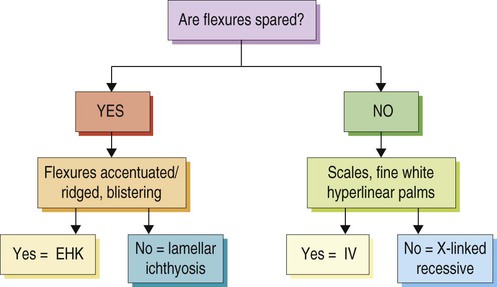
The key to management, where possible, is to establish an exact diagnosis. This provides a platform to plan therapy, discuss prognosis, and consider genetic counseling. It is important to identify the age of onset, the presence or absence of collodion membrane, blistering or erythroderma in the neonatal period, and the type, color, and distribution of scale. Family members should be examined. The Ichthyosis Support Group (ISG) provides a support network for families with resources and information sheets (www.ichthyosis.org.uk). Arin MJ, Oji V, Emmert S, Housser I, Traupe H, Krieg T, et al. Br J Dermatol 2011; 164: 442–7.
Ichthyoses

Management strategy
Specific investigations
Expanding the keratin mutation database: novel and recurrent mutations and genotype–phenotype correlation in 28 patients with epidermolytic ichthyosis.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree