Fat Repositioning in Transconjunctival Lower Eyelid Blepharoplasty
Todd Cook
Raymond S. Douglas
Robert A. Goldberg
Norman Shorr
Lower eyelid blepharoplasty is a useful technique for rehabilitation of the aging face. Many lower eyelid blepharoplasty techniques have been described. Involutional laxity of the orbital septum, orbicularis oculi muscle, and canthal tendons allows protrusion of the anterior orbital fat and interstitial fluid, leading to lower eyelid bags. This convex deformity is accentuated by a coexisting caudal, concave tear trough deformity resulting from age-related loss of fat from the subcutaneous space and attenuation of the superficial musculoaponeurotic system (SMAS) combined with gravitational descent of the suborbicularis oculi fat (1,2). The overall result is a double-convex deformity of the lower eyelid-midface continuum. Repositioning of the prolapsed orbital fat through the transconjunctival approach to fill the tear trough deformity (concavity) is a particularly powerful way of restoring the more youthful single convexity of the lower eyelid-midface continuum (1,3, 4 and 5).
Patient Selection
Ideal patients have moderate fat prolapse and tear trough deformities without coexisting excess skin or interstitial fluid retention. It is important to distinguish interstitial fluid from fat because fluid retention will worsen with surgery and compromise surgical success. When there is a significant history of variable lower eyelid bags, orbital fat is distinguished from interstitial edema by observation of lower eyelid bags in primary gaze and upgaze. Fat becomes more prominent in upgaze and fluid becomes less prominent (Fig. 4.4.1). It may be helpful to photograph this clinical finding with an overhead light source to accentuate subtle differences. When difficulty persists in quantifying the relative contributions of the fat and fluid to lower eyelid bags, the patient should be questioned whether the fluctuation is worse with the intake of salty food, is positional (worse with lying down, improved with head elevation), or worse with exercise. If a question remains, a 1-week course of an oral diuretic is useful. We commonly use hydrochlorothiazide 25 mg per day for 7 days and document the response with photographs.
Technique
Patient preparation begins with marking the patient’s lower eyelid-midface continuum deformities with color-coded markers in the upright position. We also find it useful to hang pictures of the marked and unmarked patient for intraoperative reference. Failure to mark the patient properly will result in loss of the deformities with the injection of local anesthetic and will require a guess on the part of the surgeon as to where to reposition the orbital fat.
Under conscious sedation, the patient is prepared for surgery by placing a drop of tetracaine 0.5% in the inferior conjunctival fornix. Using a 10-mL Luer lock syringe with a 25-gauge 1.5-inch needle, local anesthetic (consisting of a mixture of 9 mL of lidocaine 2% with 1:100,000 units epinephrine and 1 mL of sodium bicarbonate 8.4%) is injected transconjunctivally into the lower eyelid retractors and anterior orbital fat. Patients without significant cardiac history receive a 1:50,000 ratio of lidocaine to epinephrine for improved hemostasis. A transcutaneous infraorbital nerve block then is done, followed by injection into the tear trough deformity. Ten minutes is allowed for the epinephrine to take effect as evidenced by skin blanching. During this time the patient’s skin is prepped with povidone iodine (Betadine) 5%, including a drop in the inferior conjunctival fornix, and draped in sterile fashion.
The assistant positions a lacrimal rake inside the eyelid at the lower border of the tarsus and lifts the lower eyelid away from and superior to the globe. Maintenance of this position will prevent inadvertent premature transection of the orbital septum and potential postoperative lower eyelid retraction. We do not find it necessary to use a corneal protective lens or shield. Beginning centrally, the surgeon grasps the conjunctiva 2.5 mm inferior to the tarsal border with 0.5-mm forceps in the nondominant hand and lifts the conjunctiva away from the underlying lower eyelid retractors. The dominant hand cuts the conjunctiva 1 mm below and parallel
to the inferior tarsal border with the cutting mode of the monopolar needle tip cautery. The incision is carried medially as far as the punctum and laterally as far as the tarsal-tendinous junction.
to the inferior tarsal border with the cutting mode of the monopolar needle tip cautery. The incision is carried medially as far as the punctum and laterally as far as the tarsal-tendinous junction.
The assistant then repositions the rake under the superior edge of the conjunctival incision and the surgeon grasps the inferior edge of the conjunctival incision. The cautery is used to incise the lower eyelid retractors along the entire length of the conjunctival incision. The assistant grasps the inferior cut edge of the lower eyelid retractors and elevates them superiorly, wrapping them around and protecting the globe.
The surgeon uses blunt and sharp dissection in the posterior orbital septal plane to reach the arcus marginalis. We find a combination of pushing with blunt cotton-tipped applicators with intermittent cutting with Westcott scissors to be most useful. We find it possible to maintain a thin layer of posterior orbital septum, preventing premature fat prolapse into the surgical field.
If the orbital fat has not prolapsed into the surgical field, the arcus marginalis is released by elevation off of the inferior orbital rim with a periosteal elevator. A subperiosteal dissection then is performed. If the fat has prolapsed, the posterior remnant of the orbital septum is widely opened and fat pedicles are formed as described later. As the dissection progresses, the lacrimal rake is replaced with an 8-mm Parkes nasal retractor and the area deep to the premarked tear trough deformity is dissected. We often find it necessary to release the origin of the levator labii superioris muscle, which is immediately superior to the infraorbital neurovascular bundle, in order to adequately dissect under the tear trough deformity.
The posterior remnant of the orbital septum is incised with the cutting mode of the monopolar cautery, exposing the orbital fat and allowing it to prolapse into the surgical field. Fat pedicles are formed first by identifying the three distinct lower eyelid fat pads: medial, central, and lateral. Often it is possible to separate the fat pads solely with blunt dissection with cotton-tipped applicators in the dominant hand while elevating the identified fat pad with Adson-Brown forceps; however, the surgeon should not hesitate to use the cutting mode of the monopolar cautery when components of the orbital suspensory ligaments and the arcuate expansion of the inferior oblique tendon are encountered. The number and position of fat pedicles developed are determined by the position and extent of the tear trough deformity. We most commonly form medial and central pedicles but do not hesitate to form a lateral pedicle if necessary. Care is taken when separating the medial fat pad from central fat pad to specifically identify and avoid cutting the inferior oblique muscle. The assistant can aid in pedicle development by wrapping the lower eyelid retractors superiorly around the globe, gently retropulsing the globe. The length of the fat pedicle is determined by the distance necessary to fill the tear trough deformity. We have found that maintenance of a pedicle length to width ratio of 3:1 results in adequate pedicle perfusion and fat survival. The combined width of the pedicles should be wide enough to span the entire width of the tear trough deformity.
The distal ends of the fat pedicles are individually coupled to a double-armed 4-0 chromic suture (G-1 needles). We use a technique similar to that used for securing extraocular muscles in strabismus surgery. A suture is woven through the distal fat pedicle, and locking bites are secured on the medial and lateral most aspects of the pedicle. The subperiosteal space is visualized with elevation using the Parkes retractor, and the needle is directed into the wound to the inferior most aspect of the dissection. The needle is passed upward through the periosteum, through the SMAS, and externalized through the skin. Once both double-armed sutures are properly positioned, the surgeon observes the fat draping over the inferior orbital rim and filling the subperiosteal dissected space while the assistant draws the fat pedicle into the wound by applying slow constant traction on the sutures. The suture is tied without tension and the ends are left long. All of the pedicles are positioned using this technique to completely fill the tear trough deformity.
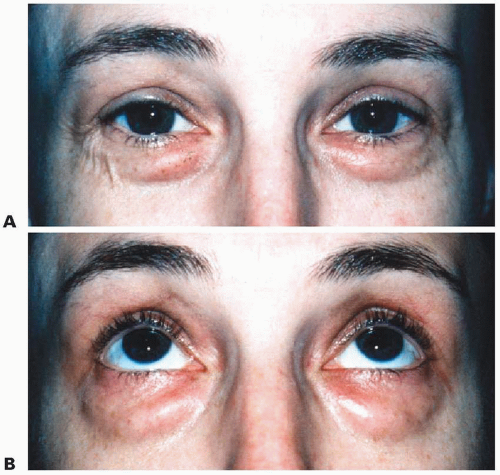
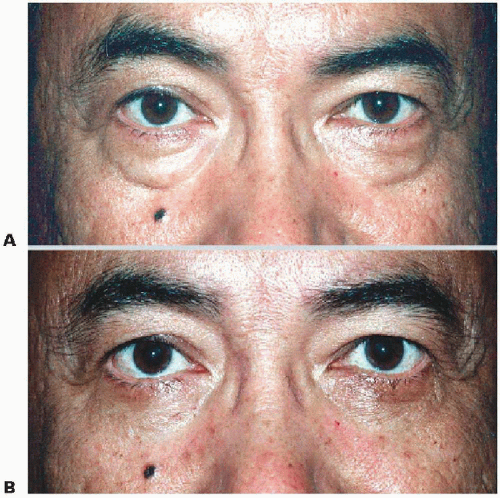 Figure 4.4.2. Before (A) and after (B) transconjunctival lower eyelid blepharoplasty with arcus marginalis release and fat repositioning. |
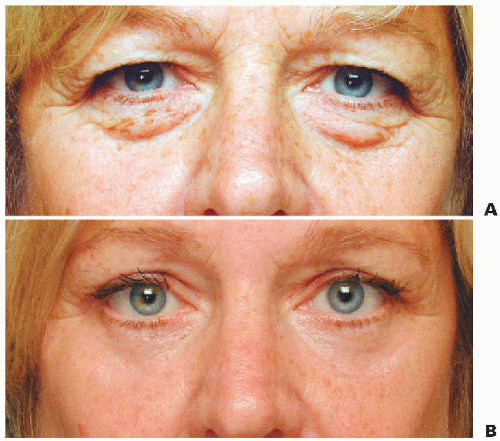 Figure 4.4.3. Before (A) and after (B) transconjunctival lower eyelid blepharoplasty with arcus marginalis release and fat repositioning. |
Gentle forced duction testing is performed to ensure complete freedom of movement of the globe, and the conjunctiva is closed with three interrupted 6-0 fast absorbing gut sutures (PC-1 needle). Antibiotic ointment is placed in the inferior fornix and on the skin sutures, and this application is continued for 10 days postoperatively. The fat pedicle sutures are removed 1 week after surgery.
Excellent results can be obtained using this technique with proper patient identification in men and women (Figs. 4.4.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree