Chapter 19
Hair and Scalp
OVERVIEW
- Hair grows in a cyclic manner.
- Hair loss or alopecia may be scarring or non-scarring, resulting in permanent loss of hair follicles. It may be generalised or localised, with or without inflammation.
- Androgenetic alopecia is the most common cause of hair loss and affects men and women. Topical, oral and surgical therapies can provide benefit.
- Common types of non-scarring alopecia include androgenetic alopecia, alopecia areata, telogen effluvium and tinea capitis.
- Scarring alopecia is less common and maybe divided into lymphocytic and neutrophilic disorders.
- Hair treatments and styling can result in scarring alopecia.
- Excess or diminished growth of hair may indicate underlying disease.
Introduction
Human hair plays a significant role in the self-image of individuals and the image they present to the world. Healthy hair conveys a sense of well-being, vitality and youthfulness and as such it cannot be overestimated how devastating diseases affecting this vital organ can be. Excess hair growth in females, particularly in prominent sites such as the face, is not only an embarrassment but may indicate underlying systemic disease.
Hair cycle
Hair is a modified type of keratin and is produced by the hair matrix, which is equivalent to the epidermis. Three types of hair occur in humans.
- Lanugo hair covers the foetus in utero and is normally shed before birth. This is long and silken.
- Vellus hair covers the whole body (sparing the palms and soles only) and is short, fine and non-pigmented.
- Terminal hair is limited to the eyebrows, lashes and scalp until puberty; following puberty secondary terminal hair develops in the axillae, pubic region and on the central chest in men in response to androgens. It is coarser than vellus hair and tends to be darker and longer.
The hair follicle is unique among epidermal structures in that it grows in cycles (Figure 19.1). There are three phases.
- Anagen—the active growth phase, which typically lasts 1000 days depending on predetermined genetic factors (as opposed to body hair which lasts from 1 to 6 months).
- Catagen—the short growth arrest phase, of approximately 10 days.
- Telogen—the resting phase, lasting approximately 100 days irrespective of location.
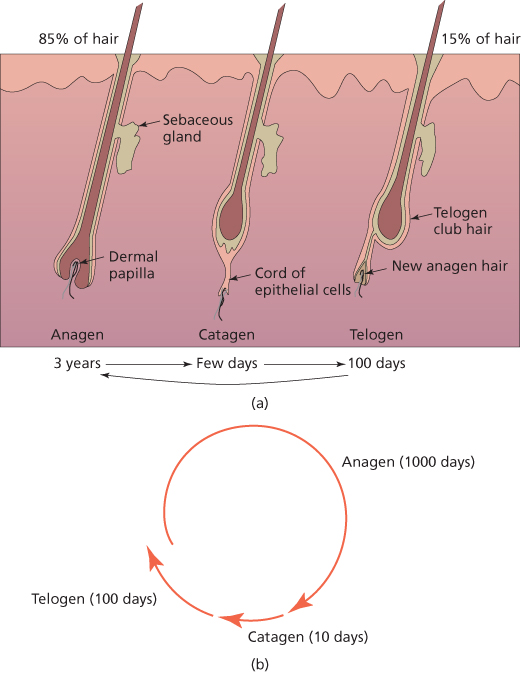
Figure 19.1 (a) Diagrammatic cross-section of hair at various growth phases. (b) Hair growth cycle.
The ratio of anagen to telogen hairs is 9:1 reflecting the fact that only a few hairs at a time are in catagen phase. On average, 100 hairs are shed per day although seasonal variation does occur.
Hair loss
Hair loss or alopecia can be divided into scarring and non-scarring types depending on the underlying pathological process, and these can then be further categorised according to distribution, either diffuse or localised.
Non-scarring alopecias
Androgenetic alopecia
Androgenetic alopecia (AGA) is synonymous with male-pattern baldness and is the most prevalent form of hair loss, affecting about 50% of Caucasian males to some extent by the age of 50. It also affects a significant number of women and is synonymous with female pattern hair loss (FPHL) (Figure 19.2). It is an androgen-dependent trait, requiring a genetic predisposition, and becomes more prevalent with advancing age. It causes hair loss over the temples (fronto-temporal recession) or vertex in men and may progress to leave a horse-shoe distribution of hair over the ears and occipital scalp. Women experience thinning over the central scalp, often presenting with a widening of their parting. In contrast to men, there is usually preservation of the frontal margin. Over time, the follicles become smaller, producing shorter and finer hairs.

Figure 19.2 Female androgenetic alopecia.
The more potent androgen, dihydrotestosterone (DHT), formed by the action of 5α-reductase on testosterone is the main driver of hair loss, particularly in men. Circulating levels of androgens are often within the normal range in both sexes, however. In some premenopausal women, there may be other signs of androgenisation suggesting gonadal (e.g. polycystic ovarian syndrome) or rarely adrenal disorders and elevated circulating androgens maybe present. The diagnosis particularly in men is straightforward; however, chronic telogen effluvium and rarely diffuse alopecia areata (AA) may be considered.
There is currently no cure for AGA and few treatments have been shown to be effective. Two drugs which are currently licensed to promote hair growth in men with AGA are oral finasteride and topical minoxidil. Minoxidil provides improvement in around 60% of men after use for at least 3–6 months. Benefit may be sustained from continued use, but is lost on cessation. Finasteride is a 5α-reductase inhibitor and reduces circulating DHT levels. Daily dosing with 1 mg orally may slow hair loss and improve growth. There is a small increased incidence of sexual dysfunction, for example, impotence in men.
Minoxidil also provides benefit in FPHL. Combined oral contraceptives may increase sex-hormone-binding globulin (SHBG) levels, leading to a reduction in free testosterone. Anti-androgens such as spironolactone, flutamide and cyproterone acetate are most useful in women with hyperandrogenism, although each requires monitoring for side effects, some of which are significant. Finasteride and dutasteride may also be beneficial; however, the dose of finasteride required maybe higher than in men.
Hair transplantation is an option where medical therapy fails. It is only possible if there is an adequate donor area, which in AGA is usually the occiput or the sides of the scalp. For follicular unit hair transplantation (FUT), hair follicles are harvested by excising a strip of skin, and individual follicular units, each consisting of 1–4 hairs, are dissected out and implanted into the bald areas. Consideration should be made of future areas of loss pre-operatively, and any progressive pathology should be treated or accounted for.
Alopecia areata
AA is an organ-specific autoimmune disease, which leads to non-scarring alopecia. It affects 0.15% of the population and can affect any hair-bearing part of the body. Extensive involvement may lead to total scalp hair loss (alopecia totalis), total body hair loss (alopecia universalis) or localised hair loss along the scalp margin (ophiasis).
AA typically presents with smooth round or oval patches of non-scarring hair loss on the scalp (Figure 19.3). Exclamation mark hairs, when present, are diagnostic of AA. These characteristic hairs break at their distal point as they taper and lose pigment proximally, giving them the appearance of an exclamation mark and occur at the periphery of patches of alopecia (Figure 19.4). Nail abnormalities, predominantly pitting or roughening, may occur in association with this condition (Figure 19.5). Other organ-specific autoimmune disorders such as vitiligo and thyroiditis are occasionally associated with AA. Investigation of associated diseases is usually indicated if symptomatic.

Figure 19.3 Alopecia areata.
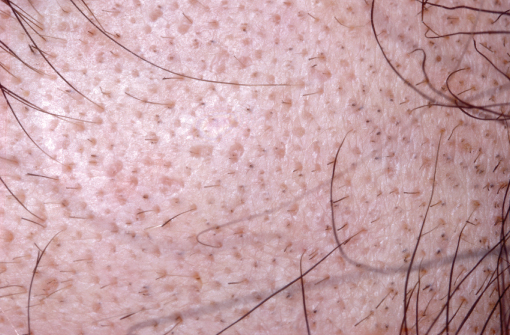
Figure 19.4 Exclamation mark hairs.

Figure 19.5 Nail pitting associated with alopecia areata.
The age of onset is usually in the first two decades. The course of AA is difficult to predict. Poor prognostic markers include
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








