Histology
It is useful to understand the histology of normal and pathologic veins and venous valves because the structure of the vein determines its normal mode of function as well as its common modes of failure. It is also important to understand the zones that must be injured in order to permit sclerosis and closure of veins.
 VEIN WALLS
VEIN WALLS
Collection of venous blood begins with the end-capillary venule, which is about 20 microns in diameter and consists of an endothelium surrounded by a thin layer of collagenous fibers. As it carries blood proximally, the venule increases in diameter and gains smooth muscle cells within the fibrous sheath. At a diameter of 200 μm, the muscular layer becomes better defined, and by the time the vessel is large enough to be clinically visible, three distinct layers can be recognized. This is the case for venules on the leg that comprise telangiectatic webs. As veins become larger, they include elastic fibers and demonstrate a more organized structure with three tunicas: intima, media, and adventitia (Figure 3-1).
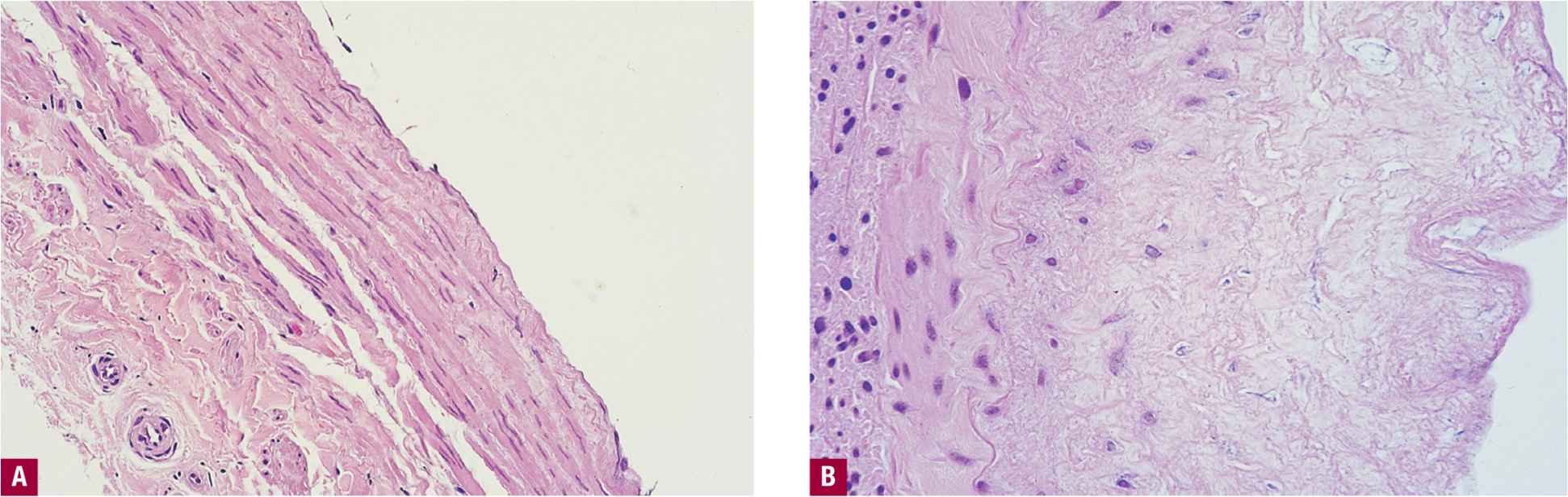
![]() FIGURE 3-1 Cross section of adult normal vein. A. Note three distinct layers of intima (facing right), media, and adventitia (H&E 200X). B. Same vein after in vivo exposure to 3 percent sodium tetradecyl sulfate for 10 min. Note marked destruction of media with necrosis of smooth muscle cells.
FIGURE 3-1 Cross section of adult normal vein. A. Note three distinct layers of intima (facing right), media, and adventitia (H&E 200X). B. Same vein after in vivo exposure to 3 percent sodium tetradecyl sulfate for 10 min. Note marked destruction of media with necrosis of smooth muscle cells.
In its relaxed state, the normal vein contains an “intrinsic rest volume” and is slightly oval or elliptical in cross section, with the short axis perpendicular to the skin. When the volume of blood increases, the vein accommodates additional volume by becoming circular in cross section, increasing its volume without significantly increasing the intravascular pressure (Figure 3-2). This contributes to the large intrinsic capacitance of the venous system.1 When further volume needs to be accommodated, the vessel stretches and the pressure rises according to the tension developed in the muscular, elastic, and fibrous tissues of the vein wall. Prolonged exposure to high pressures causes the vein to increase its intrinsic rest volume by permanently increasing its length and diameter, becoming dilated and tortuous and often following a spiral path. Varicose saphenous veins have been shown to have significantly larger wall areas and higher amounts of collagen. Collagen content and wall area are larger proximally compared to distally in both control and varicose veins, with a higher content of smooth muscle and elastin in varicose veins (Table 3-1).2 Varicosis is therefore thought to be a dynamic response to venous hypertension.
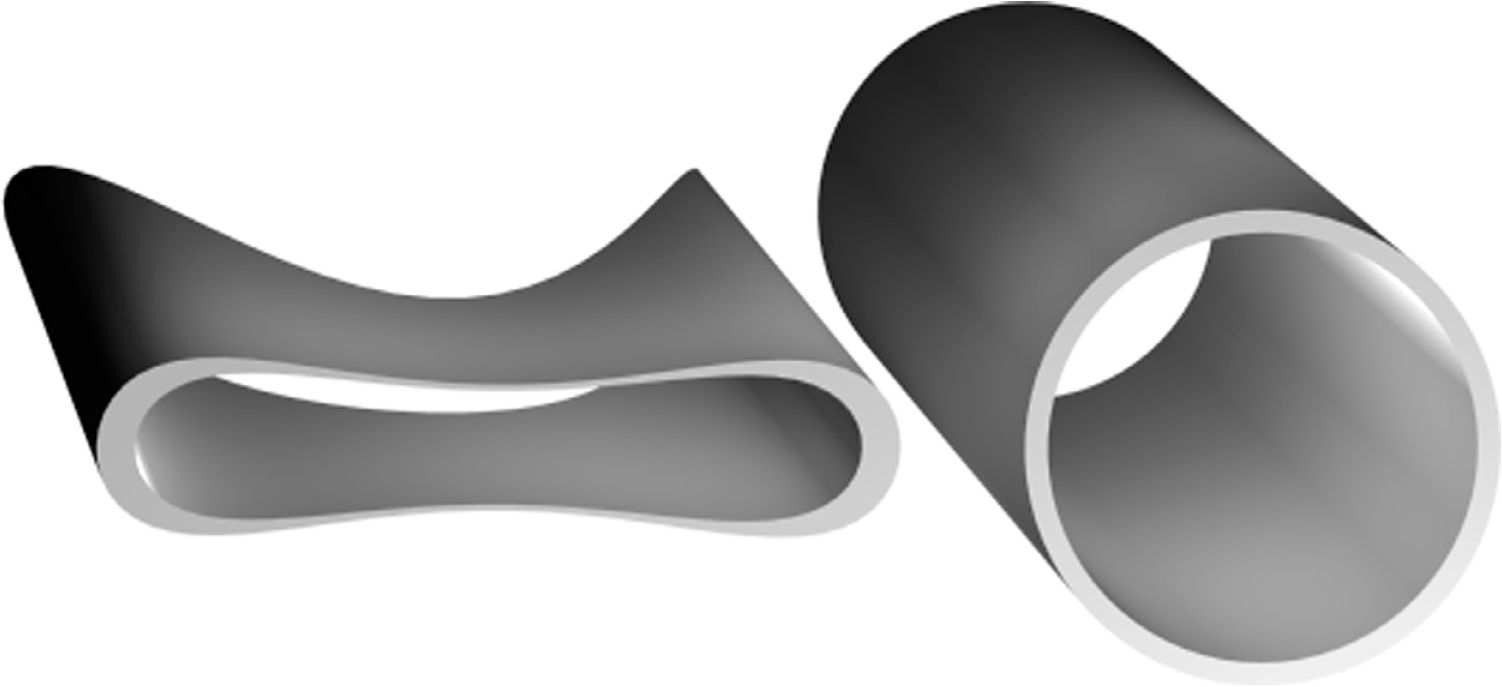
![]() FIGURE 3-2 Transformation of shape from oval to circular to accommodate increased volume without raising pressure.
FIGURE 3-2 Transformation of shape from oval to circular to accommodate increased volume without raising pressure.
TABLE 3-1
Histologic Changes Characteristic of Varicose Veins
Decreased smooth muscle cells
Apoptotic smooth muscle cells
Irregular bundles of collagen
Higher proportion of collagen, lower elastin content
Marked degenerative changes in intima and media
Adapted from Elsharawy MA, Naim MM, Abdelmaguid EM, Al-Mulhim AA. Role of saphenous vein wall in the pathogenesis of primary varicose veins. Interact Cardiovasc Thorac Surg. 2007 Apr;6(2):219-24. Epub 2006 Dec 1. PubMed PMID: 17669815.
Intima
The intima includes a layer of endothelial cells and a fenestrated basement membrane covered by an incomplete elastic lamina. The endothelial cell has multiple microvilli on its intravascular surface. Endothelial cells are easily damaged but have a remarkable regenerative ability. For successful sclerosis, this layer must be completely destroyed (Figure 3-3).
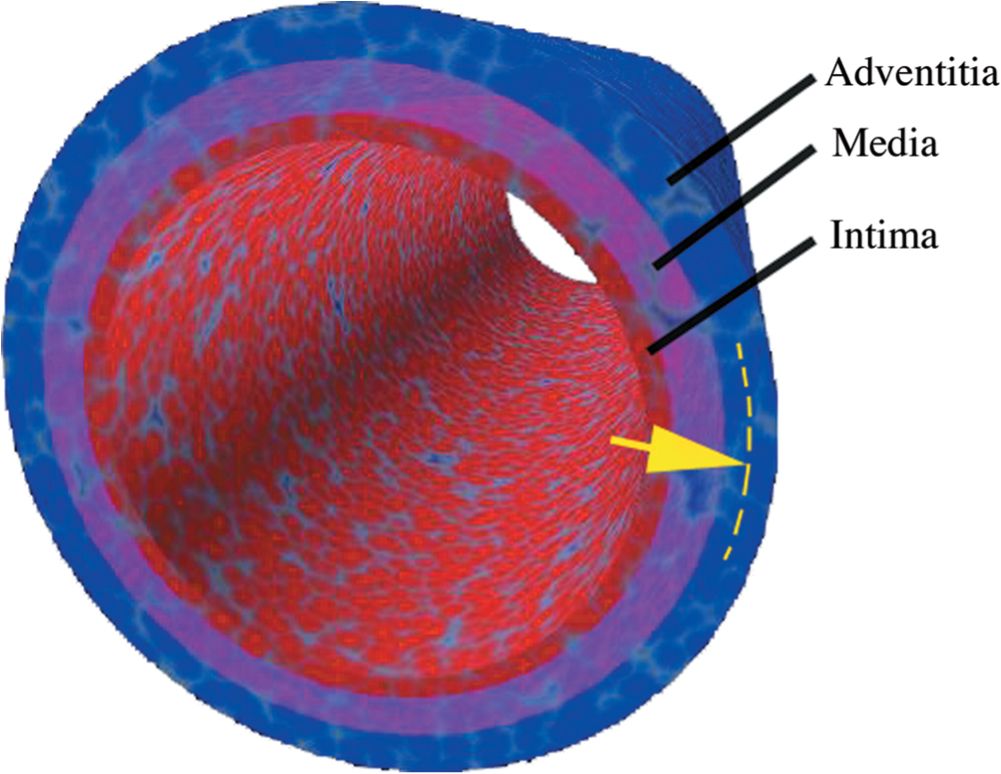
![]() FIGURE 3-3 Schematic of histologic layers of vein showing to which depth destruction must occur (yellow arrow) for sclerosis to be successful.
FIGURE 3-3 Schematic of histologic layers of vein showing to which depth destruction must occur (yellow arrow) for sclerosis to be successful.
Media
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


