CHAPTER 7 Facelift with SMAS technique and FAME
History
Surgery of the deep layer tissues of the face and neck is now established as a permanent part of facelift operations. There is no clear consensus as to how to treat the midface and its related nasolabial fold. Skoog introduced tightening of the midface superficial fascia and platysma muscle in the late 1960s, and Mitz and Peyronie verified the anatomy of the superficial musculoaponeurotic system (SMAS) in 1976. Surgery of the midface developed subsequent to descriptions of the retaining ligaments of the cheek, as the focus of facial rejuvenation extended to correction of the nasolabial fold. Masseteric-cutaneous and lateral zygomatic-cutaneous ligament release allowed lifting of the SMAS to correct the lower face below the zygoma. However, approaches to the prezygomatic SMAS developed in an effort to gain harmony of the upper and lower parts of the face. In this effort two different approaches are in use:
1. Wide skin undermining and separate dissection of a SMAS platysma flap.
2. Very limited skin undermining in the cheek and the dissection beneath the SMAS layer in continuity with the skin.
Physical evaluation
• Evaluate the face in general for the bone structure of the entire face including the forehead, orbits, zygomas, zygomatic arches, maxilla, mandible, mentum, as well as the lips, nose and teeth.
• Evaluate skin quality and laxity, fat deposits and/or bulges in the face and neck.
• Evaluate midface thickness, laxity, and mobility to finger tip manipulation.
• Evaluate nasolabial folds, and labiomandibular folds if present.
• Evaluate neck including fat deposits, platysma muscle anatomy, hyoid position, thyroid cartilage contour and submandibular gland position.
• Evaluate the malar area for bony contour and the thickness of the soft tissue lying medial to the zygomaticus major muscle.
• Evaluate the lower eyelids for the integrity and function of the orbicularis oculi muscle.
• Evaluate the lower eyelids for prominence of herniated fat, prominence of the bony orbital rim, palpebromalar grove and nasojugal grove.
• Determine patient’s main concerns.
Anatomy
The midcheek can be understood as part of the midface and refers to a part of the cheek medial to a line extending from the frontal process of the zygoma to the oral commissure and from the lower lid above to the nasolabial fold below. It is composed of two functionally distinct parts including the prezygomatic part over the body of the zygoma and maxilla and infrazygomatic part below, as described by Mendelson (Ch. 6). A major determinant of the shape of the midface is the underlying skeleton as it connects the orbital and oral cavities and provides a bony platform for their skeletal attachments and retaining ligaments of each muscle. The aging changes that appear in the midcheek largely reflect the effect of laxity and ptosis of the soft tissues relative to the underlying skeleton. This affects the upper face by revealing the anatomy of the orbit, with exposure of the bony orbital rim inferiorly, palpebromalar groove laterally, and nasojugal groove medially. The displaced soft tissue accentuates the nasolabial fold and reveals lower lid fat bulges. With soft tissue descent, laxity of the structures of the prezygomatic space including the orbital retaining ligament at its uppermost aspect and its roof (pars orbitale of the orbicularis oculi) are resisted by the zygomatic-cutaneous ligaments below. When visibly enlarged this area forms the clinical entity known as the malar mounds, also termed malar bags and malar crescent. It should be noted that the presence of the malar septum was described by Pessa and Garza and Pessa et al. to explain the clinical appearance of a black eye, and explain the anatomic basis of malar mounds and malar edema. Malar mounds should be distinguished from the malar fat pad. The anatomical terminology regarding this area can be somewhat confusing, as the malar fat pad is also simply known as malar fat.
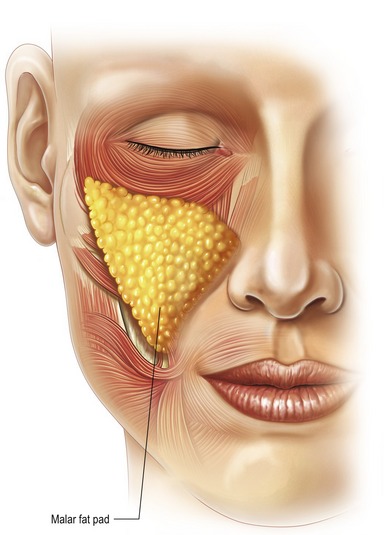
Specifically, the malar fat pad is a term used to describe the subcutaneous fat of the medial cheek that exaggerates the nasolabial fold. The malar fat pad is a localized thickness of the subcutaneous panniculus adiposus (Fig. 7.1). The malar fat pad is of maximum thickness centrally in youth with a well-defined border at the nasolabial crease and less discrete border in the upper face as it blends imperceptibly into the lower lid with a gradual decrease in thickness over the prominence of the orbital rim and zygoma. The malar fat has upper, middle and lower components. The fullness of the nasolabial fold is in large part caused by the medial and inferior migration of the soft tissue medial to the zygomaticus major muscle (primarily the malar fat pad). It is triangular in shape with its base along the nasolabial crease, and its apex overlies the body of the zygoma. The malar fat pad firmly attaches to skin. It is easily separated from underlying fascia, and the malar fat pad moves forward and down perpendicular to the nasolabial crease during the aging process.
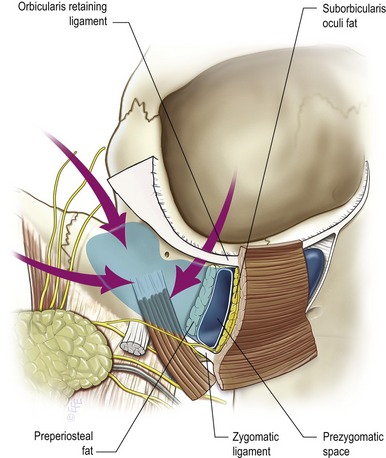
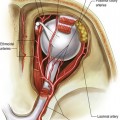
The prezygomatic space overlies the body of the zygoma and the origins of the lip elevator muscles. It extends to the posterior border of the body of the zygoma and can be accessed from the lower temporal region and lower lid. The floor is a thick layer of preperiosteal fat with an overlying thin membrane which covers the origins of the muscle bellies of the lip elevators. The upper border of the space is formed by the orbicularis retaining ligament, which separates the preseptal from the prezygomatic space and becomes confluent at the inferolateral orbital rim with the broad lateral orbital thickening that overlies the frontal process of the zygoma. The zygomatic-cutaneous neurovascular pedicle is the only structure crossing this space as Mendelson has previously elucidated. The roof of the space is the orbicularis oculi and its investing fascia, which is contiguous with the temporoparietal fascia laterally. The inferior wall of the prezygomatic space is lined by a continuation of the preperiosteal membrane and the most cephalad of the zygomatic-cutaneous ligaments as they extend between the origins of the lip elevator muscles through the subcutaneous fat to the dermis. With blunt dissection in this space, as in the FAME procedure, the smooth surface of this membrane remains intact and preperiosteal fat remains attached to the underlying facial bones. Mendelson has noted that the prezygomatic space can be entered from (1) the lower eyelid; (2) the temporal area; (3) laterally passing between the seventh nerve branches as performed with the FAME procedure to enter the prezygomatic space (Fig. 7.2).
Technical steps
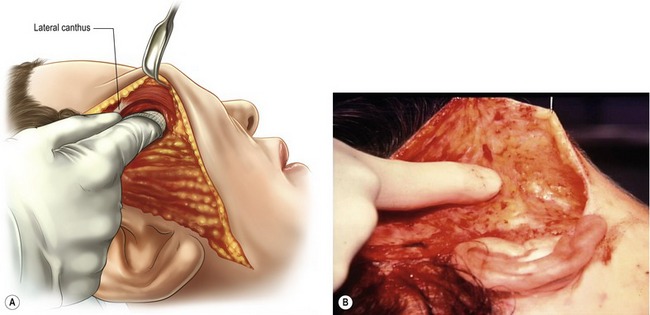
The senior author (SJA) began using the FAME technique in the early 1990s as a procedure in conjunction with a standard SMAS/platysma facelift to improve the midface and nasolabial fold. The FAME technique (finger assisted malar elevation) is a composite technique designed to elevate skin, lateral orbicularis oculi muscle, and reposition the malar fat pad. This technique is used in combination with skin undermining and a SMAS/platysma flap to correct the remainder of the laxity in facial and cervical areas. The description given here is as performed for approximately 14 years. Recent modifications since February 2006 will be described below.
In the temporal area the skin is undermined sharply for approximately half the distance between the ear and lateral canthus. The right index finger is rotated medially and inferiorly so as to separate the orbicularis oculi muscle from the temporal fascia; the lateral canthus is easily reached (Fig. 7.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree