64
Fungal Diseases
Key Points
Superficial Fungal Infections
Tinea (Pityriasis) Versicolor
• Secondary to transformation of Malassezia spp., especially M. furfur, from the yeast form to the hyphal form (see Fig. 2.1A).
• Malassezia spp. are part of the normal flora.
• Most commonly develops on the upper trunk and shoulders, but can also involve flexural sites such as the antecubital fossae, submammary folds, and groin (Fig. 64.1); in children more frequently than adults, there can also be facial involvement.


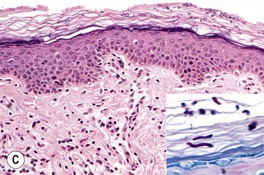
Fig. 64.1 Tinea (pityriasis) versicolor. A Hyperpigmented variant. B Hypopigmented variant on the face. C Yeast and short hyphae in the stratum corneum highlighted by a PAS stain (insert). A, B, Courtesy, Kalman Watsky, MD; C, Courtesy, Lorenzo Cerroni, MD.
• Often first noticed in the summer, and a suntan accentuates the hypopigmented variant.
• DDx: postinflammatory hypopigmentation and idiopathic macular hypomelanosis (if hypopigmented); confluent and reticulated papillomatosis of Gougerot and Carteaud (if hyperpigmented; see Chapter 89).
Tinea Nigra, Black Piedra, and White Piedra
• Typically seen in tropical areas.
– Most commonly due to infection with Hortaea werneckii, a pigmented fungus found in soil.
– Brown, sharply marginated macule or patch; most commonly on the palms (Fig. 64.2).
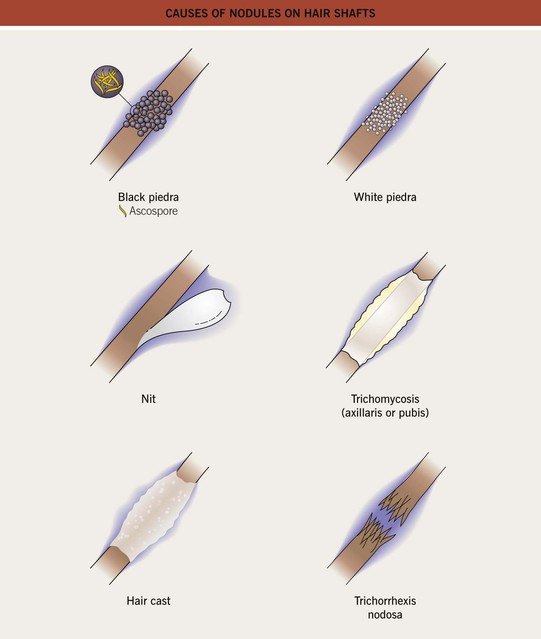
• Black piedra and white piedra are characterized by the formation of nodules on hair shafts (Table 64.2; Fig. 64.3).
Table 64.2
Comparison of black and white piedra.
| White Piedra | Black Piedra | |
| Nodule color | White (occasionally red, green, or light brown) | Brown to black |
| Nodule firmness | Soft | Hard |
| Nodule adherence to the hair shaft | Loose | Firm |
| Typical anatomic location | Face, axillae, and pubic region (occasionally scalp) | Scalp and face (occasionally pubic region) |
| Favored climate | Tropical | Tropical |
| Causative organism | Trichosporon beigelii | Piedraia hortae |
| KOH examination of ‘crush prep’ of cut hair shafts | Nondematiaceous hyphae with blastoconidia and arthroconidia (see Fig. 2.17A) | Dematiaceous hyphae with asci and ascospores (sexual reproduction) |
| Culture on Sabouraud’s agar | Moist, cream-colored, yeast-like colonies* | Slow-growing, dark green to dark brown-black colonies |
| Treatment | Clip affected hairs, wash affected hairs with antifungal shampoo | Clip affected hairs, wash affected hairs with antifungal shampoo |
* Growth inhibited by cycloheximide.
Dermatophytoses (Tinea Infections)
• The names of dermatophyte infections consist of the word ‘tinea’ followed by the Latin name for the involved body site; examples are tinea pedis (foot) and tinea cruris (groin) (Fig. 64.4).
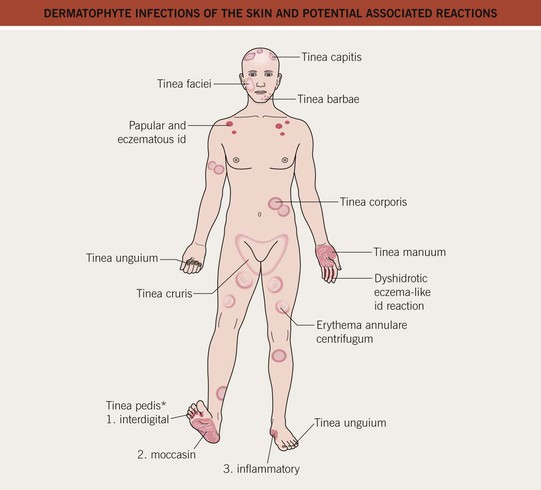
Fig. 64.4 Dermatophyte infections of the skin and potential associated reactions. *Often associated with an id reaction, particularly dyshidrotic eczema-like findings on the palms and lateral digits; papular and eczematous id may also be seen, especially in association with tinea capitis. Erythema annulare centrifugum is a reaction pattern that can be idiopathic or associated with tinea infections (see Chapter 15).
• Due to fungi of three genera – Trichophyton, Microsporum, and Epidermophyton – that invade only keratinized tissue (stratum corneum, hair, and nails).
– Trichophyton mentagrophytes has two major variants that infect the skin, which can lead to confusion; T. mentagrophytes var. interdigitale is spread human-to-human, whereas T. mentagrophytes var. mentagrophytes is acquired from animals; these variants are also known as T. interdigitale [anthropophilic] and [zoophilic], respectively.
• The classic presentation is an erythematous, annular lesion with an active, scaly border; superficial pustules may also be present (Fig. 64.5).





Fig. 64.5 Tinea corporis. A Lesions with subtle annular configuration and border composed of individual, slightly scaly papules. B Scaly concentric rings on the arm. C Extensive figurate lesions on the neck and upper chest. D Pustules within multiple figurate lesions on the upper arm. E Tinea ‘incognito’ due to use of topical corticosteroids. A, B, Courtesy, Julie V. Schaffer, MD. C, Courtesy, Kalman Watsky, MD; E, Courtesy, Julie V. Schaffer, MD.
• Occasionally, vesicles may develop, especially in tinea pedis or manuum due to T. mentagrophytes.
• Dx: KOH ± fungal culture of skin scrapings (see Fig. 2.1) as well as hairs and nails, in the case of tinea capitis and tinea unguium, respectively.
– Tinea incognito refers to atypical clinical presentations, often due to inappropriate treatment with potent topical CS or combination topical therapies that contain CS; lesions may lack scale or be minimally inflamed (Fig. 64.6; see Fig. 64.5E).
– Majocchi’s granuloma is characterized by erythematous papules or pustules within an area of tinea corporis; the papules represent sites of hair shaft invasion, usually due to T. rubrum; often seen in women with tinea pedis who shave their legs or in immunosuppressed patients (see Fig. 31.4A; Fig. 64.7).
Examples of Specific Types of Dermatophytoses
– Most commonly due to T. rubrum or T. mentagrophytes var. interdigitale > Epidermophyton floccosum.
– Three major types: (1) interdigital – erythema, scaling, and maceration in the web spaces, especially the two lateral web spaces, which have the most occlusion; can be accompanied by fissures as well as superimposed bacterial infection; (2) moccasin – diffuse scaling and erythema that extends onto the lateral aspect of the feet; and (3) inflammatory (vesicular) – vesicles and bullae, especially on the medial aspect of the plantar surface.
– Occasionally, especially in immunocompromised and diabetic patients, a more severe ulcerative toe-web infection can occur where there is both a dermatophyte and a bacterial (e.g. pseudomonal) infection; see discussion of gram-negative toe-web infection in Chapter 61.
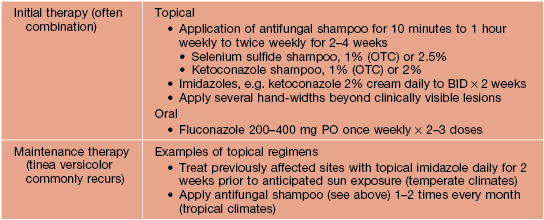
– Consider use of oral antifungal medications if the tinea pedis fails to respond to topical agents or is severe (Table 64.3).



Fig. 64.8 Tinea pedis. Diffuse scaling in the moccasin type (A), maceration between the third and fourth toes in the interdigital form (B), and erythema, scale-crust, and bullae in the inflammatory form (C). The patient in (A) also has involvement of the right hand (i.e. one hand–two feet tinea). B, Courtesy, Jean L. Bolognia, MD.
Table 64.3
Therapeutic regimens for dermatophytoses.
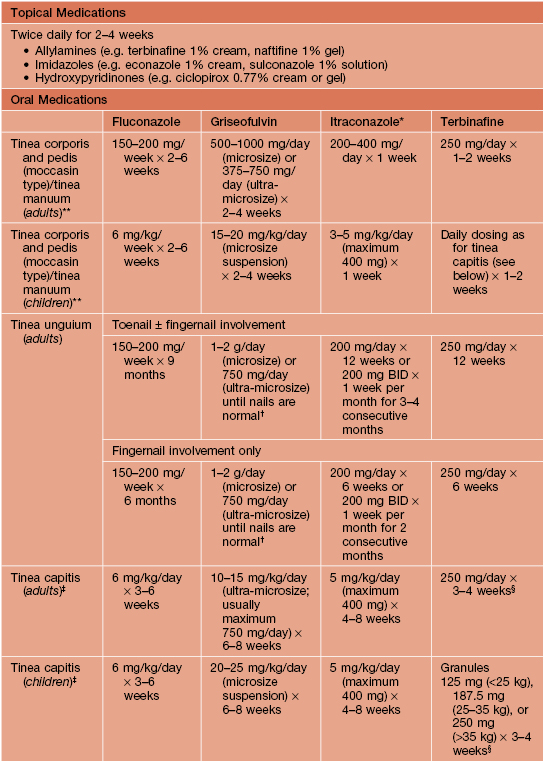
* Not approved in the United States for use in children.
** In general, the shorter courses and lower doses tend to be used for tinea corporis.
† No longer commonly used for this indication.