33 Facial prosthetics in plastic surgery
Synopsis
 The success of osseointegration biotechnology has revolutionized facial prosthetic reconstruction.
The success of osseointegration biotechnology has revolutionized facial prosthetic reconstruction.
 Titanium is the implant material of choice as it is light, biocompatible, and resistant to corrosion.
Titanium is the implant material of choice as it is light, biocompatible, and resistant to corrosion.
 Implant placement technique is crucial to produce bone–implant contact with no interposed fibrous tissue and successful bone healing.
Implant placement technique is crucial to produce bone–implant contact with no interposed fibrous tissue and successful bone healing.
 Appropriate treatment selection requires understanding of all options available.
Appropriate treatment selection requires understanding of all options available.
 Multidisciplinary team planning is required.
Multidisciplinary team planning is required.
 Osseointegration biotechnology provides plastic surgeons with more treatment options for challenging head and neck deformities.
Osseointegration biotechnology provides plastic surgeons with more treatment options for challenging head and neck deformities.
Historically facial prosthetics have been of limited benefit. Retention of facial prostheses has been largely unsuccessful because of the need for adhesives or crude mechanical means of maintaining retention. The patient lacked confidence about the positioning of the prosthesis and its ability to stay in place. Often associated pain or discomfort would limit the length of time and circumstances in which the prosthesis would actually be worn. The adhesives are those used in industry and were not developed for the unique sensitive human biological environment. They often had adverse effects on the underlying skin compromised by radiotherapy, trauma, or thermal injury1 and affected the durability and longevity of the prosthesis.
With the success of osseointegration and its ability to solve the problem of prosthetic retention,2,3 a new treatment modality was now available.4,5 Prosthetic longevity is increased without the need for adhesives.6,7 Osseointegrated retained facial prosthetics now meet the necessary criteria for success: (1) aesthetic acceptability; (2) functional performance; (3) biocompatibility; and (4) desired retention.8 The use of osseointegration biotechnology in facial prosthetic restoration has been hailed as the most significant advance in the field of facial prosthetics in the past 25 years.9 It is estimated that more than 90 000 implants have been installed extraorally in more than 45 000 patients up to the year 2007.10
Craniofacial osseointegrated reconstruction gives the plastic surgeon another viable treatment option in many challenging head and neck defects.11 It can provide some patients with a meaningful and enhanced quality of life when in the past other treatment options would not have been successful. Unfortunately, competing specialties or providers have presented autologous techniques and craniofacial osseointegration as unrelated technologies.12 Osseointegrated and autogenous techniques should not be viewed as competing technologies, but rather as complementary reconstructive procedures that optimize the opportunity for success in the management of major head and neck deformities.
Historical perspective
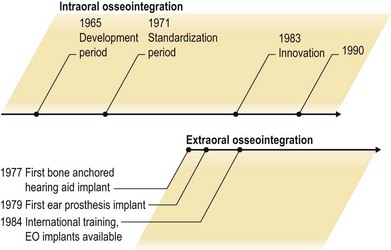
Historically, implants in bone were largely unsuccessful and had a poor reputation for long-term success. In the 1950s, Professor Brånemark, from Goteborg, Sweden, discovered titanium behaved somewhat differently from other metals when in contact with bone. The first osseointegrated implant was placed in a human in 1965. The term “osseointegration” was coined by Brånemark in 1977.13 It is defined as the direct contact – structural and functional – between ordered living bone and the surface of a load-bearing implant. Osseointegration is a dynamic process that involves micromodeling at periosteal and endosteal surfaces and remodeling at the bone–implant interface.8,10,14 This principle of osseointegration ultimately led to the development of successful dental implants.15 Albrektsson et al. further postulated that a skin-penetrating implant may be possible.16 Implants were first placed in the mastoid region to support a bone-anchored hearing aid in 1977 and to retain an auricular prosthesis in 197917 (Fig. 33.1). Subsequently, numerous reports have confirme the efficacy and predictability of craniofacial osseointegration.18,19 The concept of anchoring craniofacial prosthesis on osseointegrated implants was accepted by the Food and Drug Administration (FDA) in 1985. The FDA accepted the concept of anchoring hearing aids on implants in adults in 1995 and children in 1998. In 1985, implants were used in hand surgery to anchor joint replacements and in the early 1990s the concept was used for anchoring prostheses in amputees’ fingers, hands, arms, and legs.
Advantages of craniofacial osseointegration
Craniofacial osseointegration has many advantages (Box 33.1).20 The surgical procedures are generally short with minimal morbidity and are performed on an outpatient basis. There is a short learning curve and results are predictable. The patients usually have minimal postoperative discomfort. Examination of the tumor resection site is easy and allows early diagnosis of any tumor recurrence.
Box 33.1
Advantages of craniofacial osseointegration7
Allows examination of tumor resection site
Salvage of autogenous failures
The disadvantages of craniofacial osseointegration include the need for a larger multidisciplinary team with skills that are often not freely available. Patients also require regular maintenance visits and a new prosthesis every 2–5 years (Box 33.2).20 Lifetime ongoing costs can be an issue with some insurance companies.
Indications for craniofacial osseointegration
Craniofacial osseointegration can be of particular benefit for reconstruction of selected defects involving the ear, orbit, nose, and combined midfacial defects. The osseointegrated implants have also been used to secure hairpieces.21 A newer application of interest to the plastic surgeon is the use of a bone-anchored hearing aid (BAHA) in children with microtia. In the past concern has been expressed combining a BAHA and an autogenous ear reconstruction. Fear of inappropriate positioning of the implant adversely affecting future autogenous ear reconstruction usually prevented patients having the benefits of both treatment modalities. This usually resulted in the BAHA being placed too far posterior or not being considered at all. Certainly the BAHA is an excellent option for hearing restoration in bilateral microtia patients and more recently has proven of benefit in unilateral microtia patients (Fig. 33.2). It is a much more straightforward, safer, and predictable way of improving hearing than previous autogenous means of canalplasty and middle-ear reconstruction.10
Ear reconstruction
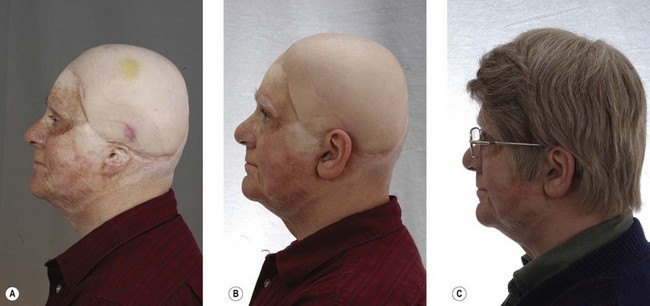
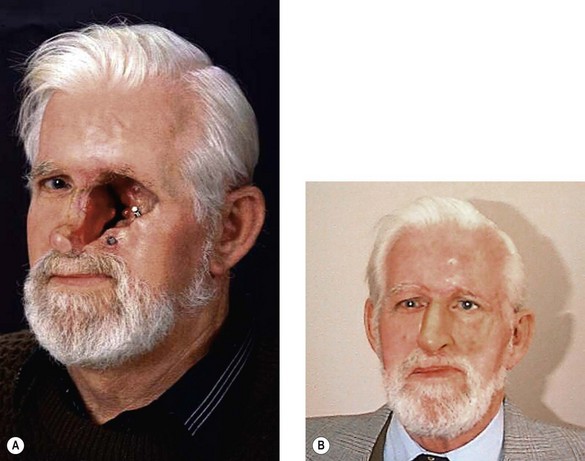
Autogenous reconstruction of auricular defects has improved greatly in the latter half of the 20th century because of the work of pioneers such as Tanzer,22 Brent,23–26 Fukada and Yamada,27 Cronin,28 Bauer,29 Yanai et al.,30 Isshiki et al.,31 Nagata,32–34 and others. Certainly, not all reconstructive attempts are successful. The appropriate treatment selection for major ear defects continues to be controversial (Table 33.1).20 Certain auricular defects have limited autogenous options, particularly after removal of the ear for cancer with associated radiotherapy. It is our belief that these reconstructive techniques are complementary and must be presented in this manner.8,12,20 Definite indications for osseointegrated auricular prosthetic reconstruction include: (1) following major cancer resection; (2) radiotherapy to the proposed site of auricular reconstruction; (3) severely compromised local tissue (Fig. 33.3); (4) patient preference; and (5) salvage procedure for failed autogenous reconstruction. Relative indications include: (1) microtia; (2) absence of the lower half of the ear; and (3) patients with calcified costal cartilage.
Table 33.1 Indications for osseointegrated ear reconstruction7
| Definitive | Relative |
|---|---|
| Major cancer resection | Microtia – most controversial |
| Radiotherapy | Absence of lower half of the ear |
| Severely compromised tissue | Calcified costal cartilage |
| Patient preference | |
| Failed autogenous reconstruction | |
| Potential craniofacial anomaly | |
| Poor operative risk |
Probably the most controversial indication for osseointegrated auricular reconstruction is microtia in children. Although it is technically possible to place implants in children as young as 3 years and early results are encouraging, the follow-up in these situations is short. Because the use of craniofacial osseointegrated implants requires removal of any local ear remnants and produces scarring in the operative field, future autogenous reconstruction options are very limited. For these reasons, the use of osseointegrated auricular reconstruction in the pediatric age group requires very careful consideration by the clinician and family (Fig. 33.4). A publication by Zeitoun et al.35 outlines the difficulties seen using osseointegration in the pediatric population. It also showed an increased need for psychological support in many of these patients. Our approach is to offer autogenous ear reconstruction to pediatric patients with microtia. Despite the potential for difficult treatment selection decisions, we rarely find this to be the case. Patients usually decide quite quickly after the possibilities are discussed. It is rare for patients to change their mind following further discussion.
Osseointegrated nasal reconstruction
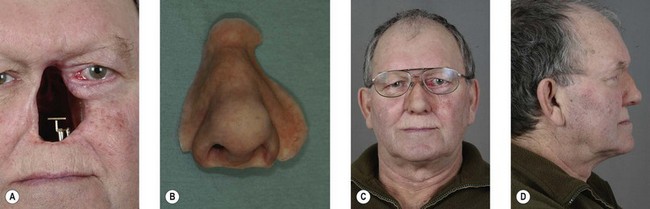
Indications for osseointegrated nasal reconstruction include: (1) failed autogenous reconstruction; (2) significant scarring in potential autogenous donor sites (Fig. 33.5)6; (3) tumor recurrence following initial autologous reconstruction; and (4) patient preference (Box 33.3). Because of the need for multiple surgical stages and the greater variability in the ultimate result with autogenous reconstruction, many patients with total nasal loss opt for placement of implants and a nasal prosthesis (Fig. 33.6). Certainly, there is less surgery involved with less morbidity. There is no need for other donor sites, and tumor surveillance is easy with prosthesis removal.8 The application of “nontraditional” long zygomaticus implants may be useful in difficult situations of nasal reconstruction.36
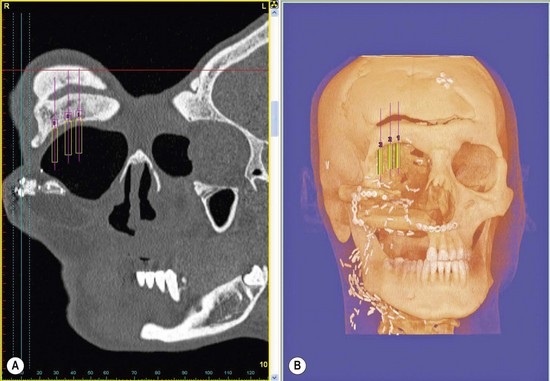
Fig. 33.5 (A, B) A Simplant™ study can be performed to determine quantity and quality of underlying bone.
Box 33.3
Indications for osseointegrated nasal reconstruction10
Failed autogenous reconstruction
Scarring at autogenous donor sites
Reconstruction following autogenous reconstruction because of tumor recurrence
Medical contraindication to multistaged autogenous reconstruction
Osseointegrated orbital reconstruction
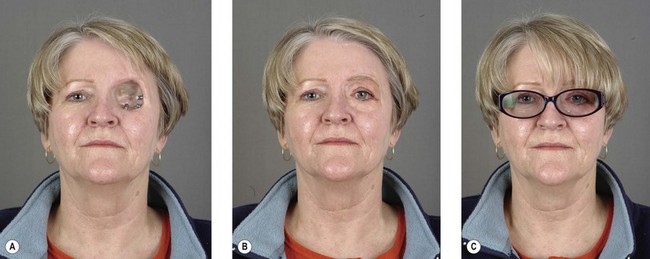
Patients with loss of the orbit and orbital contents have very poor autogenous reconstructive options (Box 33.4). Although autogenous coverage may be necessary to cover important neurological structures, in many cases it is provided only to fill the residual orbital cavity. However, “filling the hole” does not create an aesthetic result. It is in these situations that osseointegrated orbital reconstruction clearly has advantages over autogenous reconstruction. The aesthetic results are far superior and again allow visualization for early tumor recurrence (Fig. 33.7). This approach could also be considered in patients with severe enophthalmos and significantly compromised vision. Less frequently, it can be considered in patients with an ocular prosthesis and significant eyelid distortion secondary to trauma or radiotherapy that is not amenable to autogenous correction. The hope for the future would be to create an orbital prosthesis that can mimic movement of both the lids and globe of the opposite normal eye.13
Box 33.4
Indications for osseointegrated orbital reconstruction
Loss of orbit and orbital contents
Severe enophthalmos with compromised vision
Midfacial reconstruction
Patients with complex facial defects that may include the orbit, nose, and maxilla again have poor autogenous options (Fig. 33.8). Craniofacial osseointegration offers significant advantages. It enables examination of the posttumor defect and allows for a very acceptable aesthetic result. In the patient shown in Figure 33.8 it allowed early detection of a recurrence on the posterior orbital wall. Treatment consisted of surgical removal and reconstruction with a temporoparietal fascial flap and skin graft. The patient was able to resume wearing his prosthesis again only 12 days after surgery to resect the recurrence. Extraoral osseointegration in combination with intraoral osseointegration may also result in significantly improved functional results over conventional prosthetic or autogenous techniques.
Factors important to obtain osseointegration13,37
Choice of implant material
Many materials have been considered for osseointegration. Although other metals such as vanadium, tantalum, aluminum hydroxide, and ceramics like hydroxyapatite are known to integrate with bone to a certain degree, titanium is currently the material of choice.37 Titanium is relatively light but stiffer than bone. Its springiness allows it to flex with the bone. The most important factor is the ability of its titanium oxide layer on the implant surface to react with the adjacent bone (its biocompatibility). The key to success is what happens at this implant–tissue interface. The most successful is commercially pure titanium, which is 99.75% pure. This differs from the most commonly used titanium alloy, which contains 90% titanium, 6% aluminum, and 4% vanadium, and exhibits much less satisfactory characteristics of osseointegration.