67
Human Herpesviruses
General
Herpes Simplex Viruses (HSV-1/HHV-1 and HSV-2/HHV-2)
• Ubiquitous pathogens that produce primarily orolabial (HSV-1 > HSV-2) and genital infections (HSV-2 > HSV-1) characterized by recurrent vesicular eruptions (Table 67.1).
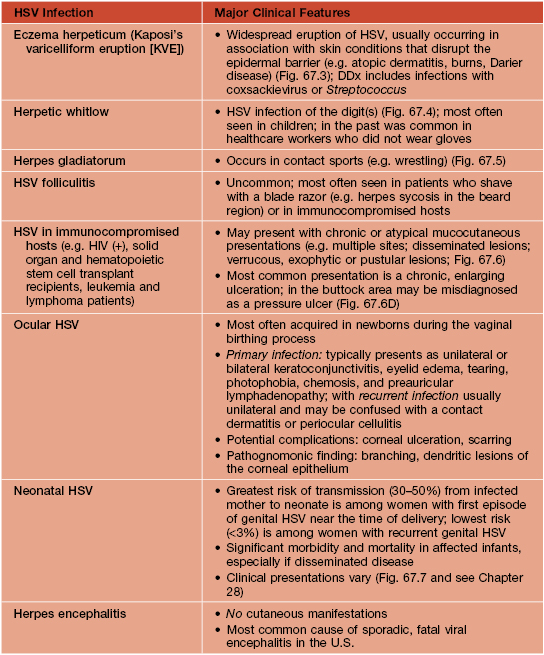
Table 67.1
Major clinical features of classic herpes simplex virus (HSV) orolabial and genital infections.
~90% of U.S. adults are seropositive for HSV-1 and ~25–30% are seropositive for HSV-2, with an increasing seroprevalence for the latter. Treatment is outlined in Table 67.3.
* For the description of typical lesions, see text; occasionally, intact vesicles are not seen but rather grouped ulcerations with hemorrhagic crusts predominate.
EM, erythema multiforme; SJS, Stevens–Johnson syndrome; DFA, direct fluorescent antibody; H&E, hematoxylin and eosin.
• Transmission can occur during both symptomatic and asymptomatic periods of viral shedding.
• A wide range of clinical presentations exist, with asymptomatic infection being the most common.
– Initial lesions: small round vesicles on an erythematous base; often painful or burning; the grouping of these vesicles is a clue to the diagnosis; vesicles may become umbilicated or pustular, followed by erosions or ulcerations with hemorrhagic crusts, often with a scalloped border; lesions resolve over 2–6 weeks (Fig. 67.1).



Fig. 67.1 Primary herpes simplex virus (HSV) infections. A Primary herpes gingivostomatitis due to HSV-1 in a child. Note the coalescing lesions with scalloped borders. B HSV-2 infection in a teenager (primary vs. non-primary initial infection). Note the scalloped borders. C Primary genital HSV infection. In addition to 1- to 2-mm hemorrhagic crusts, there are perifollicular vesicopustules. A, Courtesy, Julie V. Schaffer, MD; B, Courtesy, Jean L. Bolognia, MD; C, Courtesy, Stephen K. Tyring, MD.
– Localized prodrome of dysesthesia (e.g. burning/tingling, pain, pruritus) and tenderness.
– Mucocutaneous lesions similar as in primary but fewer in number, less severe, and shorter duration (Fig. 67.2).




Fig. 67.2 Reactivation of herpes simplex virus (HSV) infections. A Recurrent HSV-1 infection on the cheek. Occasionally such lesions are misdiagnosed as cellulitis or bullous impetigo. B Intact grouped vesicles on the penis. Note the genital wart at the base of the penis. C Grouped vesiculopustules on the buttock, a common location in women. D Healing ulcerations with scalloped borders on the penis. A, Courtesy, Kalman Watsky, MD; B, C, Courtesy, Louis A. Fragola, Jr., MD; D, Courtesy, Joseph L. Jorizzo, MD.
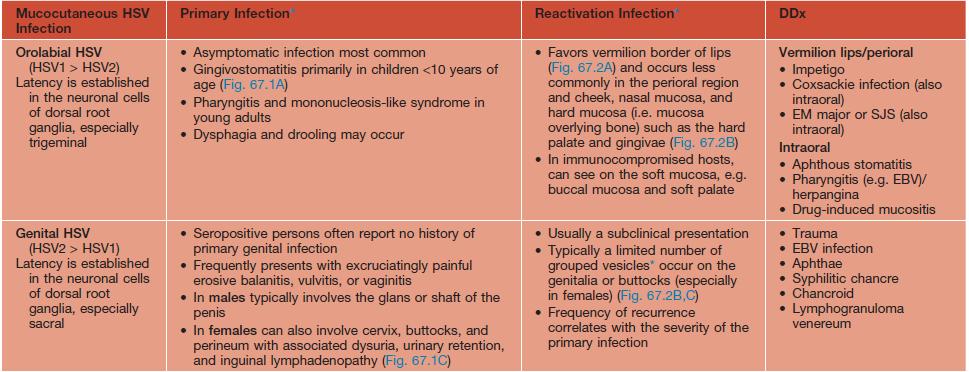
• In addition to the classic orolabial and genital infections, HSV can cause other infections (Table 67.2; Figs. 67.3–67.7).




Fig. 67.6 Herpes simplex viral infections in immunocompromised hosts. A Enlarging ulcerations in a child with acute lymphocytic leukemia who was presumed to have a Rhizopus infection, and (B) in a young man with AIDS. C Coalescence of eroded, yellow-white papules and plaques on the tongue. D Chronic perianal ulcerations in an HIV-infected male. D, From Callen JP, Jorizzo JL, et al. Dermatological Signs of Internal Disease, 4th edn.; Saunders/Elsevier, 2009.
• DDx and Dx: see Table 67.1 and Fig. 67.8.