Nevertheless, it may be useful to detect gross data if other imaging modalities are not available.
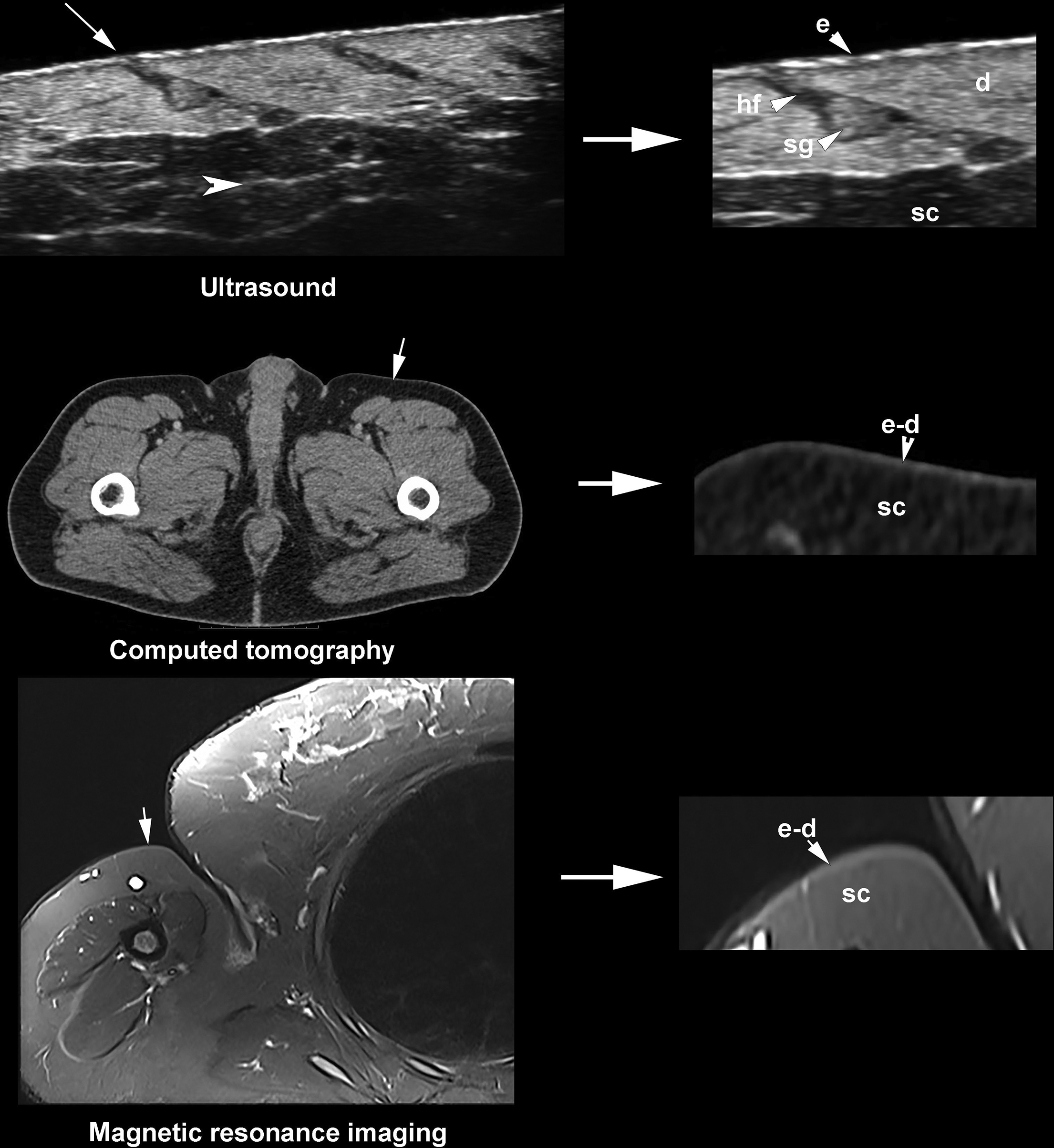
The usefulness of other imaging modalities in HS, such as computed tomography (CT), PET-CT (positron emission tomography-CT), optical coherence tomography (OCT), or confocal microscopy (CFM), is uncertain because, to date, there are no specific reports about their clinical use in HS. CT provides a lower definition for superficial layers in comparison with MRI and ultrasound; therefore, its use is not recommended for diagnosing or monitoring HS. However, abdominal CTs can be helpful in cases with concomitant inflammatory bowel diseases. In the case of Crohn’s disease or ulcerative colitis, CT may help assess the degree of bowel inflammation and rule out the presence of communicating fistulas between the abdominal cavity and wall.
Regarding PET-CT, care must be taken in the interpretation of the inflammatory signs in HS patients with a concomitant history of cancer because they can be mistaken for malignant infiltration ( Fig. 6.2 ).
Some reviews hypothesize about the potential use of CFM or OCT to detect epidermal alterations in HS; however, there are no specific HS studies available to date in the literature. These imaging techniques present very high axial spatial resolution, but their penetration is extremely low and goes up to 150 to 200 microns in CFM and 1.5 to 2 mm in OCT. This significantly limits the applications of these techniques to only the detection of epidermal or upper dermal changes. Hence, to date, neither CFM nor OCT has reported supporting the diagnosis or staging of HS.
Importantly, as in any medical procedure, all the imaging techniques need adequate machines and trained operators with proper levels of annual competence. The lack of these conditions may influence the medical decisions of requesting imaging examinations. A strong encouragement for operators’ training or good coordination with the imaging facilities that already have the machines and operators can help overcome this problem.
In the following sections, we will further review the details of the main indications, advantages, and disadvantages of imaging modalities in HS following a practical approach.
Basic Physics Concepts of Imaging Techniques
This section focuses on the most commonly used imaging techniques in HS.
Ultrasound
Ultrasound imaging is based on the reflection of sound waves from an interface due to differences in acoustic impedances. The transducer, also called a probe, transmits sound waves into the tissue and collects the reflected sound waves. The color Doppler ultrasound application allows observation of blood flow in real-time.
In dermatologic ultrasound examinations, multifrequency transducers are preferred. These have a wide range of operating frequencies within the same probe and users may adjust the frequency to get adequate penetration depth based on the layer being imaged. In dermatologic studies, the recommendation is to use linear or compact linear probes with higher ranges of frequencies ≥ 15 MHz. With improved technology, transducers with frequencies as high as 70 MHz are available for ultrasound imaging.
The color Doppler application allows discriminating the type of vessel (arterial or venous) and the peak systolic velocity of the arterial flow (cm/s) within a user-defined area. The color Doppler maps display the vessels in different colors on the screen, but the most frequent display is the one that uses red and blue. Importantly, these colors reveal the direction of the flow and don´t mean arterial and venous vessels, respectively.
In the standard configuration, the red color usually depicts flow towards the probe, and the blue color shows the flow away from the transducer. However, these settings are user-defined, and the operator may invert them. Thus, the demonstration of the spectral curve analysis of the vessels is relevant for the discrimination. The arterial flow presents a systolic and diastolic curve, and the venous flow shows a monophasic flow.
The power Doppler application is a monodirectional display of the vascularity that is usually more sensitive for detecting slow flow. Besides, several echoangio applications that subtract the tissues and present only the screen’s vascularity are available in several models of ultrasound units.
Magnetic Resonance Imaging
Protons within the nuclei of hydrogen atoms are essential to the formation of MRI signals and are present in fat and water molecules within the human body. These protons spin and induce a small magnetic field, resulting in a zero net magnetic field due to the random orientation. However, in the presence of a strong magnetic field, within an MRI system, there is non-zero net magnetization due to change in alignment. This net magnetization generates signals resulting in MRI images. The images are created by the excitation of individual atomic nuclei under radiofrequency (RF) and a strong magnetic field.
RF energy is transmitted by a coil located in the site of examination of the patient. RF pulse’s strength and duration determine the amount of rotation of the net magnetization from the main magnetic field’s direction. Information regarding relaxation after an RF pulse composes different sequences such as T1 (longitudinal) and T2 (transverse), which help in the generation of T1 or T2 weighted images that show different features for the tissues. , The typical clinical MR systems have a magnetic field strength between 0.5 T and 3.0 T (T, tesla units). Importantly, due to these potent magnets, several medical devices prevent the use of MRI, such as pacemakers and metal prostheses.
Computed Tomography and Positron Emission Tomography
CT is a radiating cross-sectional technique, where the image is produced by several x-rays devices that rotate in a ring that surrounds the patient. Nowadays, fast multislice CT machines take seconds to perform the corporal segment’s sweep or the whole body. CT is beneficial for detecting thoracoabdominal and bone pathologies.
PET is a nuclear imaging technique that is commonly fused with CT. The fusion of techniques is called PET-CT and allows the detection of anatomical and metabolic functional abnormalities. PET and PET-CT need an intravenous contrast called FDG (F-18 Fluorodeoxyglucose) which distinguishes the hypermetabolism of malignant and inflammatory conditions, named “hot spots.”
Medical Infrared Thermography
MIT is based on detecting infrared radiation emitted by an object, which is transformed into an electronic signal. The intensity of the infrared radiation generated by objects is mainly a function of its temperature; therefore, radiated energy changes represent variations in temperature within a region of interest. MIT displays in colors the temperature variations. Usually, warmer temperatures are shown in bright colors (yellow to orange), while lower temperatures are shown in darker colors (red to blue). Higher temperatures are supposedly due to increased metabolism; for example, in inflammation.
Other Potential Imaging Techniques
CFM, also called reflectance confocal microscopy (RCM) or in vivo RCM, uses near-infrared light at 830 nm. The technique generates high-resolution images utilizing intrinsic differences in cellular structures’ refractive indices, primarily melanin, collagen, and keratin. This imaging technique shows a cellular resolution of the epidermis and displays the tissue in a horizontal view. Due to limitation of penetration depth, only epidermis and superficial papillary dermis can be imaged.
OCT uses infrared light from an 830 nm superluminescence diode coupled into an optical fiber interferometer. This technique allows us to observe the epidermis and upper dermis at a high axial resolution but lower than CFM. New applications of OCT allow detecting the dermal blood flow.
Imaging of Hidradenitis Suppurativa
Ultrasound Advantages and Disadvantages in Hidradenitis Suppurativa
Among the main advantages of using ultrasound in HS are that it allows early detection of the disease, stage of severity, assessing the degree of activity, and monitoring the treatment. The widely reported discordance between clinical and ultrasonographic evaluations supports the performance of a basal ultrasound examination in every HS patient and (not only for the pre-surgical planning, severe, or obese cases).
The limitations of ultrasound vary according to the range of frequencies of the probes; however, to date, it is impossible to detect pigments (e.g., melanin), despite the frequency. The limitation of probes with a higher range of frequency up to 15 to 24 MHz includes detecting only-epidermal alterations and lesions the measure ≤ 0.1 mm. The probes with a higher range of frequency up to 50 to 70 MHz present as a limitation the discrimination of abnormalities that measure ≤ 0.03 mm.
Ultrasound, like any other medical technique or procedure, needs to follow guidelines for standardizing the performance of the examinations and training of the operators. Nowadays, ultrasonographic training is available under the umbrella of international scientific societies. These societies include the American Institute of Ultrasound in Medicine (AIUM; www.aium.org ) and the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB; www.efsumb.org ). The literature on this topic is growing.
Other disadvantages of ultrasound include the impossibility of recording a whole corporal segment or the whole body in one view, such as in MRI. Since the sound waves’ passage is stopped at the bony cortex, it is impossible to fully observe the bone medulla. Nevertheless, these limitations are not relevant to detect the soft tissue abnormalities of HS.
Definition of Early and Late Ultrasonographic Subclinical HS Lesions
Depending on the ultrasound frequency, it is possible to detect early (submillimetric) and late alterations of HS patients’ dermis and subcutis.
Early Ultrasonographic Subclinical Hidradenitis Suppurativa Lesions
For detecting early subclinical and submillimetric abnormalities, it is necessary to have ultrasound devices that work with multifrequency probes that present their upper ranges ≥ 50 MHz, which may not be widely available. However, if these ultrasound machines are available, they will allow detection of the following early signs ( Figs. 6.3 to 6.5 ) :
- 1.
Modification of the axis of the hair follicle from straight (slightly oblique) to curved
- 2.
Thickening of the hair follicles and tracts
- 3.
Ballooning of the hair follicles
- 4.
Donor Sign: Dilated hair follicles that donate their keratinous content to fluid collections and tunnels.
- 5.
Sword Sign: Fragments of hair tracts going from the cavity of a dilated hair follicle to the surrounding dermis.
- 6.
Bridge Sign: Communications between adjacent and curved hair follicles. These connections may be conformed by single or multiple bridges between neighboring hair follicles.
- 7.
Two types of fragmentations of the keratin are multifragment and cylindrical. Multifragment is the presence of multiple small fragments of hyperechoic linear fragments within the dilated hair follicles, fluid collections, or tunnels. The cylindrical type is composed of hypoechoic thick bands within the same structures that sometimes may show hyperechoic borders.
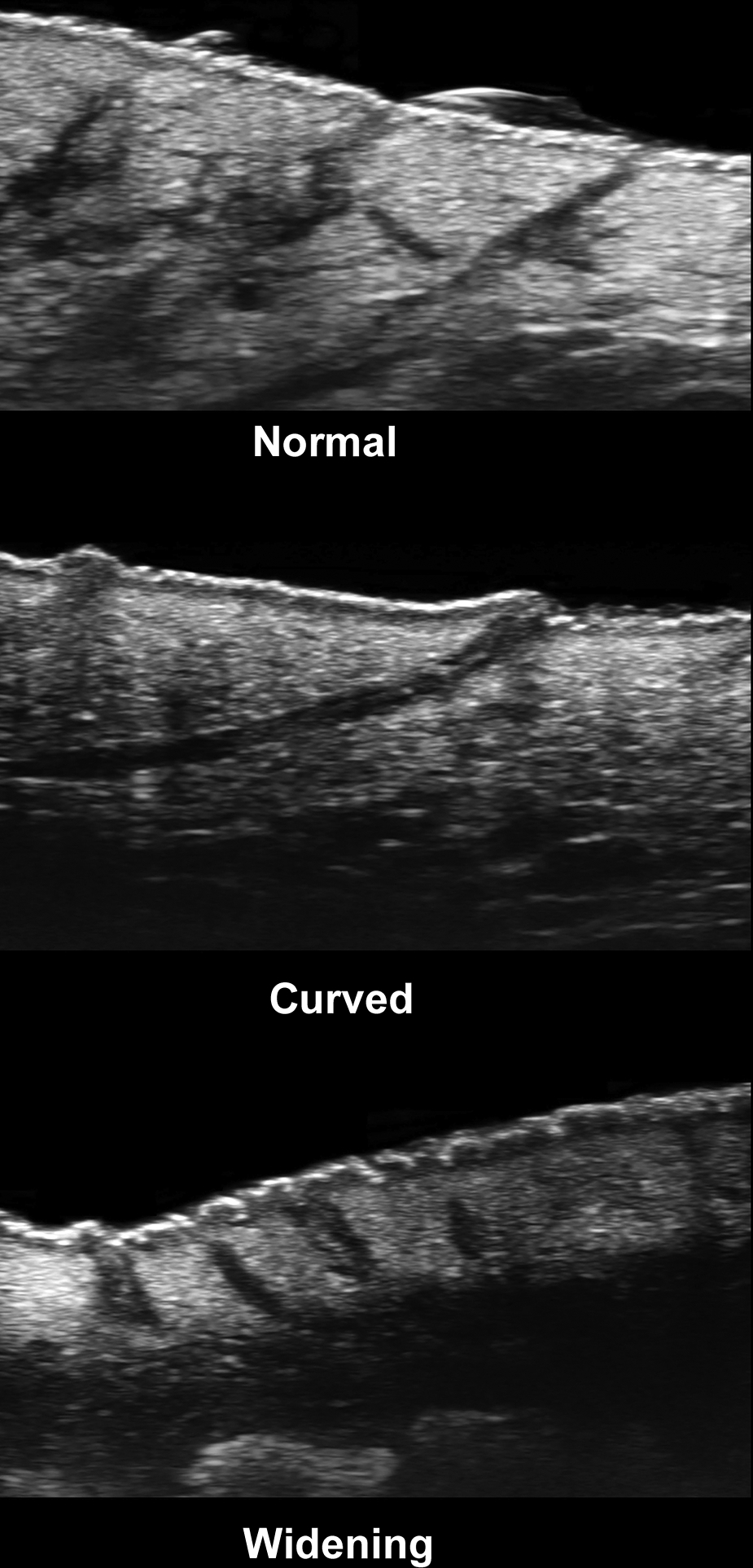

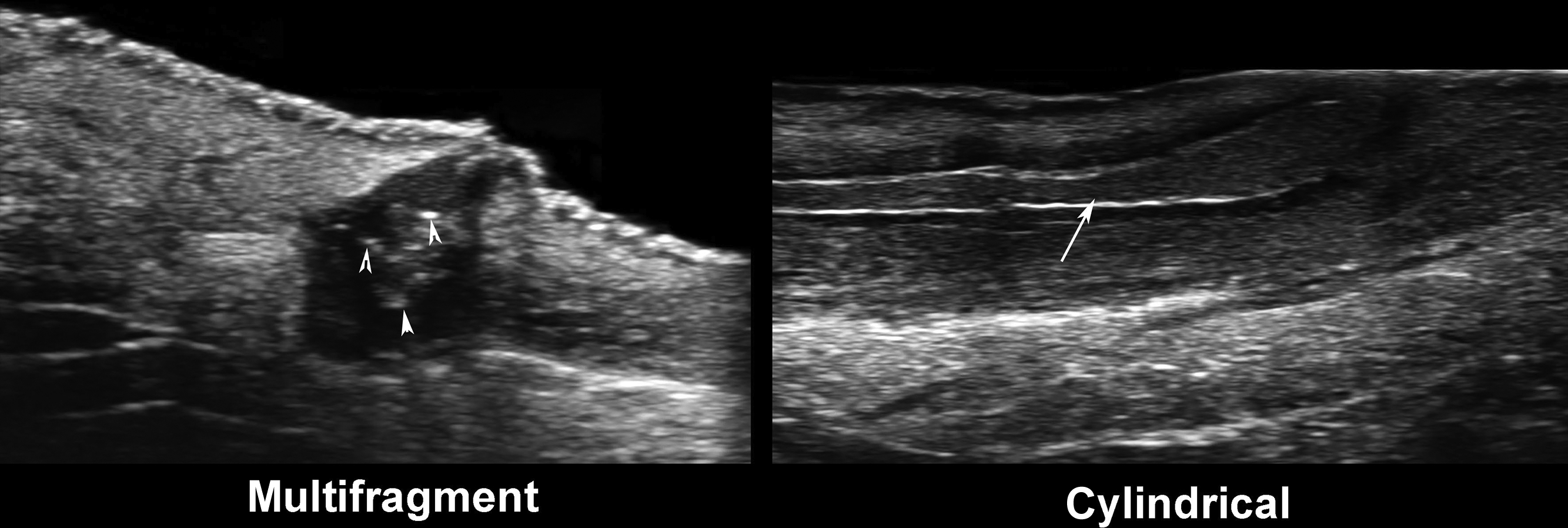
The signs significantly associated with the disease’s severity are the presence of “bridge” and “sword” signs and the cylindrical type of keratin fragmentation. Thus, tunnels and fibrotic changes are more frequent in these cases. The rest of the ultrasonographic signs may explain the initial formation of the primary clinical lesions.
Late Ultrasonographic Subclinical Hidradenitis Suppurativa Lesions
To detect late subclinical HS lesions, it is necessary to scan the patients with color Doppler ultrasound devices working with multifrequency probes that present an upper range of 15 to 24 MHz. a
a References: 2, 5, 6, 8, 11, 12, 18, 20, 21, 23, 24.
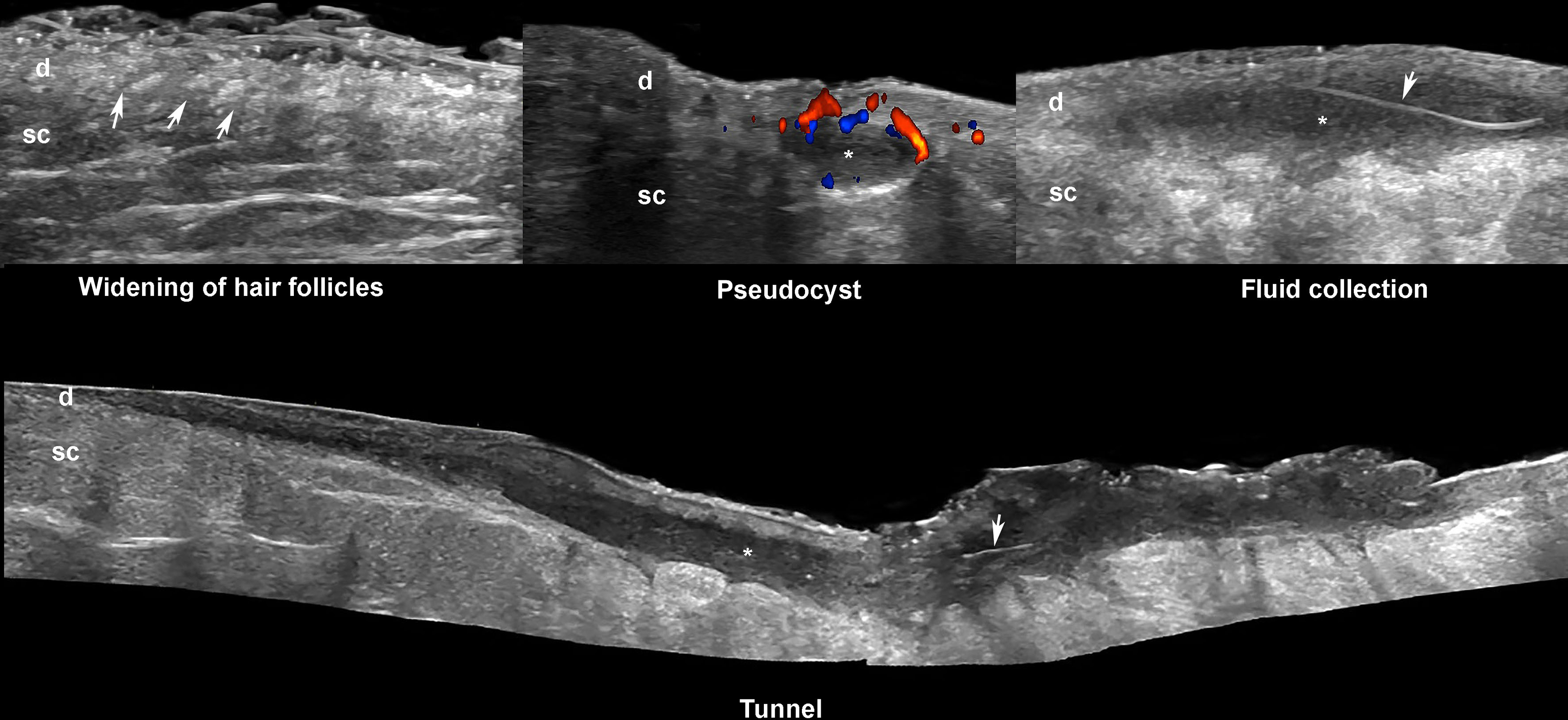
These devices are widely available and allow detection of subclinical lesions, scoring the severity of the disease, and the evaluation of the degree of inflammatory activity, besides other anatomical details.These key ultrasonographic signs are ( Fig. 6.6 ) b :
b References: 2, 5, 6, 8, 11, 20, 21, 23, 24.
- 1.
Dilation of hair follicles
- 2.
Increased thickness and decreased echogenicity of the dermis
- 3.
Pseudocysts (i.e., round or oval-shaped anechoic or hypoechoic dermal and/or hypodermal nodule < 1 cm)
- 4.
Fluid collections (i.e., anechoic or hypoechoic sac-like dermal and/or hypodermal structures ≥ 1 cm connected to the base of dilated hair follicles)
- 5.
Tunnels, also called fistulous tracts (i.e., anechoic or hypoechoic band-like dermal or hypodermal structures connected to the bottom of dilated hair follicles), which can be communicated between them or not.
Ultrasound Diagnostic Criteria of Hidradenitis Suppurativa
The diagnostic criteria of HS are the presence of three or more key lesions. The translation of clinical lesions such as nodules, abscesses, or fistulas into pseudocysts, fluid collections, or tunnels may be inexact because imaging lesions are three-dimensional anatomical structures that may not correlate with the palpable lesions. For example, an inflammatory nodule may appear as a tunnel on ultrasound.
Ultrasound Staging of Hidradenitis Suppurativa
The sonographic staging of HS may be used separately or associated with a clinical scoring system. The ultrasonographic staging, called SOS-HS, which means sonographic scoring of HS and reminds the acronym of help, defines three levels of severity that try to parallel with the Hurley clinical classification. These levels of severity are characterized as follows and shown in Table 6.1 .
| Stage | Description |
|---|---|
| I | Single fluid collection and dermal changes (hypoechoic or anechoic pseudocystic nodules, widening of the hair follicles, alterations in the dermal thickness or echogenicity) affecting a single body segment (e.g., axilla, groin, breast, buttock) (uni- or bilateral) without fistulous tracts |
| II | Two to four fluid collections or a single fistulous tract with dermal changes affecting up to two body segments (uni- or bilateral) |
| III | Five or more fluid collections or two or more fistulous tracts with dermal changes or involvement of three or more body segments (uni- or bilateral) |
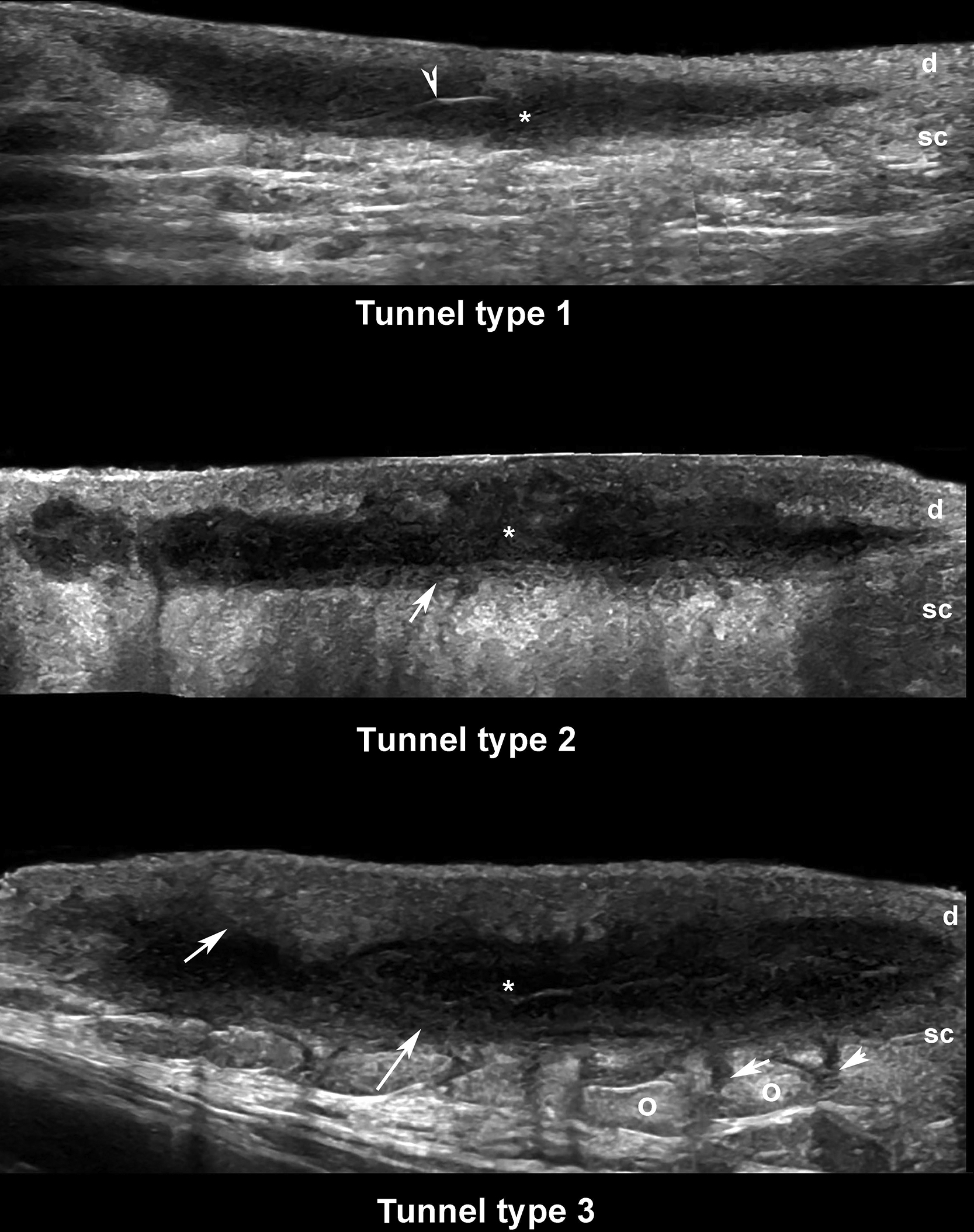
Ultrasound Classification of Hidradenitis Suppurativa Tunnels
The level of subcutaneous edema and fibrosis surrounding the fistulous tracts may support the discrimination of good and bad responders to the medical treatment. Thus, fibrosis’s high presence surrounding the tunnels may imply a lower response to systemic medical therapy.
The surrounding subcutaneous edema to the tunnels can be categorized as 22 :
0-absent
1-diffuse hyperechogenicity of the subcutis surrounding the tunnels
2-diffuse hyperechogenicity of the subcutis and anechoic or hypoechoic fluid in between the fatty lobules
The fibrosis surrounding the tunnels can be categorized as 22 :
0-absent
1-Thin hypoechoic laminar band surrounding the tunnel
2-Thick hypoechoic laminar band surrounding the tunnel that may conform a “halo sign” in transverse view (cross-sectional view)
The tunnels’ main classification is based on the degree of edema, and fibrosis is shown in Table 6.2 ( Fig. 6.7 ). There is another classification of the tunnels according to the layer of involvement that divides the tunnels into four types: dermal fistula (Type A), dermo-epidermal fistula (Type B), complex fistula (Type C), and subcutaneous fistula (Type D). Fistulas Type A and B tend to show a complete resolution after 6 months of different medical therapies in up to 95% and 65% of cases, respectively. Conversely, fistulas Type C and D have been reported to present no significant response after a medical intervention. Moreover, ultrasonography has been demonstrated to predict early fistulization in comparison with the Hurley staging.
| Type | Definition |
|---|---|
| 1 | Low fibrotic scarring (grades 0-1) with high or low edema (grades 0-2) |
| 2 | High fibrotic scarring (grade 2) with low edema (grades 0-1) |
| 3 | High fibrotic scarring (grade 2) with high edema (grade 2) |