Graft-versus-host disease
Get Clinical Tree app for offline access
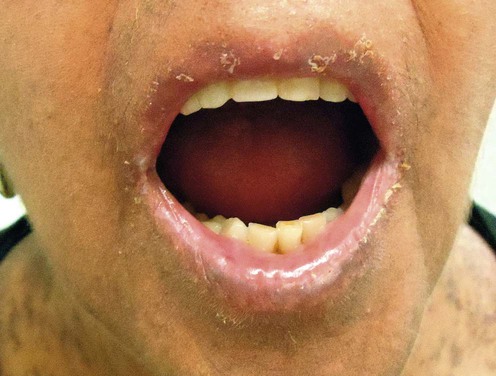
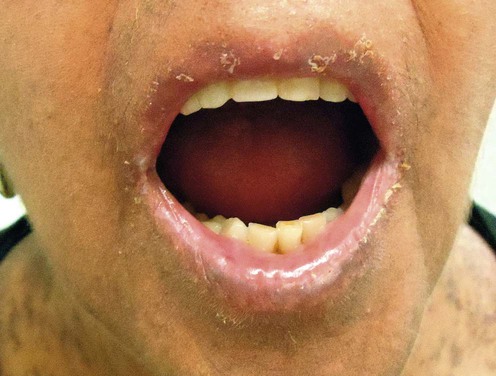
Acute gvhd
Specific investigations

Graft-versus-host disease
Get Clinical Tree app for offline access
Acute gvhd
Specific investigations
