GENERAL PRINCIPLES
I. ANATOMY
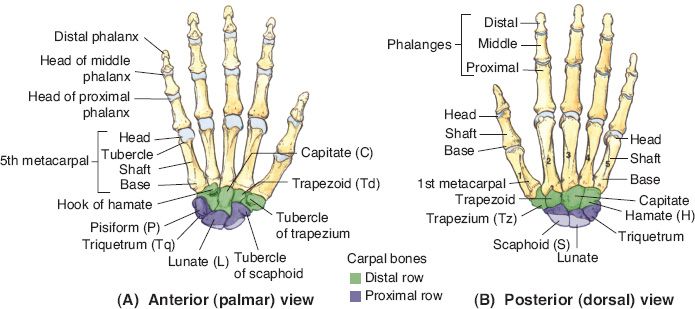
Bones of the hand and wrist depicted in Figure 39-1
II. CLASSIFICATION OF FRACTURES
A. Multiple classification schemes
1. There is at least one classification for each bone fractured in the hand and wrist
2. Most classification schemes do a poor job of easing communication between providers, providing prognosis or directing treatment
B. Universal descriptive system
1. Open versus closed
2. Fracture orientation (transverse, oblique, and spiral)
3. Anatomic location (base, shaft, neck, head, condyle, and articular involvement)
4. Displacement (degree of rotation, angulation, and shortening)
5. Level of comminution
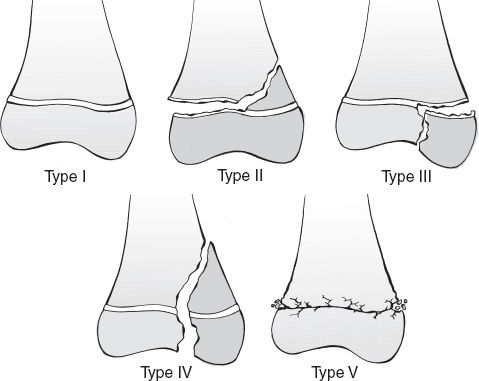
C. Salter–Harris classification of pediatric physeal fractures (Fig. 39-2)
1. Type I: Fracture through the physis
2. Type II: Fracture through the physis and metaphysis
3. Type III: Fracture through the physis and epiphysis
4. Type IV: Fracture extends from the metaphysis, through the physis and into the epiphysis
5. Type V: Physeal crush injury
6. *The amount of injury to the growth plate and possible growth disturbance increases as one increases from type I to V
Figure 39-1. Bones of the hand and wrist. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
______________
*Denotes common in-service examination topics
Figure 39-2. The Salter–Harris classification of pediatric physeal fractures. As the injury goes up in type, there is greater injury to the physis and greater chance of growth disturbance. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
III. TREATMENT
A. Affected by the displacement, the stability of the fracture pattern, and the location of fracture
B. Goals of treatment
1. Anatomic reduction
2. Appropriate immobilization
3. Maximizing the range of motion (ROM) following healing
C. Treatment options
1. Closed reduction and splint/cast immobilization: Works well for stable fracture patterns that are easily reduced and remain anatomically aligned, but requires longer immobilization
2. Closed reduction and percutaneous fixation (“Pinning”)
a. Works well for unstable fracture patterns that are easily reduced, also requires longer immobilization
b. Pinning can actually be technically difficult sometimes
c. Can occasionally result in pin-tract infections
3. Open reduction and internal fixation
a. Works well for comminuted fractures
b. Difficult to reduce fractures and in the polytrauma extremity
c. Is technically more demanding with little margin for error in alignment
d. Main benefit is early active ROM
e. Main tradeoff is increased edema and predisposition to stiffness
4. External fixation
a. Works well for open fractures with significant contamination and periarticular fractures with significant comminution
b. Can result in sensory neuritis and pin-tract infections
IV. POSTOPERATIVE CARE
A. Length of immobilization
1. Depends on fracture pattern, location and stability
2. Depends on treatment (open reduction and internal fixation [ORIF] < closed reduction and percutaneous pinning (CRPP))
3. Most fractures are stable enough for activity by 8 weeks
4. Wean patients from splint usage to slowly increase the stress on the fracture site
B. Assessment of healing
1. Serial X-rays (assessment of fracture callus or resolution of fracture lucency)
2. Physical examination (loss of tenderness over fracture site reflects bony union and precedes X-ray changes)
V. THERAPY AND FURTHER INTERVENTIONS
A. Therapy (with a certified hand therapist, physical therapist or occupational therapist) after immobilization or operative intervention is often of value to regain ROM
B. Progression of activity from gentle active to passive ROM to strengthening programs
C. Patients should maximize their outcomes from therapy prior to contemplating further procedures (i.e., tenolysis, capsulotomies, etc.)
D. Preoperative counseling is paramount to control expectations on final result
FRACTURES
I. PHALANGEAL FRACTURES
A. Epidemiology
1. Fairly common: Along with metacarpal fractures, account for 10% of all fractures
2. Most commonly in the second to fifth decades of life
B. Evaluation
1. Assess for ROM, malrotation (scissoring), extension/flexion lag, swelling, and tenderness
2. Concern for any hand fracture or injury requires hand X-rays with three views
C. Distal phalanx fractures
1. Most common hand fracture
2. Thumb and middle finger (MF) most common
3. Tuft fractures
a. Usually a result of a crush injury with nail bed laceration
b. *Subungual hematomas should be drained for symptomatic relief (when hematoma involves ≥50% of nail bed, then should perform nail plate removal and laceration repair)
c. Comminuted fractures may result in a nonunion, but are asymptomatic
d. Consider K-wire fixation if fracture is more than one-half of bone length
e. Immobilization rarely indicated for more than 3 weeks and should exclude proximal interphalangeal joint (PIPJ)
4. Shaft fractures
a. Nondisplaced fractures are usually stabilized by adjoining soft tissue and can be treated nonoperatively
b. Displaced transverse fractures are usually open due to laceration in nail bed: Can be treated with a longitudinal K-wire and nail bed repair
5. Epiphyseal fractures
a. Often missed, which can result in a foreshortened digit in children
b. *Eponym for Salter–Harris I fracture of distal phalanx = “Seymour fracture”
c. Injury may manifest as an open mallet deformity: Apex dorsal angulation due to the extensor terminal tendon attached to epiphysis and flexor digitorum profundus (FDP) attached to the distal segment
d. Treatment requires debridement, fracture reduction ± pinning, and nail bed repair
6. Dorsal articular fractures of distal phalanx (Mallet fractures)
a. Caused by hyperextension
b. Avulsion fracture of extensor tendon insertion
c. Treatment
i. Splinting in extension for 6 to 8 weeks
ii. ORIF: For fractures with volar subluxation and for larger fragments that involve >30% of articular surface
7. Volar articular fracture (profundus avulsion)
a. Most common in ring finger
b. Occurs when finger is forcibly extended while profundus is maximally contracted
c. *Classification (Leddy and Packer)
i. I: Tendon retracts into palm proximal to A1 pulley—tendon reinsertion and splinting
ii. II: Tendon retracts to proximal interphalangeal (PIP) level—tendon reinsertion and splinting
iii. III: Large bony fragment retained at A4 pulley—ORIF of bony fragment
iv. IIIA: Simultaneous avulsion of FDP from fractured fragment—tendon reinsertion and ORIF of bony fragment
D. Middle/proximal phalanx fractures
1. Fractures that are stable and nondisplaced can be treated with “buddy taping” or a short course of immobilization
2. Outcomes influenced by many factors, including patient age, motivation/compliance, associated injuries, length of immobilization, and articular involvement
3. Evaluate for angulation or malrotation
4. Digits should be immobilized 4 weeks or less to maximize motion
5. Articular fractures
a. Condylar fractures
i. Inherently unstable; err on the side of operative intervention
ii. Benefit from transverse K-wire fixation or lag screw placement
iii. Bicondylar or comminuted fractures often require ORIF
iv. PIPJ stiffness is a frequent result, so early motion is key
v. Technical points
a) Reduction can be held with a towel clip for CRPP
b) Open approach should be between lateral band and central tendon
c) Preserve the central tendon and collateral ligament attachments
vi. Pitfalls: One screw or pin may lead to rotation, two points of fixation preferred
b. Comminuted head fractures
i. Extensively comminuted head fractures are associated with soft-tissue injury that is best treated nonoperatively
c. Base fractures
i. Often result from avulsion of central tendon or collateral ligaments
ii. Stable joints can be treated nonoperatively
iii. Significantly displaced corner fracture may be unstable, requiring ORIF
iv. Comminuted pilon fractures can be treated with skeletal traction or ORIF
6. Nonarticular fractures
a. Neck fractures
i. Usually seen in children
ii. Usually treated by reduction and splinting or K-wires
iii. When fractures cannot be reduced closed, need open reduction, usually from dorsal approach
b. Shaft fractures
i. Can have varied anatomy: Transverse, oblique, spiral, and comminuted
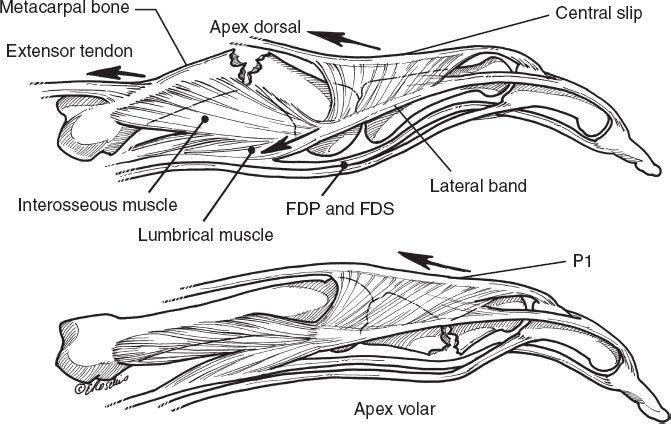
ii. Proximal phalanx fractures often have apex volar angulation based on intrinsic pull (Fig. 39-3)
iii. Stable fractures are treated with intrinsic-plus splinting (metacarpophalangeals [MPs] flexed and interphalangeals [IPs] extended) and then buddy taping
iv. Unstable fractures require fixation with K-wires, lag screws, or mini-plate
7. Complications
a. Malunion
b. Nonunion
c. PIPJ extensor lag
d. Infection
Figure 39-3. Classic deformities of metacarpal and proximal phalanx (P1) shaft fractures, due to forces of adjacent tendons. Metacarpals tend to have an apex dorsal deformity and P1 fractures tend to have an apex volar deformity. FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis. (From Doyle JR, Tornetta P, Einhorn TA, eds. Hand and Wrist. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
II. METACARPAL FRACTURES
A. Epidemiology
1. Makes up 30% to 40% of all hand fractures, one-quarter of which are SF metacarpal neck fracture
2. Lifetime incidence of a metacarpal fracture is 2% to 3%
3. “Boxer fractures” rarely occur in actual boxers and are a result of poor form
B. Evaluation
1. Assess for ROM, malrotation (scissoring), extension/flexion lag, swelling, and tenderness
2. Concern for any hand fracture or injury requires hand X-rays with three views
3. No prospective studies comparing nonoperative with operative fixation
C. Metacarpal head fractures
1. Rare and usually intra-articular
2. Most commonly the index finger due to the immobile carpometacarpal (CMC) joint
3. >25% of articular surface or >1 mm of step off warrant operative intervention
4. *“Fight bite”: Open fractures due to a clenched fist injury, require operative debridement
D. Metacarpal neck fractures
1. Common fracture when clenched MP joint strikes a solid object
2. Cause little functional deficit in the absence of “pseudoclawing” or malrotation
3. *Mobility of CMC joint and metacarpophalangeal (MCP) hyperextension allows for residual deformity to be tolerated
a. <15 degrees tolerated in the index and middle fingers
b. Up to 30 to 40 degrees tolerated in the ring finger and up to 45 to 60 degrees tolerated in the small finger
4. Treated with closed reduction and immobilization versus CRPP based on the degree of angulation and stability of attempted reduction
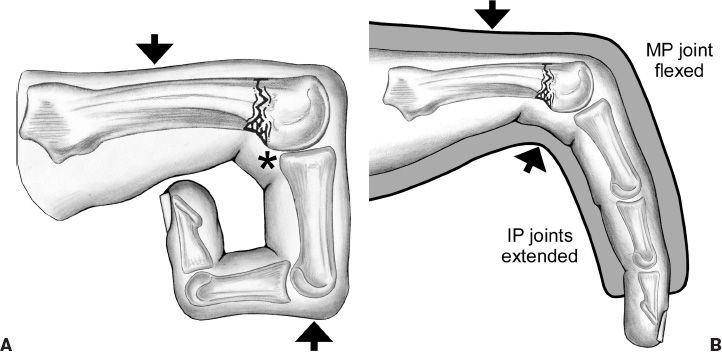
5. Jahss maneuver: Used to reduce metacarpal neck fractures, by passively flexing the MP and IP joints to 90 degrees and pushing metacarpal head dorsally to counteract the apex dorsal displacement (Fig. 39-4)
Figure 39-4. A: Schematic of the Jahss maneuver for closed reduction of metacarpal neck fractures. B: Schematic of cast immobilization of a metacarpal neck fracture. *indicates the site of reduction. Note the position of the interphalangeal (IP) joints. MP, metacarpophalangeal. (From Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
E. Metacarpal shaft fractures
1. Types of fractures
a. Transverse fractures: Angulate the apex dorsal due to forces from interosseous muscles (Fig. 39-3)
b. Oblique: Due to torsional forces, can lead to malrotation
c. Comminuted: Direct impact, can lead to shortening
2. Treatment
a. Reduction and immobilization: Works well for most shaft fractures, wrist in 30 degrees of extension, MP joints flexed >80 degrees, and IP joints extended
b. CRPP
i. Can be antegrade or retrograde, but may interfere with extensor tendons
ii. Should be in place at least 4 weeks in adults
c. ORIF
i. Can be done with plate/screws (≥2 mm) or with lag screws (long oblique fractures)
ii. Need to start active range of motion (AROM) at first post-op to prevent adhesions/stiffness
3. Operative indications
a. Open fractures: Need thorough debridement and fixation
b. Multiple fractures: Difficult to obtain acceptable reduction with adjacent fractures
c. Unstable fractures: Particularly true in border digits
d. Malalignment: Malrotation is poorly tolerated as it is magnified distally, some sagittal angulation tolerated (30 degrees in RF and SF, 10 to 20 degrees in index finger and MF)
e. Significant shortening: Opinions vary, but >3 mm of shortening believed to result in intrinsic dysfunction
F. Metacarpal base fractures
1. Index, middle, and ring finger MC base fractures
a. Rarely given lack of motion at these CMC joints, usually avulsion injuries
b. Can usually be treated nonoperatively
2. Small finger fracture dislocation of the CMC
a. Relatively common given mobility of CMC and unprotected location of SF
b. Relatively unstable with usual dorsal and proximal subluxation of the metacarpal due to the deforming force of the ECU insertion
c. Eponym is “Baby Bennett” or “reverse Bennett’s fracture”
d. Usually requires closed reduction and K-wire fixation
G. Thumb metacarpal fractures
1. Extra-articular: Usually at mid-shaft or epibasal
a. Usually apex dorsal, with distal fragment adducted and flexed due to pull of adductor, abductor pollicis brevis, and flexor pollicis brevis
b. Usually treated nonoperatively with thumb spica cast
c. Can tolerate up to 30 degrees of deformity due to motion at CMC joint
2. Intra-articular fracture
a. *Bennett’s fracture: Two-piece intra-articular fracture dislocation
i. Single volar–ulnar fracture fragment remains due to anterior oblique ligament, abductor pollicis longus pulls on metacarpal base radially, proximally, and dorsally
ii. Usually treated with CRPP
iii. Reduction performed by longitudinal traction, pressure at thumb metacarpal base, and pronation
b. Rolando fracture—Comminuted fracture of the base of the thumb metacarpal. Usually requires ORIF with plate and screws to restore articular surface
H. Complications
1. Malunion: Malunion may result in loss of “knuckle” which is unaesthetic, pseudoclaw with digital extension, or palmar prominence which may be painful with grasping
2. Infection
3. Nonunion: Uncommon in closed injuries
4. Tendon adhesions: Usually a result of ORIF
5. Intrinsic muscle dysfunction: Can result from significant shortening
III. SCAPHOID FRACTURES
A. Epidemiology
1. *71% of all carpal bone fractures
2. Common in young to middle-aged men—age 15 to 60 years
3. 10% affect proximal pole, 70% waist, 10% through distal pole
B. Pertinent anatomy
1. Shape: Mostly covered in articular cartilage; Greek “skaphos” meaning “boat-shaped”
2. Articulations: Spans both carpal rows, thus having less mobility; articulates with trapezium, trapezoid, radius, lunate, and capitate
3. *Blood supply
a. Superficial palmar and dorsal carpal branches of radial artery feed distal pole of scaphoid
b. Intraosseous vessels flow retrograde to supply proximal pole
c. Fractures through scaphoid waist can compromise blood supply to the proximal pole: This leads to avascular necrosis (AVN) of proximal fragment in as many as one-third of cases
C. Evaluation
1. Physical exam
a. Anatomic snuffbox tenderness is highly sensitive (∼90%) but nonspecific
b. Watson test (tenderness with volar pressure at distal tubercle while moving the wrist from ulnar to radial deviation) is more specific
c. Scaphoid flexes with wrist flexion and radial deviation.
2. Imaging
a. Wrist X-rays: Standard films with a “scaphoid view” (PA with wrist in ulnar deviation)
b. Computed tomography (CT) scan: More sensitive than X-rays for scaphoid fractures. Useful in assessing bony union in postoperative period
c. Bone scan: Can pick up occult fractures within 72 hours of injury, more cost effective than CT and magnetic resonance imaging (MRI) but little anatomic detail
d. MRI: Beneficial in picking up occult fractures and bony contusions, as well as assessing proximal pole vascularity. Also evaluates ligamentous injuries.
D. Management
1. All suspected injuries should be placed in a thumb spica splint/cast to prevent displacement and minimize the nonunion potential
2. If exam is concerning but X-rays are negative, examine again in 10 to 12 days with repeat films
3. Distal pole fractures
a. High union rate
b. Can be treated with a short-arm cast for 6 to 8 weeks
4. Nondisplaced waist fractures
a. Nonoperative treatment—12 weeks of immobilization, or until CT evidence of union (6 weeks long arm thumb spica, 6 weeks short arm) will lead to ∼90% union rate
b. ORIF: Preference for early ROM, high-demand occupation
5. Proximal pole fractures. *There is consensus that these CANNOT be treated nonoperatively reliably due to high nonunion rates (approaching 90%); ORIF
6. Unstable fractures warrant ORIF
Be wary of
a. >1 mm of displacement
b. Humpback deformity—>35 degrees intrascaphoid angle and usually require volar approach.
c. Comminution
d. Perilunate fracture–dislocation
E. Complications
1. Nonunion
a. Defined as a failure to heal after 6 months
b. Risk factors include proximal pole fractures, delay in diagnosis >4 weeks, displaced fractures
c. Will lead to scaphoid nonunion advanced collapse wrist and arthritis
d. Treatment—ORIF with bone grafting if no signs of arthritis, otherwise salvage procedures such as proximal row carpectomy, subtotal wrist fusion, and total wrist fusion
2. Malunion
a. Usually heals with apex dorsal angulation (humpback deformity)
b. Leads to dorsal intercalated segmental instability and arthritis
3. AVN
a. Occurs commonly in proximal pole fractures, which is why ORIF is usually indicated
b. Appears as sclerosis of proximal fragment on X-ray
c. *MRI is the most sensitive and specific test
d. Treatment—Vascularized bone grafting if no signs of arthritis (1,2 intercompartmental supraretinacular artery flap versus free medial femoral condyle versus pronator quadratus flap)
4. Posttraumatic arthritis
a. Results from malunion and nonunion
b. Treated with salvage procedures such as proximal row carpectomy, four-corner fusion, and total wrist fusion
IV. OTHER CARPAL FRACTURES
A. Rare injuries, representing 1% to 2% of all fractures
B. Usually a result of a fall on outstretched hand
C. Lunate
1. Incidence is 1% to 6% of all carpal fractures (6% includes cases of Kienbock’s disease)
2. Mechanism usually is hyperextension of the wrist
3. 50% have concomitant fractures of radius, capitates, and metacarpals
4. Diagnosis requires high index of suspicion: Plain radiographs may not show fracture, but CT/tomography will
5. Treatment
a. Nondisplaced: Cast immobilization
b. Displaced—ORIF
6. Kienbock’s disease
a. Collapse of lunate from AVN: Lunatomalacia
b. Etiology remains uncertain
c. Males 18 to 40 years old involved in heavy labor are most commonly affected
d. Likely multifactorial, with repetitive microtrauma, mechanical predisposition, vascular factors all playing a role
e. Natural history involves fragmentation, collapse, carpal malalignment, and arthrosis
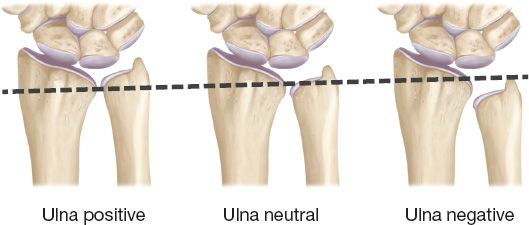
f. Ulna minus variance
i. Hulten (1928) found that 78% of 23 patients with Kienbock’s had ulna minus variance compared with 23% of 400 normal wrists
ii. Meta-analysis by Chung (2001) reports that insufficient data exist to make this conclusion
g. Diagnosis
i. Symptoms include pain, swelling, and weakness of grip
ii. Specific severe trauma is usually absent, but some form of injury usually described
iii. X-ray: Collapsed lunate, carpal instability (capitolunate collapse), and ulna minus variance
iv. CT, MRI more sensitive
h. Treatment
i. Stage 1: Cast immobilization ± NSAIDs (nonsteroidal anti-inflammatory drugs) for 1 to 3 months
ii. Stage 2: Cast trial, but surgery is more frequent given lunate fracture
iii. Stage 3: Radial shortening or ulnar lengthening versus scapho-trapezial-trapezoidal fusion versus vascularized bone grafting
iv. Stage 4: Radiocarpal or total wrist arthrodesis
D. Triquetrum
1. *Most common carpal bone fracture after scaphoid
2. Majority are dorsal cortical fractures treated with immobilization × 4 to 6 weeks
3. Mechanism is impaction/hyperextension injury in ulnar deviation
E. Trapezium
1. Usually from a fall onto the thumb with compression of trapezium by the metacarpal base
2. Require ORIF
F. Capitate
1. Can be isolated, but more commonly are a part of a greater arc injury
2. Scaphocapitate fracture syndrome: Trans-scaphoid trans-capitate perilunate fracture dislocation, often resulting in 180 degrees rotation of proximal capitates and possible AVN
V. DISTAL RADIUS FRACTURES
A. Epidemiology
1. Distal radius fractures (DRFs) are the most common fracture in the human body
2. Bimodal distribution of the injury, with young males suffering high energy injuries and elder females suffering osteoporotic fractures from falls on outstretched wrists (FOOSH)
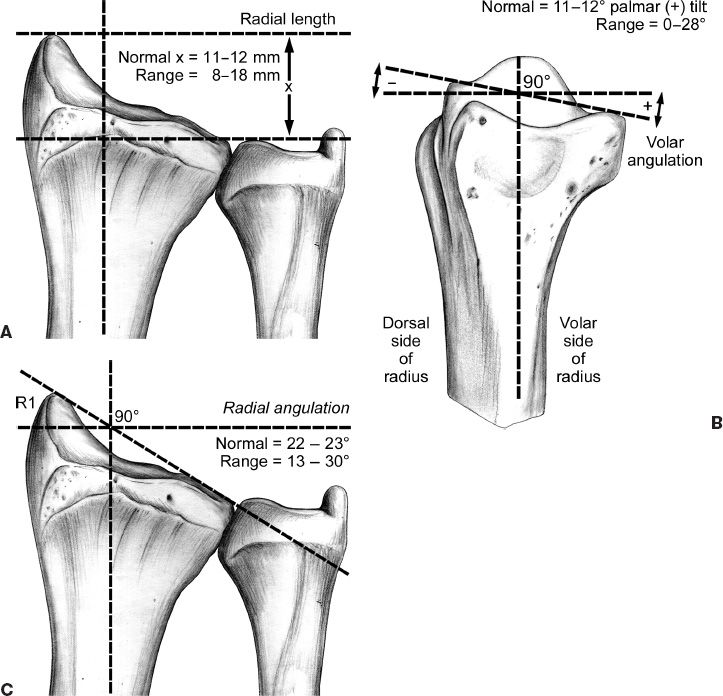
Figure 39-5. Measurement of normal uninjured radiographic landmarks of the distal radius. A: Radial length. B: Palmar tilt. C: Radial angulation. (From Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
3. Accounts for 17% of all fractures treated in emergency department (ED) and 75% of forearm fractures
4. Most commonly occurs in patients aged 6 to 10 years and 60 to 70 years
B. Anatomy
1. Distal radius has three concave articular surfaces: Scaphoid fossa, lunate fossa, and sigmoid notch (Fig. 39-5)
2. Articular surface has a radial inclination or slope of 22 to 23 degrees on PA X-ray
3. Articular surface has a palmar or volar tilt of 11 degrees on a facet lateral X-ray
4. Ulnar variance ranges widely but average is −1 mm (Fig. 39-6)
5. Dorsal aspect of radius is convex, acting as a fulcrum for the extensors
6. Lister’s tubercle acts like a fulcrum for the extensor pollicis longus (EPL) tendon
7. Normal wrist motion
a. 120 degrees flexion/extension
b. 50 degrees radial/ulnar deviation
C. History and physical exam
1. Common history is that of FOOSH, causing compressive loading on a dorsiflexed wrist
2. Exam will show tenderness, swelling, and deformity, that is, “Dinner fork deformity”
Figure 39-6. Ulnar variance.
3. Assess for median nerve symptoms before and after reduction—concern for acute carpal tunnel syndrome
D. Radiographic evaluation
1. PA/oblique/lateral X-rays: Standard imaging for all wrist injuries. Will diagnose most distal radius fractures.
a. PA view: Radial inclination (~23 degrees); radial length (10 to 12 mm), ulnar variance, congruity of sigmoid notch and radiocarpal joint
b. Lateral view: Volar tilt (11 degrees), teardrop angle (70 degrees), extent of dorsal comminution
2. Noncontrast CT: Used sparingly to better assess articular involvement or when numerous carpal injuries
E. Classification systems and eponyms
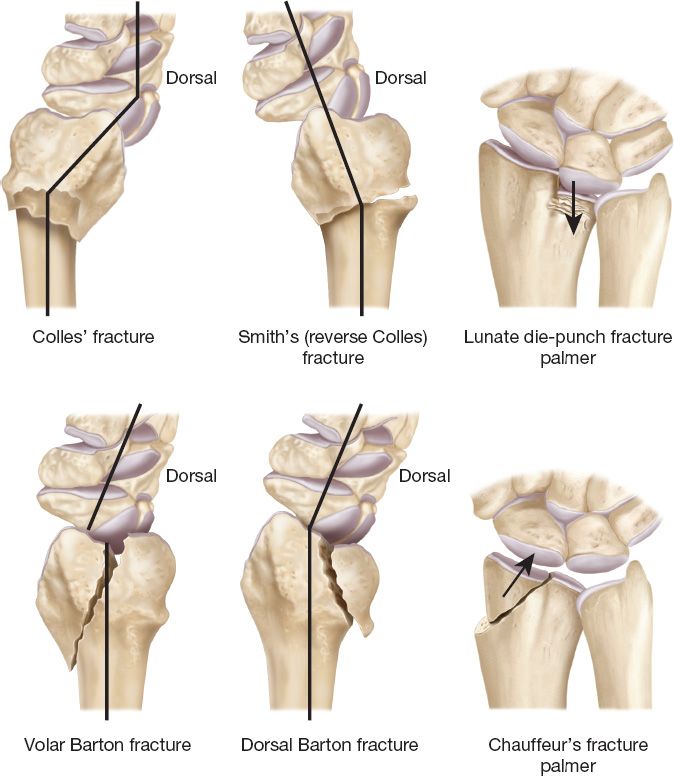
1. Eponyms: Have historical significance only (Fig. 39-7)
a. Colles’ fracture: Extra-articular fracture with dorsal comminution and apex volar deformity
b. Smith’s fracture (reverse Colles: Extra-articular fracture with apex dorsal deformity
c. Barton’s fracture: Intra-articular shear fracture, fracture–dislocation of the radiocarpal joint
d. Chauffeur’s fracture: Intra-articular radial styloid fracture, named for chauffeurs who suffered the injury due to backfires during manual crank starts
2. Classification’s systems: Many exist including AO, Frykman, Universal/Mayo, etc.
a. Systems are not universally accepted and cannot easily be related to each other
b. All available classification schemes fail in easing communication and providing prognostic information
F. Treatment
1. General principles
a. Goal is anatomic reduction to maintain wrist biomechanics
b. Stability and reduction determines treatment
c. Indications for surgery
i. Articular step-off >1 mm
ii. Radial shortening >5 mm
iii. Dorsal tilt >20 degrees
iv. Extensive comminution
v. Open fractures
2. Initial management and reduction
a. Perform hematoma block by injecting 10 cc of 1% lidocaine into fracture site from wrist dorsum; optional to give diazepam for muscle relaxation
b. Place the patient in “finger traps” and apply weight for traction (5 to 10 lb) to distract fracture; shoulder abducted 90 degrees and elbow flexed 90 degrees
c. Recreate injury mechanism to disimpact, then push distal segment in opposite direction to reduce fracture
Figure 39-7. Various types of distal radius fractures and their eponyms.
d. Place in splint; traditionally a “sugar-tong” but splint will not maintain an unstable fracture
e. Always obtain postreduction films
3. Closed reduction and immobilization
a. Greatest challenge of closed treatment is to maintain reduction, ~60% of fractures will displace in plaster
b. Good for nondisplaced or minimally displaced fractures that are well reduced
c. Should be followed by weekly X-rays to evaluate for loss of reduction. Can tolerate volar tilt of 0 to 11 degrees, radial shortening of 5 mm, articular incongruity 1 mm
d. Can be switched to a well-molded short-arm cast at 2 to 3 weeks
4. Closed reduction and K-wire fixation
a. Applicable for reducible extra-articular fractures and simple intra-articular fractures without metaphyseal comminution but with good bone quality
b. Kapandji technique: Intrafocal pinning technique where a 0.062 K-wire is used to both reduce and fix the fracture site
c. Can result in pin-tract infections, loss of reduction, or sensory neuritis
5. External fixation
a. Indicated for open fractures, impacted articular fractures, and metaphyseal fractures with significant comminution
b. Can be done with or without bridging the radiocarpal joint
c. Pins are placed via small incisions on either side of the fracture site, and fixed to external device
d. Be careful with over-distraction of fracture site, as this will lead to finger stiffness and delayed union of fracture
6. ORIF
a. ORIF is increasing in popularity due to the ease of volar plating
b. Indicated in unstable fractures, as discussed above. Argument can be made for other fracture patterns due to early return of ROM in patients after ORIF.
c. Many options including dorsal approach, fragment-specific plating, and volar locking plates
d. Volar approach: incision along the radial aspect of flexor carpi radialis tendon sheath into antebrachial fascia, sweep flexor pollicis longus out of way, and cut hockey-stick incision in pronator quadratus to expose fracture
e. Dorsal approach: Incision through floor of third extensor compartment, gives excellent intra-articular exposure
G. Associated Injuries
1. Median nerve neurapraxia: Usually improves with fracture reduction
2. Compartment syndrome—<1% of DRFs result in compartment syndrome, usually to high energy mechanism
3. Ulnar styloid fracture: Usually of little consequence, as long as distal radioulnar joint is stable; nonunions remain asymptomatic unless triangular fibrocartilaginous complex injury
4. Ligamentous injury: Can commonly injure carpal ligaments, such as scapholunate (SL) ligament
H. Complications
1. Malunion: Relatively common in comminuted fractures treated nonoperatively; can result in ulnocarpal impaction, weakness, decreased ROM; Tx with corrective osteotomy and bone grafting
2. Nonunion: Uncommon unless overdistracted in external fixator; Tx with ORIF and bone grafting
3. Tendon rupture: Most commonly an attritional rupture of EPL in the third dorsal compartment; Tx with extensor indicis proprius transfer to EPL
4. Posttraumatic arthritis: Incidence of symptomatic arthritis is unknown; but articular step off of >1 mm leads to radiographic arthritis, most of which will be asymptomatic
5. Complex regional pain syndrome
DISLOCATIONS AND LIGAMENTOUS INJURIES
I. PHALANGEAL DISLOCATIONS
A. Distal interphalangeal joint (DIPJ) dislocations
1. Usually a dorsal dislocation, secondary to a hyperextension injury
2. Treatment
a. Simple (reducible)
i. Closed reduction under metacarpal block: Extend DIPJ, then push dorsally over condyles of middle phalanx.
ii. Check X-rays to confirm joint congruity and rule out associated fracture; splint for 2 weeks
b. Complex (irreducible)
i. Open reduction is required
ii. Possible causes include interposition of the profundus tendon (implies disruption of at least one collateral ligament), volar plate, or displaced articular fracture fragment
B. PIPJ dislocations
1. Anatomy
a. Normal 100 to 110 degrees arc of rotation
b. Ligamentous stabilization
i. Lateral collateral ligaments: Insert on volar plate and volar base of middle phalanx
ii. Volar plate
a) Forms the floor of joint and is suspended by collateral ligaments
b) Prevents hyperextension of joint
c) Aids in lateral stabilization
2. Dorsal dislocation
a. More common than volar dislocation
b. Radiographs may reveal an avulsion fracture from the distal volar plate insertion site
c. Classification of dorsal dislocations
i. Type I: Partial or complete avulsion of volar plate locking middle phalanx in hyperextension
ii. Type II: Dorsal dislocation completely from middle phalanx with avulsion of volar plate and significant tear of collateral ligaments
iii. Type III: Fracture–dislocation with avulsion fracture of volar middle phalanx with volar plate
a) <40% volar articular surface: Stable
b) >40% volar articular surface: Unstable, difficult to reduce without open approach
d. Treatment
i. Closed reduction under metacarpal block, translating the middle phalanx base along the dorsum of the proximal phalanx
ii. Type I, II, and stable type III: Closed reduction with 30 degrees dorsal blocking splint or buddy taping for 3 weeks and early ROM
iii. Type III unstable: Unstable reductions are treated with a dorsal blocking splint in 20 degrees flexion greater than the angle reduction is lost
a) May require dynamic skeletal traction techniques for comminution
b) ORIF for large fracture fragments stabilizing with lag screw or K-wire
c) Volar plate arthroplasty if ORIF not possible followed by 3-week immobilization
e. Rotational deformity of the finger may suggest displacement of the middle phalanx between the central slip and lateral band
3. Volar dislocation
a. Lack of active extension of the middle phalanx against gentle resistance indicates central slip rupture
b. Radiographs may reveal avulsion fracture from the dorsum of middle phalanx (central slip insertion)
c. Treatment
i. Closed reduction with longitudinal traction and flexion at PIPJ
ii. After reduction, must assess PIPJ extension
a) If central slip intact: Immobilization with buddy taping and early ROM
b) If central slip disrupted: Treat as a central slip rupture (see Chapter 40)
4. PIPJ fracture–dislocations
a. Treatment
i. Stable PIPJ with <30% articular surface involved: Dorsal extension block splinting
ii. Unstable PIPJ and/or >30% of articular surface involved: ORIF
iii. Comminuted fractures: Volar plate arthroplasty or hemihamate arthroplasty
a. All injuries to PIPJ can cause significant joint stiffness, so early AROM is key
b. Ligamentous injuries can result in long-term instability
II. MPJ DISLOCATIONS
A. Anatomy
1. Volar plate
a. Laterally supported by deep transverse metacarpal ligament that allows stabilization to adjacent metacarpophalangeal joint (MCPJ)
b. Floor of joint as in PIP and distal interphalangeal (DIP)
2. *Cam effect: Collateral ligaments taut in flexion and lax in extension
B. Dorsal dislocations are more common; usually involve radial digits
C. Evaluation
1. Simple (reducible): Notable deformity with marked MP joint hyperextension
2. Complex (irreducible)
a. Deformity not as obvious; MP joint only slightly hyperextended
b. *Cannot be reduced, due to interposition of the volar plate or trapping of metacarpal head between lumbrical (radially) and flexor tendon (ulnarly) (aka “button-hole” effect)
D. Treatment
1. Simple dislocations
a. Closed reduction via gentle hyperextension at MCPJ followed by translation of proximal phalanx onto metacarpal head with dorsal pressure. Longitudinal traction alone may make a reducible dislocation irreducible!
b. After reduction, splinting with MCPJs in 50 to 70 degrees of flexion for a week followed by buddy taping
2. Complex dislocations: Usually require open reduction via dorsal or volar approach
a. Dorsal approach: Easier, just need to divide the volar plate longitudinally to let metacarpal head pass through it
b. Volar approach: *Beware of the digital nerve which will be pushed volarly and immediately under the skin at incision site; permits visualization of all involved structures
III. THUMB LIGAMENTOUS INJURIES
A. Ulnar collateral ligament (UCL) injury
1. Acute rupture: “Skier’s thumb”
a. Caused by forceful radial deviation of the thumb at the MCPJ
b. *Stener lesion
i. Occurs with complete UCL rupture
ii. Adductor aponeurosis becomes interposed between ligament and distal insertion site. Requires operative intervention.
2. Chronic attenuation: “Gamekeeper’s thumb”. Caused by repeated radial deviation, which results in laxity of the UCL
3. Physical exam/diagnosis
a. Tenderness along ulnar aspect of MCPJ should raise suspicion
b. *Laxity >45 degrees of radial deviation or >15 degrees in comparison to contralateral implies full UCL rupture
c. Ultrasound can be useful to evaluate partial versus complete tears
3. Treatment
a. Partial tears can be treated with thumb spica cast with ulnar deviation at MCP
b. Complete tears can be treated nonoperatively, but usually warrant operative fixation: K-wire fixation of MCPJ with slight ulnar deviation and repair of UCL with suture anchor
B. Radial collateral ligament injury
1. Much rarer injury and much less debilitating, as thumb does not need much radial stability because pinch causes stress on UCL
2. Treated nonoperatively with splint/cast
IV. CARPAL DISLOCATIONS
A. General
1. There are seven carpal bones (excluding pisiform, a sesamoid bone within the flexor carpi ulnaris tendon)
2. Wrist ligaments
a. Intrinsic ligaments
i. Connect carpal bones within a carpal row
ii. Most important are SL and lunotriquetral (LT) ligaments
b. Extrinsic ligaments
i. Connect bones between carpal rows (spans midcarpal joint)
ii. Volar extrinsic ligaments stronger than dorsal extrinsic ligaments
3. Carpal dislocations are rare, only 5% of carpal injuries
B. Kinematics
1. Wrist motion is complex and occurs primarily at radiocarpal and midcarpal interface
2. Proximal carpal row flexes with radial deviation of wrist and extends with ulnar deviation. This function is impaired with SL and LT ligament disruptions.
C. Perilunate injury
1. Occurs progressively as ligaments sequentially fail around the lunate
a. Stage I: Scaphoid fracture or scapholunate ligament tear
b. Stage II: Lunocapitate ligament tear
c. Stage III: Lunotriquetral ligament tear (dorsal perilunate dislocation)
d. Stage IV: Dorsal radiolunate ligament tear (volar lunate dislocation)
2. Greater arc injury (involves carpal fracture)
a. Combines carpal bone fracture with perilunate dislocation
b. Fractures occur as injury pattern involves an arc of greater radius around lunate that passes through surrounding osseous structures
c. Transscaphoid perilunate fracture–dislocation
i. Most common type of greater arc injury
ii. Immediate treatment: Closed reduction and splinting to minimize damage to neurovascular structures
iii. Definitive treatment: ORIF with dorsal approach for ligament repair, K-wires for maintenance of reduction of dislocation, compression screw across scaphoid
d. Transradial styloid perilunate fracture–dislocation
i. Immediate treatment: Closed reduction and splinting
ii. Definitive treatment—ORIF
3. Lesser arc injury (purely ligamentous injury)
a. Immediate treatment
i. Attempted closed reduction and splinting to minimize damage to neurovascular structures
ii. Open reduction often required in volar lunate dislocations
b. Definitive treatment
i. ORIF via combined dorsal (between third and fourth compartments) and volar (via carpal tunnel) approaches
ii. Repair volar ligament injury
iii. K-wires secure scaphoid, lunate, and capitate in their respective anatomic positions
iv. Pins remain in place for 8 to 12 weeks
c. Outcomes from surgical intervention
i. 60% of contralateral wrist motion
ii. 75% of contralateral grip strength
PEARLS
1. Describe fractures using location, fracture pattern, and displacement rather than classification schemes
2. Goal should always be for anatomic reduction, whether in ED or in operating room (OR)
3. Immobilization is necessary for fractures to heal but results in stiffness, so timing must be judicious
4. Discuss the likelihood for long-term stiffness and possible posttraumatic arthritis with the patients at initial injury, so that the patients associate it with the injury rather than the treatment
QUESTIONS YOU WILL BE ASKED
1. What structures provide stability to the PIP joint?
Lateral collateral ligaments and volar plate.
2. In a Bennett’s fracture, what tendon causes proximal migration of the thumb metacarpal?
APL.
3. What is a scaphoid humpback deformity?
Apex dorsal angulation of scaphoid after scaphoid waist fracture.
4. What is acceptable angulation of small finger metacarpal in the setting of shaft fracture?
40 to 45 degrees.
Recommended Readings
Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 2006;88(12):2687–2694. PMID: 17142419.
Hastings H 2nd. Unstable metacarpal and phalangeal fracture treatment with screws and plates. Clin Orthop Relat Res. 1987;(214):37–52. PMID: 3791758.
Henry MH. Distal radius fractures: current concepts. J Hand Surg Am. 2008;33(7):1215–1227. PMID: 18762124.
Kuo CE, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2008;33(6):998-1013. PMID: 18656780.
Medoff RJ. Essential radiographic evaluation for distal radius fractures. Hand Clin. 2005;21(3): 279–288. PMID: 16039439.
Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(5):827–832. PMID: 9763256.
Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am. 2006;31(3):359–365. PMID: 16516728.
Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH. Green’s Operative Hand Surgery. 6th ed. New York Elsevier; 2011.
< div class='tao-gold-member'>