BREAST AND COSMETIC 
Breast
 What is the next step following reduction mammaplasty when the resection specimen contains invasive ductal carcinoma?
What is the next step following reduction mammaplasty when the resection specimen contains invasive ductal carcinoma?
Determine tumor margins; decide on completion mastectomy.
 What is a critical factor in deciding breast contouring following implant removal?
What is a critical factor in deciding breast contouring following implant removal?
Preoperative ptosis (remains unchanged following removal).
 What best determines performing contouring and implant removal in the same setting?
What best determines performing contouring and implant removal in the same setting?
Thickness of residual breast (minimum thickness of 4 cm required).
 Compared to traditional transaxillary submuscular breast augmentation, endoscopic techniques are associated with a decreased rate of what?
Compared to traditional transaxillary submuscular breast augmentation, endoscopic techniques are associated with a decreased rate of what?
Malpositioning of the implant.
 Breast ptosis results from elongation and laxity of what structure?
Breast ptosis results from elongation and laxity of what structure?
Cooper ligaments.
 What is the most appropriate CPT code used for fat grafting?
What is the most appropriate CPT code used for fat grafting?
Fat grafting is reported with code 20926 (tissue grafts, other [e.g., paratenon, fat, dermis]) and includes the following: Harvest of the fat graft material by any method, closure of the donor site, processing of fat graft material, injection of fat graft into recipient site, and 90 days of routine postoperative care.
 Mastectomy resulting in decreased bulk in the inferior and lateral portions of the right pectoral muscle is caused by denervation of what nerve?
Mastectomy resulting in decreased bulk in the inferior and lateral portions of the right pectoral muscle is caused by denervation of what nerve?
Medial pectoral; C8–T1 supplies lower and lateral sternal portion of pectoralis major and pectoralis minor muscle.
 What does the lateral pectoral nerve supply?
What does the lateral pectoral nerve supply?
Arises from C5–6, supplies the medial portion of the pectoralis muscle.
 How does one assess the status of the pectoralis muscle in postmastectomy reconstruction?
How does one assess the status of the pectoralis muscle in postmastectomy reconstruction?
Have the patient place hands on hips and contract chest muscles.
 During breast augmentation, underfilling of the implants below the manufacturer’s recommended minimum will most likely have what effect?
During breast augmentation, underfilling of the implants below the manufacturer’s recommended minimum will most likely have what effect?
Decreases longevity of the implant and leads to early rupture.
 What advantage does an extended latissimus dorsi flap have over a standard latissimus dorsi flap in the setting of breast reconstruction?
What advantage does an extended latissimus dorsi flap have over a standard latissimus dorsi flap in the setting of breast reconstruction?
A decreased need for adjuvant breast implantation.
 What mammographic finding is seen 6 to 18 months following an inferior pedicle reduction mammoplasty?
What mammographic finding is seen 6 to 18 months following an inferior pedicle reduction mammoplasty?
Parenchymal redistribution, nipple elevation, calcifications, oil cysts from localized fat necrosis.
 Breast reduction by liposuction is most useful in breasts with what percentage of fat?
Breast reduction by liposuction is most useful in breasts with what percentage of fat?
50%.
 In a young patient undergoing MRM with postoperative radiation, what procedure will provide the best aesthetic reconstruction?
In a young patient undergoing MRM with postoperative radiation, what procedure will provide the best aesthetic reconstruction?
Delayed reconstruction with autologous tissue.
 In a study comparing early and late complications in patients who underwent TRAM reconstruction followed by radiation versus radiation treatment followed by TRAM reconstruction, what were the differences?
In a study comparing early and late complications in patients who underwent TRAM reconstruction followed by radiation versus radiation treatment followed by TRAM reconstruction, what were the differences?
The early complications did not differ, but the late complications were more frequent in the group undergoing immediate reconstruction.
 A woman who has the BRCA2 mutation has a lifetime incidence of what percentage of developing breast cancer?
A woman who has the BRCA2 mutation has a lifetime incidence of what percentage of developing breast cancer?
60%.
 Sharp dissection lateral to the lateral edge of the pectoralis muscle during augmentation mammaplasty may result in what complication?
Sharp dissection lateral to the lateral edge of the pectoralis muscle during augmentation mammaplasty may result in what complication?
Numbness of the nipple–areola complex; the fourth and fifth anterolateral intercostal nerves provide sensation to the nipple–areola complex.
 What is consistently the best marking for the new nipple position during reduction mammaplasty?
What is consistently the best marking for the new nipple position during reduction mammaplasty?
The inframammary fold.
 What represents the lateral border of the breast footprint?
What represents the lateral border of the breast footprint?
Anterior axillary fold.
 Sensation to the nipple–areolar complex is derived from what?
Sensation to the nipple–areolar complex is derived from what?
Anterolateral branches of the third through fifth intercostal nerves (primarily the fourth nerve).
 Define pseudoptosis of the breast.
Define pseudoptosis of the breast.
The nipple remains above the IMF, but the breast mass descends below the NAC.
 What is first-degree ptosis?
What is first-degree ptosis?
The NAC descends to the level of the IMF.
 What is second-degree ptosis?
What is second-degree ptosis?
The nipple is located beneath the IMF, but is not the lowest point of the breast.
 In polymastia, where are accessory mammary structure most commonly found?
In polymastia, where are accessory mammary structure most commonly found?
The axilla.
 What supplies sensation to the upper breast?
What supplies sensation to the upper breast?
Cervical branches from the third and fourth.
 The medial and inferior breast?
The medial and inferior breast?
Branches from the anterior cutaneous branches.
 What is the most common cause of asymmetric enlargement of a breast over a year with a palpable mass in a teenage girl?
What is the most common cause of asymmetric enlargement of a breast over a year with a palpable mass in a teenage girl?
Fibroadenoma; treat with excision.
 What is the first treatment for nipple cyanosis following breast reduction?
What is the first treatment for nipple cyanosis following breast reduction?
Releasing the sutures surrounding the NAC and return to the OR.
 What are the criteria for free nipple grafting?
What are the criteria for free nipple grafting?
Reduction amount greater than 1,500 g, nipple transposition length greater than 25 cm, and a history of smoking or diabetes.
 What affects the quality of mammography with breast implants?
What affects the quality of mammography with breast implants?
Implant position, capsular contracture, native breast volume.
 What common medications may cause gynecomastia?
What common medications may cause gynecomastia?
Tagamet, Digoxin, Minocycline, spironolactone.
 What are key elements of the Lejour reduction mammaplasty?
What are key elements of the Lejour reduction mammaplasty?
Central vertical gland excision and excision of skin in one direction, upper pedicle, more difficult to determine resection end point.
 What is considered the best reconstructive option for the breast as a secondary procedure following mastectomy and irradiation?
What is considered the best reconstructive option for the breast as a secondary procedure following mastectomy and irradiation?
TRAM reconstruction; implant reconstruction associated with increased capsular contraction rate with prior irradiation.
 What condition has an increased risk of hypercoaguability and must be considered in free flap reconstruction?
What condition has an increased risk of hypercoaguability and must be considered in free flap reconstruction?
Systemic lupus erythematosus (SLE).
 What is the next appropriate step for a woman preceding breast augmentation with milky discharge and regular menstrual cycles?
What is the next appropriate step for a woman preceding breast augmentation with milky discharge and regular menstrual cycles?
Obtaining a serum prolactin level to rule out a pituitary lesion; thyroid function studies, medication history (e.g., tricyclic antidepressants).
 What is the most frequent complication following periareolar mastopexy?
What is the most frequent complication following periareolar mastopexy?
Areolar widening.
 What defines a tuberous breast?
What defines a tuberous breast?
Constricted appearance of breast; unilateral narrowing of the breast; narrow breast diameter, superior displacement of the IMF; areola enlarged; breast hypoplasia.
 How is a tuberous breast treated?
How is a tuberous breast treated?
Augmentation mammaplasty with IMF adjustment, radial scoring of the breast glandular tissue, areola reduction.
 What is the rate of additional procedures following breast implant augmentation?
What is the rate of additional procedures following breast implant augmentation?
25% of patients requiring additional procedure within 13 years.
 What is the rate of deflation after implant augmentation?
What is the rate of deflation after implant augmentation?
1% annually.
 What is the approximate rate of capsular contraction?
What is the approximate rate of capsular contraction?
20% to 25%.
 What portion of breast parenchyma is affected after implant augmentation?
What portion of breast parenchyma is affected after implant augmentation?
Estimated 5%, not entirely seen on mammography.
 What nerve supplies the nipple–areola complex?
What nerve supplies the nipple–areola complex?
The lateral branch of the fourth intercostal nerves.
 What factors are increased in smokers who undergo free TRAM breast reconstruction?
What factors are increased in smokers who undergo free TRAM breast reconstruction?
Necrosis of the mastectomy skin, abdominal skin, and hernia rates.
 What factors are not increased with smokers undergoing free TRAM breast reconstruction?
What factors are not increased with smokers undergoing free TRAM breast reconstruction?
Vessel thrombosis, fat necrosis, flap loss, or wound infection.
 What are the grades of gynecomastia?
What are the grades of gynecomastia?
I: mild enlargement without redundant skin.
IIA: moderate enlargement without redundant skin.
IIB: moderate enlargement with skin redundancy.
III: marked enlargement with significant redundant skin.
 What are the methods of treating gynecomastia?
What are the methods of treating gynecomastia?
Suction lipectomy, excising a concentric circle of skin, amputation with free nipple grafting, glandular resection with liposuction.
 What are the general indications for delayed mastopexy following implant explantation?
What are the general indications for delayed mastopexy following implant explantation?
Marked ptosis requiring nipple elevation of greater than 4 cm, breast mound less than 4 cm, smoking history.
 What is the procedure that should be done for grade II breast ptosis?
What is the procedure that should be done for grade II breast ptosis?
For repositioning of the nipple–areola complex of 2 to 4 cm, a Wise pattern mastopexy may be performed.
 What procedure is recommended for pseudoptosis?
What procedure is recommended for pseudoptosis?
Wedge excision from the inframammary fold.
 What is the most appropriate next step for a smoker having undergone implant explantation with marked ptosis and less than 4 cm of breast thickness?
What is the most appropriate next step for a smoker having undergone implant explantation with marked ptosis and less than 4 cm of breast thickness?
Delayed mastopexy for 3 months at minimum.
 What patients are appropriate candidates for nipple sparing mastectomy?
What patients are appropriate candidates for nipple sparing mastectomy?
Tumor size of 3 cm or less, at least 2 cm from the nipple, not multicentric, and those with clinically negative nodes.
 After bilateral TRAM elevation, what supplies the umbilicus primarily?
After bilateral TRAM elevation, what supplies the umbilicus primarily?
Ligamentum teres.
 To minimize hernia recurrence following abdominal-based autologous reconstruction, where is the optimal position to place mesh to minimize recurrence?
To minimize hernia recurrence following abdominal-based autologous reconstruction, where is the optimal position to place mesh to minimize recurrence?
Between rectus muscle and posterior rectus sheath.
 What are the venous thromboembolism guidelines based on Caprini score (risk assessment model)?
What are the venous thromboembolism guidelines based on Caprini score (risk assessment model)?
Patients undergoing major plastic and reconstructive operative procedures performed during general anesthesia that last longer than 60 minutes should receive VTE prevention. For patients with Caprini score of 3 to 6, the use of postoperative low–molecular-weight heparin (LMWH) or unfractionated heparin (UH) should be considered. For patients with Caprini score of 3 or more, use of mechanical prophylaxis throughout the duration of chemical prophylaxis for nonambulatory patients should be considered. For patients with Caprini score of 7 or more, the use of extended LMWH postoperative prophylaxis should be strongly considered.
 What is the greatest source of dissatisfaction following breast reduction?
What is the greatest source of dissatisfaction following breast reduction?
Noticeable scarring.
 Following reduction mammaplasty, what is the percentage of being able to breast-feed?
Following reduction mammaplasty, what is the percentage of being able to breast-feed?
30%.
 What is the best radiologic study to assess for silicone breast implant rupture? What is the linguine sign?
What is the best radiologic study to assess for silicone breast implant rupture? What is the linguine sign?
MRI. The linguine sign is a finding on MRI of multiple curvilinear low–signal-intensity lines within the high–signal-intensity silicone gel signifying implant rupture.
 Patient presents 6 weeks after breast reduction with a firm, painless mass in the breast. Diagnosis?
Patient presents 6 weeks after breast reduction with a firm, painless mass in the breast. Diagnosis?
Fat necrosis.
 Define the following chest wall abnormalities:
Define the following chest wall abnormalities:
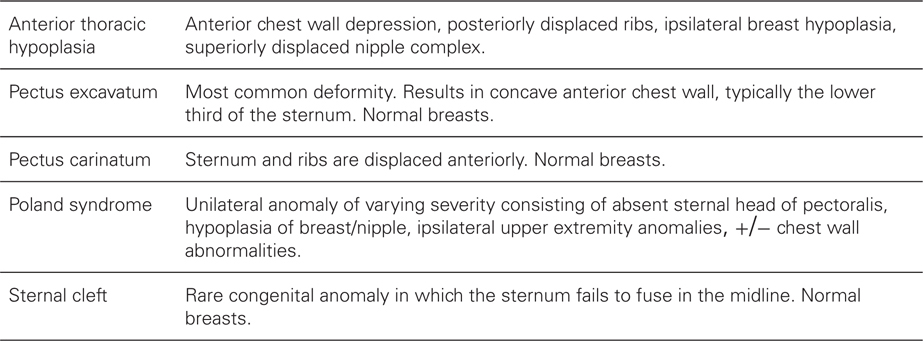
 What findings are seen in Poland syndrome?
What findings are seen in Poland syndrome?
Pectoralis muscle sternal head hypoplasia, hypoplasia/aplasia of the breast, ipsilateral hand anomalies; males and females equally affected; chest wall anomalies.
 What is the initial management of gynecomastia in puberty in the absence of other abnormalities?
What is the initial management of gynecomastia in puberty in the absence of other abnormalities?
Observation and follow-up in 12 months.
 How old do you have to be to get cosmetic silicone breast augmentation?
How old do you have to be to get cosmetic silicone breast augmentation?
The FDA has approved silicone gel breast implants for women aged 22 and older. Younger patients get saline implants.
 What is the proper shape and location of the male nipple–areola complex?
What is the proper shape and location of the male nipple–areola complex?
Oval in shape and located at the fourth to fifth intercostal spaces.
 True/False: Size of the implant in breast augmentation influences postoperative nipple sensation.
True/False: Size of the implant in breast augmentation influences postoperative nipple sensation.
True.
 What is the downside to using a textured silicone implant over a smooth silicone implant?
What is the downside to using a textured silicone implant over a smooth silicone implant?
Increased rate of rippling.
 True/False: Textured implants have a higher rate of capsular contracture than smooth implants?
True/False: Textured implants have a higher rate of capsular contracture than smooth implants?
False, they have slightly less.
 What nerves may be injured during transaxillary breast augmentation?
What nerves may be injured during transaxillary breast augmentation?
Intercostobrachial and medial brachial cutaneous nerves providing sensation to the medial aspect of the upper arm.
 What is the lifetime risk of breast cancer in a male with the BRCA2 gene mutation? Female with BRCA1 mutation? Female with BRCA2 mutation?
What is the lifetime risk of breast cancer in a male with the BRCA2 gene mutation? Female with BRCA1 mutation? Female with BRCA2 mutation?
7% in males, in females, 85% BRCA1, 60% BRCA2.
 What is a phyllodes tumor? How is it treated?
What is a phyllodes tumor? How is it treated?
Tumors from the periductal stromal cells of the breast. They are typically fast growing but 90% are benign. Management is local excision and close annual surveillance.
Nose
 How is a “hanging” columella treated?
How is a “hanging” columella treated?
Trimming of the caudal margin of the septum and medial crura of the lower lateral cartilage.
 What is the best flap to use for a defect of the lateral nasal ala?
What is the best flap to use for a defect of the lateral nasal ala?
Nasolabial flap, superiorly based.
 What should be used for a defect of the lateral nasal wall above the ala?
What should be used for a defect of the lateral nasal wall above the ala?
Cheek advancement flap.
 A defect of the caudal third of the nose centrally?
A defect of the caudal third of the nose centrally?
Frontonasal flap.
 What skin characteristics negatively affect results after rhinoplasty?
What skin characteristics negatively affect results after rhinoplasty?
Thick skin with large sebaceous glands; skin envelope does not conform easily.
 What are the three zones of injury occurring in a nasal fracture?
What are the three zones of injury occurring in a nasal fracture?
Upper vault (nasal bones, ethmoid, vomer, cephalic septal border); middle vault (upper lateral cartilages, septum, maxilla); lower vault (alar cartilages, inferior septum).
 What is the limit at which airway resistance increases in the internal nasal valve?
What is the limit at which airway resistance increases in the internal nasal valve?
Less than 10 to 12 degrees.
 What defines the internal nasal valve area?
What defines the internal nasal valve area?
The caudal margin of the upper lateral cartilage, septum, nasal floor, and anterior edge of inferior turbinate.
 Secondary healing of what part of the nose is least likely to provide an acceptable cosmetic result?
Secondary healing of what part of the nose is least likely to provide an acceptable cosmetic result?
The nasal tip.
 What techniques have important roles in providing tip projection in addition to tip grafting?
What techniques have important roles in providing tip projection in addition to tip grafting?
Suturing of the medial crura, placing a strut graft between the medial crura.
 What effect occurs with resection of the lateral and medial crura and the nasal spine?
What effect occurs with resection of the lateral and medial crura and the nasal spine?
Decrease of tip projection.
 What effect does a complete transfixion incision have?
What effect does a complete transfixion incision have?
Decreases projection secondary to weakening of nasal support.
 True/False: The evaluation of the nasal airway should include the nasal dorsum.
True/False: The evaluation of the nasal airway should include the nasal dorsum.
False.
 In a patient with a negative Cottle maneuver, what procedure is likely to improve the nasal airway?
In a patient with a negative Cottle maneuver, what procedure is likely to improve the nasal airway?
Lateral strut graft of the crus.
 What comprises the external nasal valve?
What comprises the external nasal valve?
Columella, ala, nasal sill.
 What comprises the internal nasal valve?
What comprises the internal nasal valve?
Area of the angle between the upper lateral cartilage and septum.
 How is vestibular stenosis treated?
How is vestibular stenosis treated?
An alar base flap.
 What factors lead to a saddle nose deformity?
What factors lead to a saddle nose deformity?
Excessive dorsal or septal resection, nasal bone comminution during infracture, or a fracture of the perpendicular ethmoid plate.
 What supplies sensation to the nasal radix?
What supplies sensation to the nasal radix?
The supratrochlear and infratrochlear nerves.
 What supplies sensation to the nasal tip?
What supplies sensation to the nasal tip?
External nasal branch of the anterior ethmoidal nerve; emerges from nasal bone and lateral nasal cartilage.
 What part of the nose is innervated by the infraorbital nerve?
What part of the nose is innervated by the infraorbital nerve?
Lower lateral half and skin of the columella.
 What is supplied by the infratrochlear nerve?
What is supplied by the infratrochlear nerve?
Superior portion of the nasal side wall and skin over the radix.
 Where is a 1-cm defect on the nose most amenable to healing by secondary intention?
Where is a 1-cm defect on the nose most amenable to healing by secondary intention?
Area of the medial canthus, glabella, nasolabial fold, and philtrum.
 What is the blood supply to the nasal tip during an open rhinoplasty?
What is the blood supply to the nasal tip during an open rhinoplasty?
Lateral nasal artery that arises from the angular artery.
 What artery is divided during open rhinoplasty?
What artery is divided during open rhinoplasty?
The columellar branch of the superior labial artery.
 What vessels from the internal carotid artery supply the nasal skin?
What vessels from the internal carotid artery supply the nasal skin?
Dorsal nasal artery, external branch of the ethmoidal artery.
 What defect is a dorsal nasal flap typically used for?
What defect is a dorsal nasal flap typically used for?
A defect of the nasal tip up to 2 cm.
 What is the polybeak deformity following rhinoplasty due to?
What is the polybeak deformity following rhinoplasty due to?
Excessive reduction of the tip particularly in the setting of poor nasal tip projection.
 What is the treatment for alar collapse with inspiration and a pinched nasal tip?
What is the treatment for alar collapse with inspiration and a pinched nasal tip?
Grafting of the nasal tip with cartilage.
 What are the causes of a saddle nose deformity after rhinoplasty?
What are the causes of a saddle nose deformity after rhinoplasty?
Overresection of the septum, separation of the cartilaginous septum from the vomer, collapse of the vertical component of the L-strut.
 What causes the inverted V deformity after rhinoplasty?
What causes the inverted V deformity after rhinoplasty?
Collapse of the upper lateral cartilage.
 What causes the open-roof deformity after rhinoplasty?
What causes the open-roof deformity after rhinoplasty?
Failure of the nasal bones to come together in the midline after osteotomies.
 What causes a stair-step deformity after rhinoplasty?
What causes a stair-step deformity after rhinoplasty?
An osteotomy that is too high on the nasal process and not flush with the maxilla resulting in a visible and palpable deformity.
 How do you correct the inverted V deformity after rhinoplasty?
How do you correct the inverted V deformity after rhinoplasty?
Spreader grafts correct the collapse of the internal nasal valve.
 What is the advantage of partial submucous resection of the inferior turbinate over turbinate ablation?
What is the advantage of partial submucous resection of the inferior turbinate over turbinate ablation?
Decreased incidence of atrophic rhinitis.
 How do you treat a collapsed external nasal valve?
How do you treat a collapsed external nasal valve?
Alar batten grafts.
Ear
 What is the Antia–Buch flap used for?
What is the Antia–Buch flap used for?
Lesions located on the lateral rim; tissue used from postauricular skin to reconstruct the helical margin.
 Where on the avulsed pinna is anastomosis of the arteries most appropriate?
Where on the avulsed pinna is anastomosis of the arteries most appropriate?
The posterior surface; larger arteries enter the pinna on the posterior surface.
 Treatment of an auricular hematoma by needle aspiration is likely to result in what?
Treatment of an auricular hematoma by needle aspiration is likely to result in what?
Seroma.
 A 6-year-old boy with an obtuse concha-mastoid angle with a normal antihelical fold is best treated by what technique?
A 6-year-old boy with an obtuse concha-mastoid angle with a normal antihelical fold is best treated by what technique?
Setback of the concha using concha-mastoid sutures.
 What are common causes of prominent ears?
What are common causes of prominent ears?
Enlarged conchal bowl, obtuse concha-mastoid angle, loss of the antihelical fold.
 How is ear prominence corrected from loss of the antihelical fold?
How is ear prominence corrected from loss of the antihelical fold?
Abrading or scoring the antihelix and placing Mustarde sutures between the conchal and scaphoid eminence.
 True/False: Microtia and inner ear abnormalities may be closely related.
True/False: Microtia and inner ear abnormalities may be closely related.
False.
 What is orbital auricular vertebral syndrome otherwise known as?
What is orbital auricular vertebral syndrome otherwise known as?
Goldenhar syndrome (associated with microtia, cervical spine abnormalities, mandibular hypoplasia, preauricular pits/sinuses, hemifacial microsomia).
 What develops from the first three hillocks of the ear during development?
What develops from the first three hillocks of the ear during development?
First three hillocks are from the first arch; tragus, helical root, superior helix.
 What develops from the second three hillocks of the ear?
What develops from the second three hillocks of the ear?
Antitragus, antihelix, inferior helix and lobule; from the second branchial arch.
 What is the treatment principle of cryptotia?
What is the treatment principle of cryptotia?
Detaching the superior auricle from the temporal area and placing a skin graft in the retroauricular area.
 How is Stahl ear treated?
How is Stahl ear treated?
Advancing the third crus of the antihelix.
 Placing sutures from the concha to the mastoid bowl and rasping the anterior surface of the antihelix has been described for what condition?
Placing sutures from the concha to the mastoid bowl and rasping the anterior surface of the antihelix has been described for what condition?
Correction of prominent ears.
 How is the constricted ear treated?
How is the constricted ear treated?
Partially detaching the helix from the scapha and suturing the helix.
 What is the treatment for an auricular implant (porous polyethylene) covered with a temporoparietal fascial flap with subsequent exposure of the implant?
What is the treatment for an auricular implant (porous polyethylene) covered with a temporoparietal fascial flap with subsequent exposure of the implant?
Dressing changes and secondary wound healing for at least 6 months.
 What principle guides the Mustarde otoplasty approach?
What principle guides the Mustarde otoplasty approach?
Using mattress sutures to bend the antihelix.
 What is the Stenstrom technique?
What is the Stenstrom technique?
Using an otoabrader to bend the anterior antihelical surface.
 What is the Graham and Gault otoplasty technique?
What is the Graham and Gault otoplasty technique?
Endoscopic scoring and suture of the cartilage posteriorly.
 What is the Luckett procedure?
What is the Luckett procedure?
Excision of a crescent-shaped piece of skin/cartilage.
 What is the Furnas technique?
What is the Furnas technique?
Sutures spanning the concha to the mastoid.
 What are the common descriptive findings in the prominent ear?
What are the common descriptive findings in the prominent ear?
Conchal valgus, cranioauricular angle greater than 40 degrees, antihelical underfolding; widened conchoscaphal angle (greater than 90 degrees).
 What are general options for correcting the prominent ear?
What are general options for correcting the prominent ear?
Concha to scapha sutures, concha to mastoid sutures, scoring the cartilage anteriorly, conchal resection, postauricular skin resection.
 What is the optimal timing for microtia surgery in a child?
What is the optimal timing for microtia surgery in a child?
At 6 to 7 years of age, the ear is practically fully developed by age 7.
 What is the ear canal typically created in microtia with respect to auricular reconstruction?
What is the ear canal typically created in microtia with respect to auricular reconstruction?
Typically following the creation of the auricle.
 What is the initial management of the neonate with prominent ears?
What is the initial management of the neonate with prominent ears?
Molding with tape and splinting.
 How long do maternal estrogens remain in the neonate?
How long do maternal estrogens remain in the neonate?
6 months, which allows for shaping of auricular cartilage.
 What is the Stahl ear deformity?
What is the Stahl ear deformity?
A third crus, antihelical flattening, scaphoid fossa deformity.
 What is the constricted ear?
What is the constricted ear?
Helical and scaphal hooding.
 What is seen in cryptotia?
What is seen in cryptotia?
Upper pole of the ear is buried beneath skin; absence of superior auriculocephalic sulcus missing.
 What nerve supplies sensation to the superior cranial surface of the ear?
What nerve supplies sensation to the superior cranial surface of the ear?
Lesser occipital nerve.
 What nerve supplies sensation to the skin of the anterosuperior EAC?
What nerve supplies sensation to the skin of the anterosuperior EAC?
Lesser occipital nerve.
 What areas are supplied by the great auricular nerve?
What areas are supplied by the great auricular nerve?
Inferior half of the lateral ear and inferior portion of the cranial surface of the ear.
 What area is supplied by the auriculotemporal nerve?
What area is supplied by the auriculotemporal nerve?
Sensation to the anterosuperior surface of the external ear.
 What does Arnold nerve supply?
What does Arnold nerve supply?
Sensation to the concha and posterior EAC.
 At what trimester does maldevelopment occur and microtia result?
At what trimester does maldevelopment occur and microtia result?
First trimester between 4.5 and 10 weeks.
 What is the treatment for a complete upper auricular defect from a burn several years ago?
What is the treatment for a complete upper auricular defect from a burn several years ago?
Rib cartilage framework for the upper ear with temporoparietal fascia flap and skin graft.
 What is the likely cause of recurrent prominence of ears following otoplasty at 7 months?
What is the likely cause of recurrent prominence of ears following otoplasty at 7 months?
Suture failure at the antihelical fold.
Eye
 What is the treatment for chronic ectropion and excessive scleral show after a chemical burn?
What is the treatment for chronic ectropion and excessive scleral show after a chemical burn?
Full-thickness skin grafting.
 What is the mechanism of involutional ectropion?
What is the mechanism of involutional ectropion?
Laxity of the lower lid from the lower lid retractors becoming disinserted from the tarsal plate.
 What is the treatment for involutional ectropion?
What is the treatment for involutional ectropion?
Lateral canthoplasty, lateral wedge excision, or excising of a full-thickness wedge from the lateral canthal region.
 What structure does the common canaliculus enter the lacrimal sac posterior to?
What structure does the common canaliculus enter the lacrimal sac posterior to?
The medial canthal tendon.
 What muscle is most commonly injured in blepharoplasty?
What muscle is most commonly injured in blepharoplasty?
Superior oblique; clinically may see tilting of head, and depression of chin.
 What is the procedure required for a patient who exhibits a Jones I test without dye and a Jones II test with dye in the tear sac?
What is the procedure required for a patient who exhibits a Jones I test without dye and a Jones II test with dye in the tear sac?
Dacryocystorhinostomy.
 How is a Jones I test performed?
How is a Jones I test performed?
Instill 2% fluorescein dye into the conjunctival fornices; recovery of dye indicates a normal lacrimal system (or positive result); a negative result necessitates a Jones II test.
 How is a Jones II test performed?
How is a Jones II test performed?
Dilation of the punta is performed first; fluid passing into the nose indicates that obstruction of the nasolacrimal duct is cleared.
 A negative Jones I and a positive Jones II test indicate what?
A negative Jones I and a positive Jones II test indicate what?
Blockage of the nasolacrimal duct system.
 What procedure will address lower eyelid skin laxity with 2 mm of scleral show bilaterally?
What procedure will address lower eyelid skin laxity with 2 mm of scleral show bilaterally?
Lower lid blepharoplasty with lateral canthopexy.
 Following lower lid blepharoplasty, a woman exhibiting scleral show, round, sad-looking eyes, photophobia, epiphora, what has anatomically occurred?
Following lower lid blepharoplasty, a woman exhibiting scleral show, round, sad-looking eyes, photophobia, epiphora, what has anatomically occurred?
Scarring between the orbital septum and the capsulopalpebral fascia, resulting in lower lid retraction (without lid eversion); other causes include lateral canthal tendon laxity, midface descent.
 What is the eyelid function in patients with Bell palsy?
What is the eyelid function in patients with Bell palsy?
Ectropion from dysfunction of the orbicularis muscle; inability to close the eye.
 What characterizes aponeurotic ptosis?
What characterizes aponeurotic ptosis?
Good levator function; elevation of eyelid crease, ability to visualize shadow of iris with eyelid closure (positive Nesi sign), or translucent upper eyelid.
 What may be done to improve excess scleral show and slowed retraction of a “snap-back” test following blepharoplasty?
What may be done to improve excess scleral show and slowed retraction of a “snap-back” test following blepharoplasty?
Lateral canthopexy.
 How is a patient treated with 3.5 mm of ptosis and 10-mm levator function?
How is a patient treated with 3.5 mm of ptosis and 10-mm levator function?
Resuturing of the levator aponeurosis.
 What are the classifications of ptosis?
What are the classifications of ptosis?
Neurogenic, myogenic, mechanical, aponeurotic.
 When is eyebrow suspension used for ptosis treatment?
When is eyebrow suspension used for ptosis treatment?
Poor levator function (less than 4 mm) and greater than 3 mm of ptosis.
 When is the Fasanella–Servat procedure used?
When is the Fasanella–Servat procedure used?
Good levator function and minimal ptosis (less than 2 mm).
 What procedure is used for levator function between 4- and 10-mm and 3-mm ptosis?
What procedure is used for levator function between 4- and 10-mm and 3-mm ptosis?
Levator resection.
 What is the treatment of 4-mm ptosis and 2-mm levator function in a 5-year-old child?
What is the treatment of 4-mm ptosis and 2-mm levator function in a 5-year-old child?
Frontalis suspension.
 What is associated with inadvertent blepharoptosis—Botox injection of the corrugator or lateral orbicularis?
What is associated with inadvertent blepharoptosis—Botox injection of the corrugator or lateral orbicularis?
The corrugator.
 Transcutaneous lower lid blepharoplasty is associated with what undesired finding most commonly?
Transcutaneous lower lid blepharoplasty is associated with what undesired finding most commonly?
Malpositioned lower eyelids.
 What may be done for asymmetrical lower eyelids following blepharoplasty?
What may be done for asymmetrical lower eyelids following blepharoplasty?
Conservative (taping, Frost stitches) treatment first; surgery for failed conservative treatment (tarsal strip, wedge tarsectomy).
 What percentage of patients undergoing orbital floor fracture repair through a preseptal transconjunctival approach develop ectropion?
What percentage of patients undergoing orbital floor fracture repair through a preseptal transconjunctival approach develop ectropion?
Close to 0%.
 What clinical findings are seen in levator aponeurosis dehiscence?
What clinical findings are seen in levator aponeurosis dehiscence?
Ptosis, elevated supratarsal crease, thinning of upper eyelid skin.
 What is typically done for levator aponeurosis dehiscence?
What is typically done for levator aponeurosis dehiscence?
Levator advancement.
 What is a likely cause of chronic lower lid deformity following ORIF of the orbital floor?
What is a likely cause of chronic lower lid deformity following ORIF of the orbital floor?
Posterior lamella shortening; posterior lamella (capsulopalpebral fascia) comprising tarsus, lower lid retractors, conjunctiva.
 What is done for nasolacrimal duct obstruction?
What is done for nasolacrimal duct obstruction?
Dacryocystorhinostomy.
 What predisposing factors cause patients to have dry eye syndrome after blepharoplasty?
What predisposing factors cause patients to have dry eye syndrome after blepharoplasty?
Exophthalmos, scleral show, lower lid hypotonia, maxillary hypoplasia.
 What is blepharochalasis?
What is blepharochalasis?
Recurrent episodes of painless edema of the eyelids; unclear etiology; caused by elastic tissue deficiency; leading to “baggy” appearance of lids.
 What is dermatochalasis?
What is dermatochalasis?
Excess eyelid skin.
 What is the blepharophimosis syndrome?
What is the blepharophimosis syndrome?
Genetic condition; telecanthus, ptosis, upper eyelid phimosis.
 What is the most common form of acquired ptosis?
What is the most common form of acquired ptosis?
Involutional; results from thinning of the levator aponeurosis; good levator function, elevated eyelid creases.
 What characterizes blepharophimosis syndrome?
What characterizes blepharophimosis syndrome?
Type I: large epicanthal folds, epicanthus inversus, horizontal shortening of the eyelids, marked ptosis.
Type II: telecanthus, epicanthal fold absence, bilateral ptosis, no levator function, shortened eyelids.
Type III: missing epicanthal folds, telecanthus, antimongoloid slant; telecanthus.
 What treatment is done for blepharophimosis?
What treatment is done for blepharophimosis?
Epicanthal fold repair, levator resection, medial canthoplasty, eyelid suspension.
 What defines normal levator function?
What defines normal levator function?
Greater than 10 mm of excursion.
 What degree of ptosis is the Fasanella–Servat procedure performed for?
What degree of ptosis is the Fasanella–Servat procedure performed for?
Mild ptosis.
 What is given for ptosis seen in Horner syndrome?
What is given for ptosis seen in Horner syndrome?
Phenylephrine eye drops.
 What is the treatment of choice 14 days after blepharoplasty in a patient with lagophthalmos?
What is the treatment of choice 14 days after blepharoplasty in a patient with lagophthalmos?
Corneal lubrication.
 What structure are the upper eyelid fat pads immediately posterior to?
What structure are the upper eyelid fat pads immediately posterior to?
The orbital septum; the fat pads sit just anterior to the levator aponeurosis.
 In the lower lids the fat pads are located just anterior to what structure?
In the lower lids the fat pads are located just anterior to what structure?
The inferior retractors.
 What separates the medial and middle fat pads in the lower lid?
What separates the medial and middle fat pads in the lower lid?
The inferior oblique.
 What is an epiblepharon?
What is an epiblepharon?
A congenital anomaly in which a fold of skin lies across the upper or lower lid margin. In the lower eyelid it causes a turning inward of the eyelashes.
 What is senile ptosis?
What is senile ptosis?
Most common cause of ptosis in elderly patients, the result of dehiscence of the levator aponeurosis. The supratarsal crease is elevated on examination.
 How do you measure the prominence of the globe in relation to the orbit?
How do you measure the prominence of the globe in relation to the orbit?
Distance from anterior border of globe to most anterior aspect of the lateral orbital rim. Enophthalmos is <14 mm, exophthalmos is >18 mm.
 What happens to the lacrimal drainage system on eyelid closure?
What happens to the lacrimal drainage system on eyelid closure?
Lacrimal puncta are closed, the lacrimal diaphragm is compressed, the lacrimal sac opens.
 What is the appropriate amount of pretarsal eyelid show?
What is the appropriate amount of pretarsal eyelid show?
2 to 5 mm.
 What is symblepharon?
What is symblepharon?
Pathologic adhesion of the palpebral conjunctiva to the bulbar conjunctiva, usually related to thermal injury.
 What is chemosis?
What is chemosis?
Edema of the bulbar conjunctiva.
 What is a chalazion?
What is a chalazion?
A cyst on the eyelid caused by inflammation from a blocked meibomian gland.
 What is a hordeolum?
What is a hordeolum?
Also known as a sty, it is an infection of the sebaceous glands at the base of the eyelashes. Unlike a chalazion, these are acute, painful and usually do not resolve without intervention.
 What is the function of the inferior oblique muscle? Superior oblique muscle?
What is the function of the inferior oblique muscle? Superior oblique muscle?
Inferior oblique: abducts, elevates, laterally rotates; superior oblique: abducts, depresses, medially rotates.
 What is the most commonly injured muscle during blepharoplasty?
What is the most commonly injured muscle during blepharoplasty?
Inferior oblique muscle. Presents as diplopia with upward gaze.
 What muscle acts as the primary depressor of the lateral eyebrow?
What muscle acts as the primary depressor of the lateral eyebrow?
Orbicularis oculi muscle.
Face
 What type of genioplasty should be performed in a patient with sagittal deficiency and vertical excess with class I occlusion?
What type of genioplasty should be performed in a patient with sagittal deficiency and vertical excess with class I occlusion?
Jumping genioplasty.
 Where should the brow peak in a female patient undergoing browlifting?
Where should the brow peak in a female patient undergoing browlifting?
At the lateral limbus to lateral canthal area.
 What branch of the facial nerve is injured most frequently during face lift?
What branch of the facial nerve is injured most frequently during face lift?
Buccal.
 What effect do corticosteroids have on edema and ecchymosis following rhytidectomy?
What effect do corticosteroids have on edema and ecchymosis following rhytidectomy?
No change in both instances.
 Compared with primary rhytidectomy, distortion of the hairline is more or less frequent in secondary rhytidectomy?
Compared with primary rhytidectomy, distortion of the hairline is more or less frequent in secondary rhytidectomy?
More likely to occur; if the same incisions are used, recession of the temporal hairline, obliteration of sideburn hair, and alopecia may occur.
 Are the risks of hematoma, hypertrophic scarring, and skin slough higher in the setting of secondary rhytidectomy?
Are the risks of hematoma, hypertrophic scarring, and skin slough higher in the setting of secondary rhytidectomy?
Typically not.
 What adverse effect is lessened by endoscopic browlifting as opposed to conventional coronal browlifting?
What adverse effect is lessened by endoscopic browlifting as opposed to conventional coronal browlifting?
Scalp sensibility changes.
 In a patient with microgenia who has both bony deficiencies in the anteroposterior and vertical dimensions, what is the most appropriate treatment?
In a patient with microgenia who has both bony deficiencies in the anteroposterior and vertical dimensions, what is the most appropriate treatment?
Osseous genioplasty.
 How well does chin implantation correct vertical deficiency of the chin?
How well does chin implantation correct vertical deficiency of the chin?
It only corrects anteroposterior dimension.
 Transverse rhytids along the root of the nose are from which muscle group?
Transverse rhytids along the root of the nose are from which muscle group?
Procerus (originates from upper lateral cartilage inserting into skin/glabella).
 What is the origin/insertion of the corrugator?
What is the origin/insertion of the corrugator?
Originate along periosteum/medial orbital rim inserting into dermis of upper eyelid.
 Following a face lift, an inability to raise the upper lip on one side is due to what complication?
Following a face lift, an inability to raise the upper lip on one side is due to what complication?
Injury to the buccal branch of the facial nerve (innervates levator labii oris).
 What does injury to the cervical branch of the facial nerve manifest as?
What does injury to the cervical branch of the facial nerve manifest as?
Platysmal weakening, or an asymmetric smile.
 What must be evaluated first during a consult for chin implantation?
What must be evaluated first during a consult for chin implantation?
The patient’s occlusion.
 Fullness of the lateral orbit noted during browlift may be due to what structure?
Fullness of the lateral orbit noted during browlift may be due to what structure?
A ptotic lacrimal gland.
 What is the treatment of a ptotic lacrimal gland?
What is the treatment of a ptotic lacrimal gland?
Suspension of the gland, not resection.
 What approach is used for browlift in a 60-year-old woman with a high hairline with brow descent under the level of the supraorbital rim?
What approach is used for browlift in a 60-year-old woman with a high hairline with brow descent under the level of the supraorbital rim?
Open browlift through a hairline incision.
 What may cause resorption of the malar fat pad following rhytidectomy?
What may cause resorption of the malar fat pad following rhytidectomy?
Disruption of the branches of the angular artery; significant in malar fat pad advancement greater than 2 cm.
 What is the treatment for bone resorption following chin implantation with chin asymmetry?
What is the treatment for bone resorption following chin implantation with chin asymmetry?
Implant removal, bone graft, and sliding genioplasty.
 What is the treatment of an obtuse cervicomental angle, marked fat pads in anterior neck, subcutaneous banding, and loose redundant skin in the neck?
What is the treatment of an obtuse cervicomental angle, marked fat pads in anterior neck, subcutaneous banding, and loose redundant skin in the neck?
Removal of cervical fat and platysmaplasty.
 What is the relation of the temporal branch of the facial nerve to the superficial temporal fascia above the zygomatic arch?
What is the relation of the temporal branch of the facial nerve to the superficial temporal fascia above the zygomatic arch?
Deep to the superficial temporal fascia.
 What is the most frequent rhytidectomy complication?
What is the most frequent rhytidectomy complication?
Hematoma (0.3–8.1%).
 What are risk factors for hematoma following rhytidectomy?
What are risk factors for hematoma following rhytidectomy?
Male patients and hypertension.
 What vascular supply are the temporal scalp flap and Washio flap based on?
What vascular supply are the temporal scalp flap and Washio flap based on?
Posterior temporal branch of the superficial temporal artery.
 What does the deep branch of the supraorbital nerve innervate?
What does the deep branch of the supraorbital nerve innervate?
Central frontoparietal scalp.
 What does the superficial branch of the supraorbital nerve innervate?
What does the superficial branch of the supraorbital nerve innervate?
Central forehead and hairline.
 What supplies sensation to the temporal forehead?
What supplies sensation to the temporal forehead?
V2 and V3.
 What supplies sensation to the temporal scalp?
What supplies sensation to the temporal scalp?
The occipital nerve.
 What is the most worrisome component of a secondary rhytidectomy regarding postoperative complications?
What is the most worrisome component of a secondary rhytidectomy regarding postoperative complications?
Hairline distortion.
 How does the vascular supply of the skin flap compare in a secondary rhytidectomy?
How does the vascular supply of the skin flap compare in a secondary rhytidectomy?
Usually good or better due to the delay factor following the primary procedure; skin slough is less frequent.
 What is the mechanism of outward pseudoherniation of the buccal fat pad?
What is the mechanism of outward pseudoherniation of the buccal fat pad?
Buccopharyngeal membrane attenuation.
 What is the natural progression of Bell palsy?
What is the natural progression of Bell palsy?
85% have recovery spontaneously within 3 weeks.
 What is the description of the mandible in Pierre Robin sequence?
What is the description of the mandible in Pierre Robin sequence?
Retrognathia; normal mandibular dimensions.
 What defines microgenia?
What defines microgenia?
Maldevelopment of the mental symphysis.
 What is the likely cause of increased show of the lower incisors following genioplasty?
What is the likely cause of increased show of the lower incisors following genioplasty?
Inadequate repair of the mentalis muscle on closure; lower lip drifts downward with healing.
 What muscle supplies blood to the anterior bony segment following a horizontal genioplasty?
What muscle supplies blood to the anterior bony segment following a horizontal genioplasty?
The anterior digastric.
 What are the zones of the malar region?
What are the zones of the malar region?
Zone I: First third of the zygomatic arch and malar bone.
Zone II: Middle third of the zygomatic arch.
Zone III: Paranasal.
Zone IV: Posterior third of the zygomatic arch.
Zone V: Submalar region.
 What is the largest zone?
What is the largest zone?
Zone I.
 Which malar zones are rarely augmented in aesthetic surgery?
Which malar zones are rarely augmented in aesthetic surgery?
Zone III and zone IV.
 What is the appearance with zone V malar augmentation?
What is the appearance with zone V malar augmentation?
Midface fullness, rounded appearance of the cheeks.
 What is the management of an anterior platysmal band?
What is the management of an anterior platysmal band?
Plication in the midline.
 What is the most important factor in facial reanimation following trauma?
What is the most important factor in facial reanimation following trauma?
Length of time between injury and reconstruction; facial muscles are viable for 2 years following paralysis; after 2 years, free muscle transfer is required.
 What is the appropriate amount of tooth show in repose?
What is the appropriate amount of tooth show in repose?
2-mm upper incisor show (may be 4 mm in women). Lower incisors should not show in repose.
 What is the most commonly injured nerve during rhytidectomy?
What is the most commonly injured nerve during rhytidectomy?
Great auricular nerve.
 What is the MACS lift?
What is the MACS lift?
Minimal access cranial suspension. A short scar rhytidectomy technique in which the SMAS is purse-string sutured to the deep temporal fascia above the zygomatic arch using a vertical vector.
Body Contouring
 When do serum lidocaine concentrations peak postoperatively?
When do serum lidocaine concentrations peak postoperatively?
Approximately 12 hours.
 How do you increase graft survival in autologous fat grafting?
How do you increase graft survival in autologous fat grafting?
Maximize surface area contact between fat graft and vascularized bed. Minimize the amount of fat injected per pass.
 What is the safe dose of lidocaine when used in tumescent solution for liposuction?
What is the safe dose of lidocaine when used in tumescent solution for liposuction?
35 mg/kg.
 What diagnosis should be considered with disorientation after massive weight loss surgery?
What diagnosis should be considered with disorientation after massive weight loss surgery?
Wernicke–Korsakoff encephalopathy from thiamine deficiency, which can be present from malnutrition of massive weight loss. Treat with intravenous thiamine.
 What cosmetic procedure is associated with the highest incidence of venous thromboembolic events (VTE)?
What cosmetic procedure is associated with the highest incidence of venous thromboembolic events (VTE)?
Abdominoplasty.
 What is the most common complication of brachioplasty?
What is the most common complication of brachioplasty?
Hypertrophic scarring in as many as 40% of patients.
 Numbness of the anterolateral thigh after abdominoplasty is due to what complication?
Numbness of the anterolateral thigh after abdominoplasty is due to what complication?
Injury to the lateral femoral cutaneous nerve (becomes superficial 10 cm below the anterior superior iliac spine).
 What is the course of the lateral femoral cutaneous nerve?
What is the course of the lateral femoral cutaneous nerve?
Arises from L2–3, passes 1 cm medial to the ASIS, superficial to the sartorius, and branches anteriorly and posteriorly.
 What does the genitofemoral nerve innervate?
What does the genitofemoral nerve innervate?
Sensation to skin of scrotum, mons pubis, labia, and over the superior portion of the femoral triangle.
 What does the iliohypogastric supply?
What does the iliohypogastric supply?
Sensation to the skin of the lateral buttocks and abdomen above the pubis.
 What does the ilioinguinal nerve supply?
What does the ilioinguinal nerve supply?
Sensation to the superomedial thigh and scrotum or mons pubis.
 The obturator nerve?
The obturator nerve?
Skin of the medial and lower thigh.
 With tumescence during suction lipectomy, what percentage of total blood loss is to be expected of the total aspirate?
With tumescence during suction lipectomy, what percentage of total blood loss is to be expected of the total aspirate?
1%.
 The wet technique?
The wet technique?
This technique utilizes 300 mL of fluid per region—25% blood in the aspirate.
 Complications from smoking arise in what percentage of patients undergoing abdominoplasty?
Complications from smoking arise in what percentage of patients undergoing abdominoplasty?
50%.
 In addition to contour irregularities, UAL is likely to cause what complication more frequently than SAL?
In addition to contour irregularities, UAL is likely to cause what complication more frequently than SAL?
Thermal injury.
 A 1:1 infiltrate to aspirate ratio during liposuction indicates which technique?
A 1:1 infiltrate to aspirate ratio during liposuction indicates which technique?
Superwet.
 What defines tumescent technique during liposuction?
What defines tumescent technique during liposuction?
2 to 3 cc wetting solution/1 cc of aspirate.
 What is the wet technique?
What is the wet technique?
Injecting 100 to 300 cc of wetting solution per area regardless of the amount of aspirate removed.
 What specific technique has been shown to decrease the recurrence rate in thigh lifts?
What specific technique has been shown to decrease the recurrence rate in thigh lifts?
Superficial fascial system suspension; anchoring skin flap to Colles fascia.
 What is the most likely cause of death following liposuction?
What is the most likely cause of death following liposuction?
Thromboembolism; followed by abdominal wall perforation, anesthetic complication, infection.
 In a patient returning several days after liposuction with clear gray fluid from incisions, erythema, and early sepsis, what is the most appropriate management?
In a patient returning several days after liposuction with clear gray fluid from incisions, erythema, and early sepsis, what is the most appropriate management?
Surgical debridement of involved tissues. Necrotizing fasciitis is a rapidly progressive soft-tissue infection that occurs in 0.4 per 100,000 patients following liposuction.
 What is the most frequent chronic complication following brachioplasty?
What is the most frequent chronic complication following brachioplasty?
Scar widening.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


