GENERAL 
 What are the bones of the orbit?
What are the bones of the orbit?
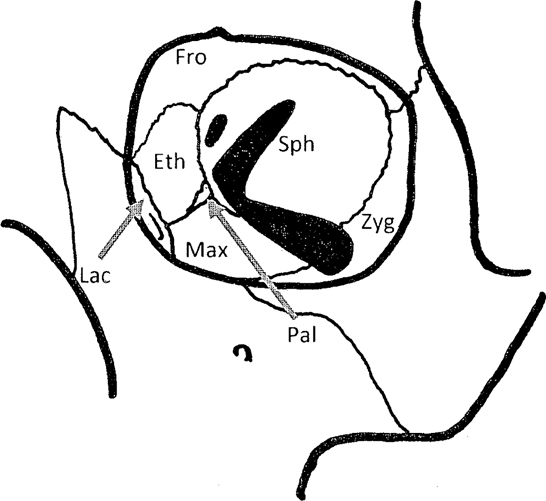
Fro, Frontal bone; Sph, Sphenoid; Zyg, Zygoma; Pal, Palatine bone; Max, Maxilla; Lac, Lacrimal bone; Eth, Ethmoid bone.
Roof: Frontal, lesser wing of sphenoid.
Medial wall: Ethmoid, lacrimal, frontal process of maxilla.
Lateral wall: Zygoma, greater wing of sphenoid.
Floor: Zygoma, maxilla.
 What are the buttresses of the facial skeleton?
What are the buttresses of the facial skeleton?
Vertical: Nasomaxillary (medial), zygomatico-maxillary/lateral orbit (lateral), mandibular ramus (posterior).
Horizontal: Fronto-orbital, inferior orbital rims, maxillary arch, mandibular arch, zygomatic arches.
 What is the most common facial fracture in children?
What is the most common facial fracture in children?
A relatively recent study stratifies by age (0–6, 6–12, 12–18 years) and demonstrated a downward trend over time across age groups in skull and orbital fractures, and a concomitant upward trend in midface (maxillary, nasal, NOE, ZMC) fractures, mandible, and dentoalveolar fractures, as a percentage of total fractures remained stable from infancy through adolescence; in this study, orbital fractures were most common, followed by mandible or nasal, depending on the age.
 What is the current consensus of use of resorbable plates in facial fractures?
What is the current consensus of use of resorbable plates in facial fractures?
Some studies show comparable results to titanium, but their use is not commonly employed, and remains controversial.
 What is the standard imaging for facial fractures?
What is the standard imaging for facial fractures?
CT scan with axial and (reconstructed) coronal images are the minimum necessary; often sagittal and/or 3D reconstruction are critical to fully define the extent of injury.
 When is consideration made for tracheostomy in facial fractures?
When is consideration made for tracheostomy in facial fractures?
Unstable airway (bilateral mandible fractures and altered LOC); panfacial fractures with maxillary and mandibular fractures, especially with concomitant thoracic trauma and pulmonary contusion or brain injury.
 Is IMF an indication for gastrostomy?
Is IMF an indication for gastrostomy?
No. A liquid diet can be managed effectively per os (through a straw) in most cases.
 What finding should raise concerns with skull base fractures?
What finding should raise concerns with skull base fractures?
Pulsatile proptosis, headache, visual loss, diplopia and periorbital and ocular erythema are signs of posttraumatic carotid-cavernous fistula. It may occur with fractures extending into the cranial fossa from either posterior or anterior cranial fossae. It is confirmed with angiography, and initially managed with VIR techniques.
 In facial nerve transection, how long before the distal segments lose the ability to be located with a nerve stimulator?
In facial nerve transection, how long before the distal segments lose the ability to be located with a nerve stimulator?
24 to 48 hours.
 What general anatomic landmark may be used to determine the feasibility of facial nerve exploration and repair?
What general anatomic landmark may be used to determine the feasibility of facial nerve exploration and repair?
Injuries medial to the lateral canthus are unlikely to be successfully repaired surgically.
 How often do patients with facial fractures from high-speed motor vehicle crashes sustain cervical spine injury?
How often do patients with facial fractures from high-speed motor vehicle crashes sustain cervical spine injury?
10%.
 How are parotid duct injuries managed acutely?
How are parotid duct injuries managed acutely?
Cannulation with a 5F pediatric feeding tube, with instillation of dye to locate laceration or transaction. Repair with fine suture (8-0 monofilament) acutely over the stent is advised.
 How effective is external carotid artery ligation in controlling facial hemorrhage following traumatic injury?
How effective is external carotid artery ligation in controlling facial hemorrhage following traumatic injury?
Because of rich collateralization between internal and external carotid artery vascular territories, ligation is usually not very effective. Packing oral and nasal cavities is more likely to stem the hemorrhage and allow for coagulation and hemostasis.
 What is a “growing” skull fracture?
What is a “growing” skull fracture?
Usually encountered in children under age 3 years, it occurs when a skull fracture is accompanied by an underlying dural tear that is untreated. Herniation of the underlying brain, sometimes referred to as a leptomeningeal cyst, prevents spontaneous bone healing, and the fracture appears to widen over time. It is managed with dural repair and cranioplasty.
 How does one approach the panfacial fracture?
How does one approach the panfacial fracture?
From stable to unstable; with concomitant maxillary and mandibular fractures, usually occlusion is established, followed by mandible, then maxilla ORIF.
 In cases of ORIF of the maxilla and/or mandible, what are the most likely causes of malocclusion after removal of intraoperative IMF?
In cases of ORIF of the maxilla and/or mandible, what are the most likely causes of malocclusion after removal of intraoperative IMF?
Inadequate reduction leading to inaccurate placement of miniplate fixation.
 FRONTAL SINUS
FRONTAL SINUS 
 How often do frontal sinus fractures present with CSF leak?
How often do frontal sinus fractures present with CSF leak?
About 20%
 What is the cause of a CSF leak in this setting?
What is the cause of a CSF leak in this setting?
A dural tear (likely from a posterior table bone fragment or cribriform plate disruption) combined with a fracture pattern allowing the CSF to enter the paranasal sinuses.
 What are the conditions in frontal sinus fracture that warrant conservative management?
What are the conditions in frontal sinus fracture that warrant conservative management?
Minimal displacement of fractures (anterior and posterior tables), even when CSF leak is present, are initially managed with observation. If CSF leak persists, a lumbar drain may be considered to reduce the flow across the dural tear, and allow for secondary healing.
 What are the features in frontal sinus fracture that determine which operative intervention is indicated?
What are the features in frontal sinus fracture that determine which operative intervention is indicated?
There are three: integrity of the barrier between the brain and frontal sinus, contour of the anterior table, and patency of nasofrontal ducts. The (colonized) sinus mucosa must be removed if there is communication with the dura/brain; therefore, cranialization is usually employed when there is a displaced posterior table fracture with or without CSF leak. ORIF of the anterior table addresses contour deformity, and outlet obstruction (assessed with instillation of dye in sinus, with patency confirmed with appearance of dye in nasal cavity) with intact posterior table is addressed by sinus obliteration or endoscopic sinus surgery.
 How is the frontal sinus cranialized?
How is the frontal sinus cranialized?
A coronal approach is generally employed, in the subpericranial plane. The fragments of the anterior table are marked for replacement, and additional osteotomy performed if necessary. The posterior table, usually comminuted, is removed, the dura repaired, the mucosa of the sinus thoroughly stripped, the sinus bony surface burred, and a pericranial flap raised from the frontal scalp, and placed in the base of the sinus to form a barrier between the intracranial space and frontonasal ducts. The anterior table is replaced with internal fixation, leaving a small gap above the brow to accommodate the pericranial flap.
 How is the frontal sinus obliterated?
How is the frontal sinus obliterated?
The anterior table fragments are recovered, the mucosa stripped and the bony cavity burred, the pericranial flap raised and inset, and the sinus cavity filled with fat, muscle, or bone. The anterior table is replaced with internal fixation.
 How is the mucosa properly stripped?
How is the mucosa properly stripped?
All visible mucosa is manually removed. A fine burr is used over the entire bony surface of the sinus to remove the remaining mucosal invaginations (pits of Breschet).
 How do you test for CSF?
How do you test for CSF?
Beta-2-transferrin is most specific; halo sign on filter paper is unreliable.
 What are the early complications of frontal sinus fracture?
What are the early complications of frontal sinus fracture?
CSF leak, epistaxis, meningitis, intracranial bleed.
 What are the late complications of frontal sinus fracture?
What are the late complications of frontal sinus fracture?
Osteomyelitis, mucocoele (from retained mucosa), intracranial abscess. These can occur years later; current recommendations are for annual surveillance imaging for 5 years, though there are many cases of mucocoele presenting more than 10 years post-injury.
 NASAL
NASAL 
 What is the sensory innervation of the nose?
What is the sensory innervation of the nose?
External branches of the anterior ethmoidal nerve (V1), infratrochlear nerve (V1) supply superior portion and tip; branches of infraorbital nerve (V2) supply inferior and lateral nasal skin.
 Why must a septal hematoma be drained?
Why must a septal hematoma be drained?
Failure to recognize and treat a septal hematoma may result in necrosis of the septal cartilage and perforation. It is most effectively accomplished with early intervention (at presentation) and apposition of mucosa to cartilage must be confirmed.
 What are the common features of a naso-orbital-ethmoid fracture?
What are the common features of a naso-orbital-ethmoid fracture?
Telecanthus, epiphora, flattened nasal bridge, upturned nasal tip.
 What is the Markowitz–Manson classification schema for NOE fractures?
What is the Markowitz–Manson classification schema for NOE fractures?
Related to the fragment with the medial canthal insertion:
Type 1: large central fragment
Type 2: small fragment within comminuted segment
Type 3: extensive comminution/avulsion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


