CHAPTER 6 Femoroacetabular Osteoplasty
The possible etiologic role of abnormal hip anatomy in the development of hip osteoarthritis was described by Murray1 and Stulberg and colleagues2 in the mid-1960s and 1970s. These anomalies—the so-called pistol grip or head tilt deformities—were recognized then, but the pathophysiologic mechanism leading to osteoarthritis in these patients was not elucidated. In the mid-1980s, Harris3 also proposed a causal relationship between these deformities and primary osteoarthritis, now a disappearing term. Since the mid-1990s, it has been well recognized that gross anatomic abnormality likely results in cartilage degeneration4 through a mechanism now known as femoroacetabular impingement (FAI).5,6 FAI and its role as a prearthritic condition have been studied extensively. We currently know that gross anatomic abnormality is not a prerequisite for this condition, but that even subtle anatomic abnormalities (which often go undetected) can lead to osteoarthritis through this same pathophysiologic mechanism.7,8
CONCEPT OF FEMOROACETABULAR IMPINGEMENT AND CLINICAL PRESENTATION
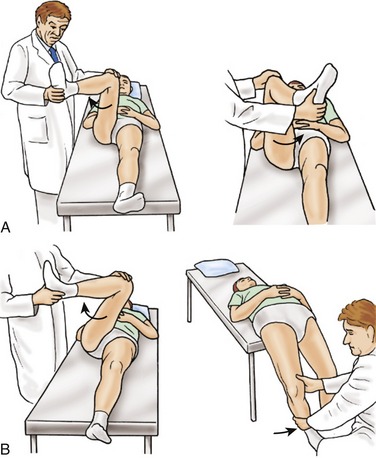
On examination, the impingement test, first described for patients with acetabular rim disorders in dysplastic hips, is often positive.9 With the hip at 90 degrees of flexion, maximum internal rotation and adduction is performed. Contact between the anterosuperior acetabular rim and femoral neck elicits pain (Fig. 6-1A). The hip is tested at varying degrees of flexion, and higher degrees usually elicit more pain. Another provocative hip test, the posterior impingement test,10 is evaluated with the patient lying with both legs dangling off the distal edge of the examination table (Fig. 6-1B). The unaffected side is flexed maximally and held within the patient’s hands. In FAI, this test is used to evaluate posterior acetabular cartilage damage. The dangled extremity is externally rotated abruptly, and the femoral head contacts the posterior acetabular cartilage and rim. If buttock pain is reproduced with this test, posterior cartilage degeneration has occurred, as can be seen in retroverted sockets with anterior FAI and a so-called contrecoup lesion.11
TYPES OF FEMOROACETABULAR IMPINGEMENT AND PATHOPHYSIOLOGY
Based on the structural abnormalities of the hip and the findings at the time of surgery, two types of FAI were initially described: cam and pincer FAI. With increasing clinical experience, we have noticed that a combined cam-and-pincer FAI is much more common—present in 80% of the hips we treat.11
Cam-type Femoroacetabular Impingement
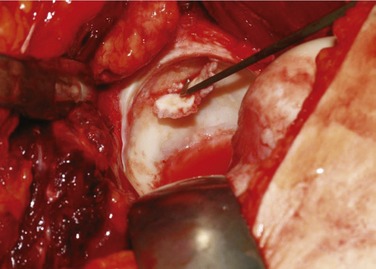
Cam-type FAI (10%)6,11–13 is more common in physically active men and in heavy laborers. These patients often have abnormally shaped proximal femurs, such as femurs with insufficient head-neck offset14,15 seen in pathologies leading to head tilt or pistol grip deformities,2,16 slipped capital femoral epiphysis,5 post-traumatic deformities, malunited femoral neck fractures,17 femoral retrotorsion, coxa vara, or femoral head necrosis with flattening.18 In these disorders, jamming of the abnormally shaped femoral head into the acetabulum with flexion and internal rotation exerts shear forces on the acetabular rim, producing an outside-in abrasion and finally avulsion of the cartilage from the subchondral bone, most commonly in the anterosuperior rim area (Fig. 6-2). The labral tear as seen on MRI is not an avulsion of the labrum, but an avulsion of the cartilage from it.
Pincer-type Femoroacetabular Impingement
Pincer-type FAI (10%) occurs in patients with abnormal acetabular morphology, (most commonly a retroverted acetabulum)19,21,22 but it is also seen in patients with coxa profunda or protrusio acetabuli. Retroversion of the acetabulum was described by Reynolds and associates.19 In these hips, the normal anterolateral opening of the acetabulum is pointed more posterolaterally in the sagittal plane. In normal hips, the anteversion progresses in a spiral from cranial to caudal. In retroverted sockets, despite normal caudal anteversion, the cranial aspect is retrotorted or is less anteverted than the normal hip (cranial retroversion). Acetabular retroversion is present in 20% of hips undergoing total hip arthroplasty (THA) for osteoarthritis and in 5% of hips in the general population.20 Retroversion of the acetabulum has also been associated with specific entities, such as Legg-Calvé-Perthes disease,22 bladder exstrophy,23 neuromuscular disorders,24 and proximal femoral focal deficiency.25 It can also be a manifestation of developmental hip dysplasia,22,26 the end result of poorly performed pelvic osteotomies,27 or traumatic closure of the triradiate cartilage in patients younger than 6 years.28
Coxa profunda and protrusio acetabuli, more commonly seen in women, lead to global overcoverage resulting in pincer-type FAI.6,11,12 This type of FAI also occurs in patients who perform activities in which the hip is placed in extreme ranges of motion. Localized or global overcoverage resulting in pincer-type FAI causes abutment between the femoral head-neck junction and the pelvic rim with range of motion, most commonly with flexion and internal rotation, but it may occur in extension and external rotation as well. In this type of FAI, the acetabular labrum fails early, and continued abutment results in labral degeneration, intrasubstance ganglion formation, or additional bone deposition at the rim of the socket (leading to worsening degrees of overcoverage). The cartilage damage in this type of FAI is more circumferential, but is usually restricted to a narrow band, most commonly malacia located in the anterosuperior acetabular rim. Continued anterior impingement can lead to posterior subluxation of the femoral head with flexion leading to damage of the posteroinferior cartilage on the acetabulum or the posteromedial cartilage of the femoral head. This contrecoup lesion has been reported to occur in 30% of acetabula and 60% of femoral heads with advanced pincer-type FAI.11
Combined Cam-and-Pincer Femoroacetabular Impingement
In practice, combined cam-and-pincer FAI (80%) is the type of FAI that is seen most commonly.11 Most of these patients have some degree of acetabular retroversion and mild-to-moderate proximal femoral abnormalities resulting in a mixed picture. Long-standing FAI usually worsens the anatomic abnormality because of additional bone deposition at the rim of the socket or in the femoral head-neck region. As the condition is diagnosed earlier, the prevalence of this type of FAI may decrease, and the isolated types may become more prevalent.
DIAGNOSTIC TESTING
Plain Radiographs
An anteroposterior pelvic radiograph provides the most information in cases of FAI. Interpretation of this radiograph is very sensitive to the position of the pelvis at the time of exposure, however.29 It is commonly accepted now that a well-centered anteroposterior pelvic view is obtained when there is symmetry of the iliac wings and of the obturator foramina and the coccyx is at a point in the midline within a distance of 0 to 2 cm above the symphysis pubis. In addition, the exposure of the film has to be good enough to show clearly the outline of the acetabulum, particularly the anterior and posterior walls, the ischial spine, the sourcil, and the lateral edge of the acetabulum.29 If a well-centered radiograph is not obtained, variations for pelvic tilt and rotation should be accounted for when observing angular measurements and acetabular version.
The abnormal anatomy of the proximal femur can be seen on the anteroposterior pelvic radiograph. The shape of the femoral head is classified as “pistol grip” if the lateral contour of the femoral head extends in a convex shape to the base of the neck, and as “aspherical” if the epiphysis of the head protrudes laterally out of a circle around the head.15 Notice should be taken of the head in the neck deformity and a high fovea, which is often combined with a head having a smaller craniocaudal diameter than the mediolateral diameter. Often the nonspherical extrusion of the head is anterolateral, and it is not always visible on anteroposterior radiographs.30
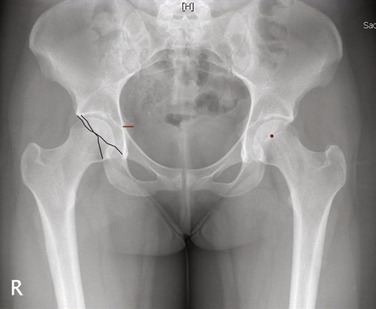
Acetabular retroversion can be recognized on a standardized anteroposterior pelvic radiograph. In the normal hip, the contours of the anterior and posterior acetabular wall edges usually meet superiorly and laterally, and this is indicative of acetabular anteversion. Reynolds and associates19 described a more distal meeting of the contours of the anterior and posterior wall edges, which they called the “crossover” sign, as indicative of acetabular retroversion (Fig. 6-3). Kalberer and colleagues31 developed the prominence of the ischial spine (PRIS) sign as a measure of acetabular retroversion. In their study, using a positive crossover sign as the gold standard for measurement of retroversion, the presence or absence of the PRIS sign as diagnostic of acetabular retroversion showed a sensitivity of 91%, specificity of 98%, positive predictive value of 98%, and negative predictive value of 92%. This study shows how the ischial spine can be used reliably as a screening tool for retroversion in patients with hip pain. The “crossover” and PRIS signs are highly sensitive, however, to radiographic pelvic tilt and rotation (see Fig. 6-3).
Coxa profunda is present when the floor of the fossa acetabuli touches the ilioischial line, and protrusio acetabuli is present when the femoral head overlaps the ilioischial line medially (Fig. 6-4).32 There are other, lesser radiographic signs that aid in diagnosing and choosing the appropriate surgical management for FAI. The posterior wall sign, which assesses posterior wall coverage, is commonly used.19,33 The visible outline of the posterior wall on the anteroposterior x-ray should lie at the level of the center of the femoral head or lateral to it. If the posterior wall sign is positive (posterior rim medial to center of head), a reorientation osteotomy (reverse periacetabular osteotomy) can be discussed as treatment for management of symptoms related to the retroversion.33
Osteophyte formation around the femoral head-neck junction seen in cam-type FAI is commonly seen as a sclerotic line in this area on the anteroposterior pelvic radiograph, and is indicative of longer standing FAI. The presence of an os acetabuli should also be noted in patients with mixed FAI because it may represent fatigue fracture with anterosuperior cartilage degeneration.34 In some patients with coxa profunda and posterior acetabular impingement, a double contour sign of the rim is often present on standard radiographs. MRI shows that this is a result of bone apposition, rather than ossification of the labrum. Fibrocystic changes (herniation pits) in the anterosuperior femoral neck junction have been reported in approximately 33% of hips with anterior FAI.35
The presence of a “crossover” sign on the anteroposterior pelvic radiograph and the presence of a bony prominence or “bump” on the anterior femoral head-neck junction on the cross-table lateral radiograph often suggest FAI.36 The presence of the “bump” on this view is highly sensitive to the position of the extremity at the time of the radiograph.30 This radiograph should be taken with the extremity in internal rotation because this view best shows head asphericity. Despite adequately taken radiographs, the anteroposterior pelvic view can show only the lateral femoral neck junction and the cross-table lateral view can show only the anterior femoral head-neck junction: it is the anterolateral aspect of the femoral head-neck junction that is often abnormal and not visualized on either view. Specifically in this area, MR arthrography37–39 and the use of specialized radial sequences perpendicular to the true plane of the acetabulum have proved to give invaluable information.
The grade of osteoarthritis is commonly classified according to the criteria described by Tönnis.40 These criteria are of limited value, however, in patients with FAI. The craniomedial joint sector is not well shown in anteroposterior and lateral radiographs, and most patients have completely normal radiographs despite significant symptoms and damage to the acetabular cartilage (as observed surgically and on MR arthrography).32 Even more concerning is the fact that there is a delay in appearance of symptoms; we have operated on patients who have had symptomatic FAI on one side and asymptomatic FAI on the second side, and at the time of surgery there already has been significant cartilage damage on both sides.
MR Arthrography
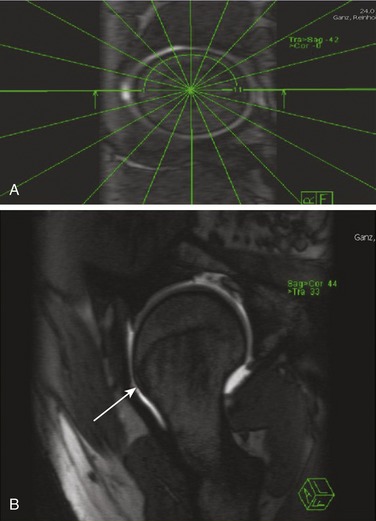
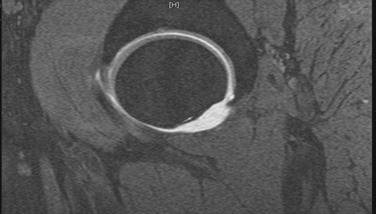
Although conventional and three-dimensional CT scanning of the hip has been described for assessing acetabular version and FAI, MR arthrography of the hip has gained popular acceptance for the diagnosis of these conditions.37–39,41,42 The protocol for obtaining MR arthrography has been described by Locher and colleagues.37 In brief, axial, coronal oblique, sagittal oblique, and radial sequences should be obtained. The radial sequence is a proton density–weighted sequence orthogonal to the femoral head-neck junction and is a reconstruction of the true axial slice orthogonal to the acetabular plane and the sagittal oblique slice parallel to the acetabular plane (Fig. 6-5).
MR arthrography is commonly used to diagnose labral pathology, articular cartilage degeneration, intraosseous ganglion formation, and femoral head-neck junction abnormalities, all of which are important in managing FAI. Labral tears are commonly seen in patients with FAI.39 One study reported the sensitivity and specificity of MR arthrography in diagnosing these tears to be 63% and 71% respectively.41 Adding a small field of view may increase sensitivity to 92%.42 These tears are often seen on T2-weighted images as increased signal intensity that extends into the articular surface.37 It is also common to see extension of the magnetic resonance contrast material into the tear as visualized on T1-weighted images. In contrast to patients with hip dysplasia who commonly have a labral tear within a hypertrophied labrum and associated with intraganglia formation, patients with FAI have labral tears accompanied by very few signal changes within the structure.39
Acetabular cartilage degeneration can also be seen with MR arthrography, but arthrography is less reliable compared with actual intraoperative findings.32 Assessment of the status of the cartilage is important in planning surgical intervention for patients with FAI. The cartilage lesion is often anterosuperior, and patients with advanced cam-type FAI may have extensive chondral lesions in this location as a result of the outside-in shearing mechanism.11,12 Actual debonding of the acetabular cartilage or cleavage lesions are sometimes not visible on MRI, however. The presence and extent of supra-acetabular cyst formation, often not seen on plain radiographs, is also visible on MRI and often is indicative of more advanced disease. It is extremely important to look for migration of the femoral head into the cartilage defect (Fig. 6-6). This is seen as an increase in the width of the contrast layer in the posterior aspect of the joint compared with the anterior aspect. Migration of the head into the defect is indicative of advanced disease.32
Notzli and coworkers15 described the abnormal femoral morphology associated with cam-type FAI. The alpha angle represents the angle formed by a line between the center of the femoral head and the center of the femoral neck, and a line between the center of the femoral head and the point at which the femoral head-neck contour diverges from a circle drawn around the femoral head.15 A mean alpha angle of 74 degrees was seen in patients with clinical symptoms of FAI compared with an alpha angle of 42 degrees in control groups. The relationship between the width of the femoral neck and the diameter of the femoral head (head-neck offset) was also measured on MRI by the same group. The width of the femoral head-neck junction was measured at distances equal to the radius and half the radius of the femoral head along the axis of the femoral neck. The perpendicular distances to the anterior cortex and posterior cortex were recorded and (to correct for patient size) expressed as ratios of the radius length. Increased ratios were also seen in patients with symptomatic FAI.
Current MR arthrography techniques have the ability to see 360 degrees around the femoral head-neck junction with the use of specially obtained radial sequence reconstructions.37 These sequences are highly sensitive in visualizing alterations of head-neck offset and bump formation, which are not commonly seen with conventional radiography and were not seen with axial MRI alone (see Fig. 6-5B). Using these sequences, the surgeon can estimate the amount of bone that will require resection at the time of surgery.
BACKGROUND WORK
Intergluteal Posterolateral Surgical Approach
In 1950, Gibson43 described an approach to the hip that consisted of a posterior skin incision followed by detachment of the anterior border of the gluteus maximus from the iliotibial band. In his description, the deep exposure to the hip was completed by detaching the gluteus medius and minimus from the trochanter. This posterior exposure differs from the traditional Kocher-Langenbeck method44 in that the anterior gluteus maximus fibers are not placed at risk. The gluteus maximus is a powerful extensor of the hip, and all efforts to preserve its function, especially in young patients, should be made.
Nork and colleagues45 described in their anatomic study that the inferior gluteal nerve and artery branches are consistently located within the fascia that is shared by the gluteus maximus and medius. An average of 2.2 major neurovascular branches1–4 travel within this fascia, and if a gluteus-splitting approach is used, the first major branch may cross in a location 7 cm from the greater trochanter (average inferior gluteal nerve and artery 8.7 cm [±1.5 cm]). To protect the vessels and nerves from injury at the time of surgery, the fascia overlying the gluteus medius musculature should be retracted posteriorly with the maximus muscle belly. If a gluteus maximus splitting approach is used, these measurements should be accounted for because vigorous retraction, extended splitting of the gluteus maximus, or coagulation of bleeding vessels within the substance of the muscle may risk damaging the nerve, as these structures run together. Based on our anatomic studies, to maximize surgical exposure and spare the anterior gluteus maximus fibers from damage caused by surgical hip dislocation performed through the traditional Kocher-Langenbeck approach, we have adopted the superficial intermuscular dissection as described by Gibson, which consists of a straight skin incision followed by a trochanteric flip rather than detachment of the gluteal muscles.
Trochanteric Flip Osteotomy (Trigastric Osteotomy)
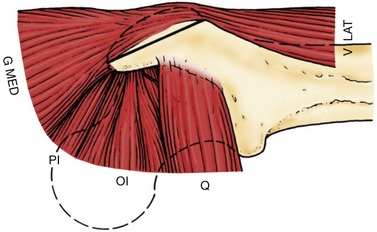
During surgical hip dislocation, in order to provide wide exposure to the hip joint and to minimize injury to the superior gluteal neurovascular bundle, a trochanteric flip osteotomy is preferred.46,47 The trochanter is osteotomized from a posterior-to-anterior direction. Because the deep branch of the medial femoral circumflex artery runs in the trochanteric crest posteriorly,48 the osteotomy should not be performed posterior to the trochanteric overhang, but within the substance of the trochanter approximately 5 mm anterior to it, superficial to the piriformis fossa, and in a direction toward the vastus ridge laterally. In this case, the so-called digastric osteotomy is really a trigastric osteotomy because the gluteus medius and minimus and the vastus lateralis are left on the mobile trochanter. The piriformis, some posterior gluteus medius fibers, and all external rotators are left on the stable portion, reducing the risk of damage to the deep branch as it penetrates the capsule at the posterolateral femoral neck area (Fig. 6-7).
Femoral Head Blood Supply
Knowledge of the arterial anatomy of the hip is crucial for the surgeon performing hip-preserving procedures. The blood supply to the femoral head has been studied by several investigators, and all have contributed significantly to current knowledge.48–54 A summary of the most important points within these classic papers is followed by a summary of the most recent anatomic study performed by the senior author. The nomenclature for the different structures differs among these studies, and this is noted throughout our description.
The primary blood supply to the femoral head is provided by the deep branch of the medial femoral circumflex artery (MFCA). This vessel arises from the profunda femoris, but can arise less commonly from the femoral artery. Howe54 in 1950 described how this vessel (describing the MFCA and not specifically the deep branch of the MFCA), viewed from the posterior direction, lies in the trochanteric fossa proximal to the lesser trochanter, where the posteroinferior vessel (likely the main division of the deep branch) to the femoral head arises. Tucker52 reported that there is often a brief extracapsular anastomosis that occurs in this area, to which the inferior gluteal, profunda femoris, obturator, and circumflex arteries contribute. In our anatomic studies, we found that there are two main central and five main peripheral anastomoses of the MFCA. All of the latter were found to be extracapsular, and the largest and most consistent of these was a branch of the inferior gluteal artery that runs along the inferior border of the piriformis.
Howe and colleagues54 described how the posterior inferior vessel then passes beneath (we believe the author means posterior because otherwise this is not true: the vessel does pass posteriorly to) the obturator externus and penetrates the thin capsule at its insertion into the femoral neck. Protected by a synovial membrane (and not within the external fibrous capsule as described by Tucker52 in 1949), the vessel gives rise to two to three large branches that enter the femoral neck near the junction of the greater trochanter. In this same area, three to four large vessels pierce the lateral capsular insertion, and, passing proximally beneath a thickened synovial membrane (now called the retinaculum), enter toward the superior portion of the femoral head through four to five large foramina located at the articular rim. These vessels give rise to what Trueta and Harrison51 in 1953 called the lateral epiphyseal and superior and inferior metaphyseal arteries (which arise from the superior retinaculum). In their anatomic study, the lateral epiphyseal vessels (usually two to six in number) enter the head superiorly and posterosuperiorly, and closely follow the course of the old epiphyseal plate.
Tucker52 described how these vessels do not really pierce the epiphyseal cartilage, but actually cross the plate at its periphery and then turn toward the center of the femoral head. The superior metaphyseal arteries (usually two to four) arise from the vessels that then give off the lateral epiphyseal group (from the superior retinaculum), enter the superior aspect of the femoral neck at some distance from the articular cartilage, and head vertically down across the neck, and then turn abruptly superomedially toward the epiphyseal scar. Tucker52 found anastomoses between the epiphyseal and metaphyseal vessels within the femoral head; however, the work of Sevitt and Thompson50 and our laser Doppler study measurements do not confirm this finding.
Tucker52 used the term retinacular arteries for the first time and pointed out that there are commonly three groups of them (posterosuperior, posteroinferior, and anterior). The first two are branches of the deep branch of the MFCA. These two groups are moderately large and quite consistent, although the posterosuperior group is usually larger. In his studies, Tucker52 found that occasionally (20% of the time) the posterosuperior group provides the sole supply to the epiphysis. This study provides support to the concept that if damage to the posterosuperior retinacular arteries occurs, and this is the only blood supply to the femoral head, femoral head osteonecrosis may occur. Tucker52
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree