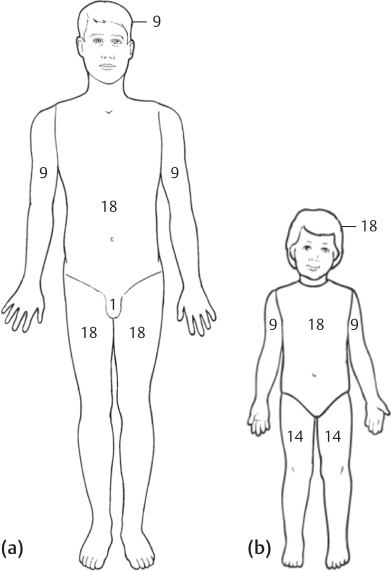
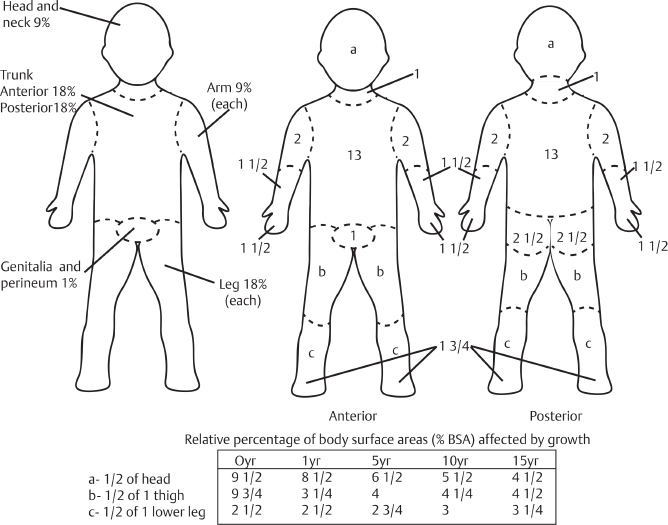
6 Fluid Management Abstract This chapter will provide information on fluid management of plastic surgery patients, with particular emphasis on liposuction. The reader will be able to plan fluid management in a variety of clinical scenarios, including liposuction, burn, and trauma. Keywords: postsurgical fluid management, liposuction, trauma, burn Six Key Points • Estimate burns by the rule of nines in adults. • Estimate burns by the Lund and Browder chart in children. • Fluid resuscitate for greater than 20% body surface area (BSA) burns. • Resuscitate using 4 mL/kg/% BSA. • Large-volume liposuction is greater than 4 L. • For liposuction, fluid ratio is tumescent volume plus intraoperative volume/aspirate. You have just performed an abdominal wall reconstruction on a 56-year-old male with a large ventral hernia. 1. What are the fluid considerations in the perioperative period? Patients undergoing surgery have both sensible and insensible losses. Sensible losses include those measurable losses such as blood and urine. Insensible losses include respiratory losses and evaporative losses. Some studies have shown that blood volume is not affected by overnight fasting prior to operative procedures.1 Sensible losses should be replaced on a demand-based regimen. Insensible losses are estimated at 0.5 to 1 mL/kg/h,2 although some authors do not advocate routine replacement of insensible losses.3 A 26-year-old male presents to the emergency department after spilling boiling water on his bilateral hands, abdomen, and thighs. 1. How do you estimate the size of a burn? Burn size is estimated based on the relative body surface area involved. In pediatric patients, the distribution of body surface area is different than for adults. Wallace’s rule of nines assigns percent body surface area in multiples of 9, in which each upper extremity is 9%, each lower extremity is 18%, the front torso is 18%, the back torso is 18%, the head is 9%, and the neck is 1% (see Fig. 6.1). In children, the Lund and Browder chart (Fig. 6.2) is often used. It stratifies children based on age (0–1, 1–4, 5–9, 10–14, and 15 years) and reflects the relative larger BSA contributions of the head and torso in the pediatric population. Fig. 6.1 The rule of 9s for estimating a burn size. (Adapted from Lakin GE. Plastic Surgery Review. New York, NY: Thieme; 2015.) 2. How do you fluid resuscitate a burn patient? Assuming that the patient has been medically stabilized according to Advanced Trauma Life Support (ATLS) guidelines, fluid resuscitation consists of administering crystalloid solution through an IV to patients who have sustained a burn greater than 20% BSA. Lactated Ringer’s solution is used for resuscitation and the Parkland formula is a tool for estimating fluid needs in the first 24 hours for an adult. • The Parkland formula is as follows: 4 mL/kg/% BSA burn. • Half of the total amount is given in the first 8 hours from the time of injury, and the second half is given over the next 16 hours. For pediatric patients, the Galveston formula is used: • 5,000 mL/m2 BSA burn + 2,000 mL/m2 total BSA. • Half of the total amount is given over the first 8 hours from the time of injury and the second half is given over the remaining 16 hours. 3. You start that fluid. How do you know it is adequate? The adequacy of fluid resuscitation is determined by urine output, which should be at least 0.5 mg/kg/h in adults and 1 mL/kg/h in children.
Questions
General
Case 1
Burn
Case 2
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine