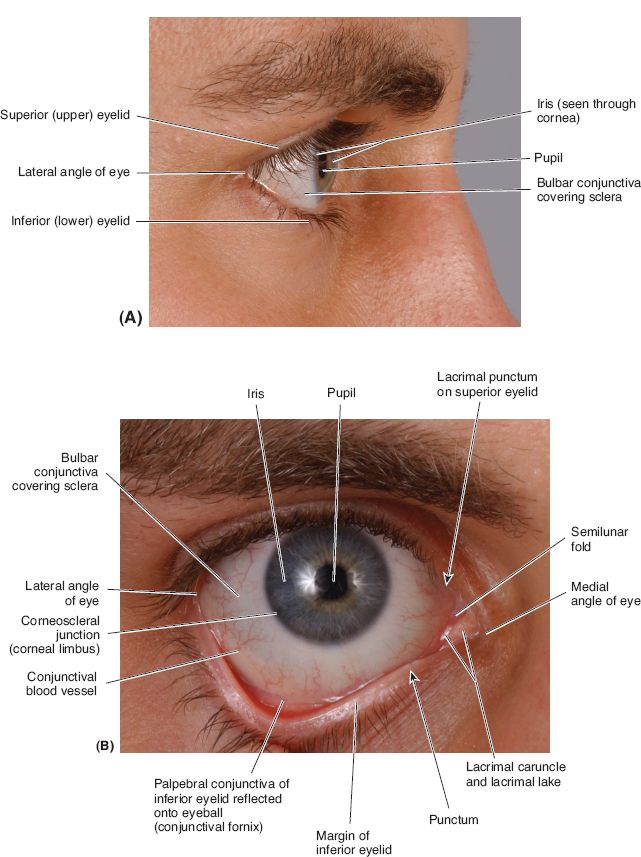
I. EYELID ANATOMY AND PHYSIOLOGY (FIG. 19-1)
A. The primary function of the eyelids is protection of the globe.
B. The upper eyelid is dynamic, whereas the lower eyelid acts as a static sling.
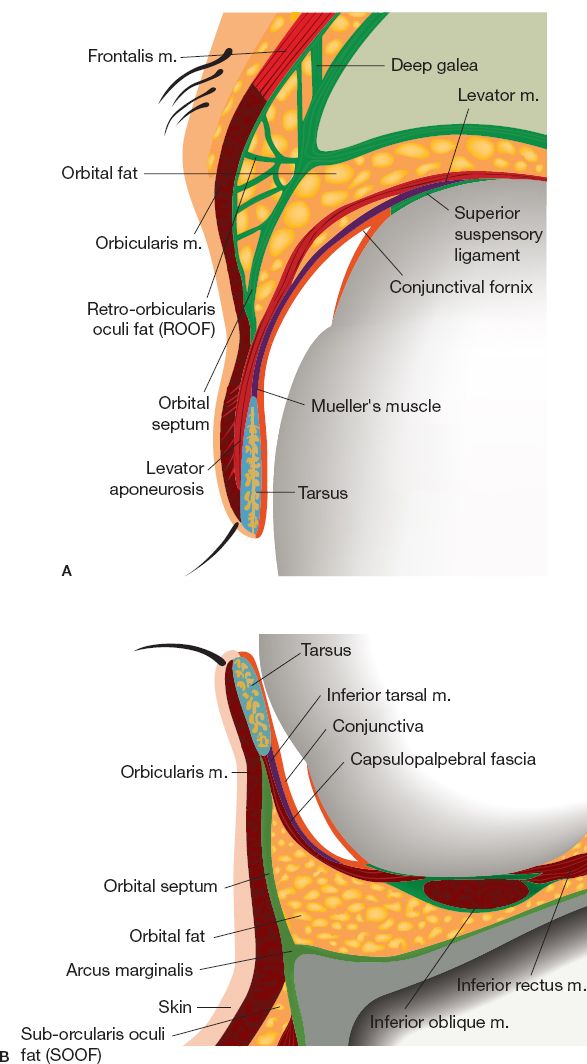
C. Composed of three lamellae (Fig. 19-2): Well-vascularized external coverage (anterior), structural support (middle), and mucosal lining (posterior).
1. Anterior lamella: Skin and orbicularis oculi muscle
a. Skin
i. Approximately 1-mm-thick—thinnest skin in the body
ii. Underlying subcutaneous tissue is exiguous and areolar
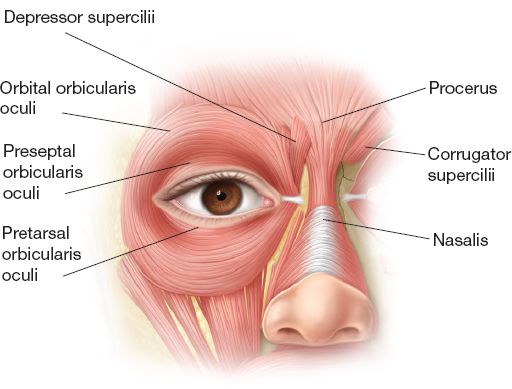
b. Orbicularis oculi muscle (Fig. 19-3)
i. Innervated by zygomatic branch (CN VII) on its undersurface
ii. Pretarsal portion: Assists with involuntary blink
iii. Preseptal portion: Assists with involuntary blink
iv. Orbital portion: Produces voluntary lid closure
2. Middle lamella: Preseptal fat, orbital septum, and orbital (postseptal) fat
a. Preseptal fat
i. Between the orbicularis oculi muscle and the orbital septum
ii. Upper eyelid: Retro-orbicularis oculi fat (ROOF)
iii. Lower eyelid: Suborbicularis oculi fat (SOOF)
iv. Increasingly ptotic with age causing fullness and hooding
b. Orbital septum: Anatomic boundary between eyelid and orbit
i. Multilayer fibrous membrane arising from the periosteal confluence of the superior and inferior orbital rims.
ii. Fuses with the levator aponeurosis in the upper eyelid and the capsulopalpebral fascia in the lower eyelid.
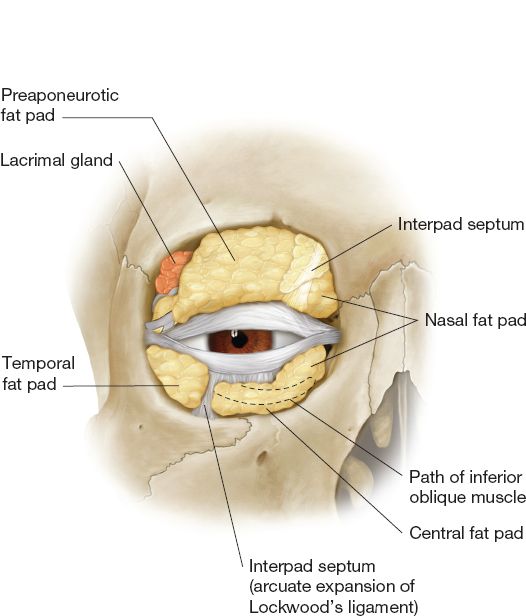
c. Orbital (postseptal) fat (Fig. 19-4)
i. Upper eyelid: Two compartments (nasal and central)—separated by the trochlea and superior oblique tendon.
ii. *Lower eyelid: Three compartments (medial, central, and lateral)—inferior oblique muscle separates medial and central compartments.
iii. Medial compartment contains white fat with small lobules.
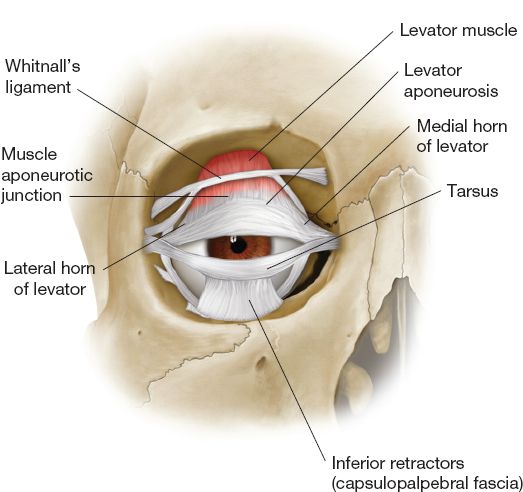
3. Posterior lamella (Fig. 19-5): Tarsal plate, retractor muscles, and conjunctiva
a. Tarsal plates
i. Composed of cartilaginous-like dense connective tissue
ii. Provides structural support and rigidity to the eyelids
iii. Superior tarsus: 1-mm-thick, 25 mm long, 10 mm tall
iv. Inferior tarsus: 1-mm-thick, 25 mm long, 4 mm tall
b. Upper lid retractors
i. *Levator palpebrae superioris:
a) Innervation: Superior division of CN III
b) Origin: Lesser wing of sphenoid, then broadens as aponeurosis at Whitnall’s ligament
c) Insertion: Superior tarsus and dermis forming supratarsal crease
d) Function: Acts as fulcrum providing 10 to 15 mm lid elevation
______________
*Denotes common in-service examination topics
Figure 19-1. Surface anatomy of the eye. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
ii. *Mueller’s muscle
a) Innervation: Sympathetic nervous system
b) Origin: Deep surface of levator aponeurosis
c) Insertion: Superior tarsal margin
d) Function: 1 to 2 mm lid elevation
c. Lower lid retractors
i. Capsulopalpebral fascia: Analogous to levator aponeurosis
a) Origin: Inferior rectus sheath, splits at inferior oblique muscle, then reunites as Lockwood suspensory ligament (lower lid equivalent of Whitnall’s ligament)
b) Insertion: inferior tarsus
Figure 19-2. Cross section of the upper (A) and lower eyelids (B). (Redrawn from Tasman W, Jaeger EA, eds. Duane’s Opthamology on CD-ROM. 2006 ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2006.)
Figure 19-3. Periorbital musculature.
Figure 19-4. Eyelid fat compartments and lacrimal gland.
Figure 19-5. Ligamentous and cartilage support structures of the eyelids.
ii. Inferior tarsal muscle: Analogous to Mueller’s muscle
a) Innervation: Sympathetic nervous system
b) Origin: Posterior capsulopalpebral fascia
c) Insertion: Inferior tarsal margin
d. Conjunctiva
i. Gliding surface of nonkeratinized squamous epithelium
ii. Palpebral conjunctiva: Posterior surface of the eyelid
iii. Bulbar conjunctiva: Anterior surface of the globe
iv. Superior and inferior fornices: Apices where the palpebral and bulbar conjunctiva meet
D. Lateral canthal tendon (LCT)
1. Originates at lateral margin of the superior and inferior tarsal plates
2. Crura fuse as a Y-shaped common tendon that inserts onto Whitnall’s tubercle, a bony prominence located 5 mm within the lateral orbital rim
a. Eisler fat pad is anatomic landmark for Whitnall’s tubercle
b. Located in pocket between the orbital septum and LCT insertion
3. Other contributing structures: Pretarsal and preseptal portions of the orbicularis oculi muscle, lateral horn of the levator aponeurosis, Lockwood suspensory ligament, and check ligament of the lateral rectus muscle
E. Medial canthal tendon (MCT)
1. Originates at medial margin of the superior and inferior tarsal plates.
2. Crura fuse as a tripartite common tendon prior to insertion.
a. Superficial Head: Anterior to lacrimal sac
i. Inserts onto frontal process of the maxilla
ii. Provides majority of support for the medial canthus
b. Deep Head: Posterior to the lacrimal sac
i. Inserts onto the posterior lacrimal crest
ii. Less developed compared to the superficial head
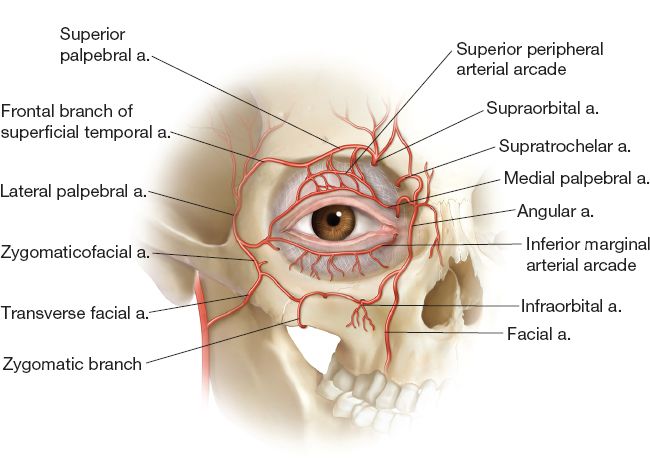
Figure 19-6. Arterial supply of the eyelids.
c. Vertical head: Forms roof of lacrimal sac
i. Inserts onto orbital process of the frontal bone
ii. Functions in the tear pump mechanism
F. Vascular system (Fig. 19-6)
1. Dual blood supply from both the external and internal carotid systems.
2. Marginal arcade is located 2 to 3 mm from the lid margin.
3. Peripheral arcade is located between the levator palpebrae superioris and Mueller’s muscle just above the superior tarsal margin.
4. Upper lid: Primarily supplied by branches of ophthalmic artery (internal carotid).
5. Lower lid: Primarily supplied by branches of facial artery (external carotid).
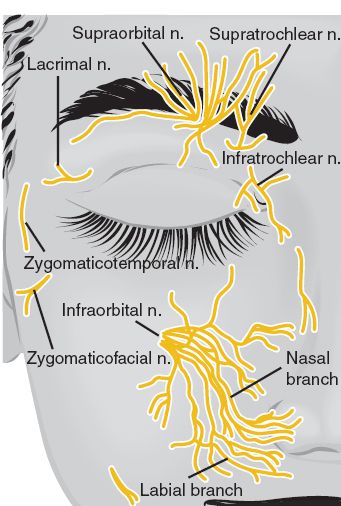
G. *Sensory innervation (Fig. 19-7)
1. Upper eyelid: Ophthalmic division of CN V (V1)
2. Lower eyelid: Maxillary division of CN V (V2)
II. CLINICAL EYELID MEASUREMENTS
A. Palpebral fissure: Distance between upper and lower lid margins (10 mm vertically and 30 mm horizontally)
B. Marginal reflex distance (MRD): Corneal light reflex to lid margin
1. Upper eyelid rests slightly below the superior limbus (MRD1 = 4 mm)
2. Lower eyelid rests at the inferior limbus (MRD2 = 5 mm)
C. Lateral canthus sits 1 to 2 mm above the medial canthus
D. Distance between lash line and supratarsal crease is 8 to 12 mm (women > men).
E. Ideal amount of pretarsal show is 2 to 3 mm in primary gaze
F. Distance from upper lid margin to brow: 22 mm
F. Highest point of the upper lid margin is just nasal to the mid-pupillary line, while the lowest point of the lower lid margin is just temporal to the mid-pupillary line.
G. *Asian upper eyelids are anatomically different than occidental upper eyelids.
1. *Absent supratarsal crease (lack of levator aponeurosis dermal insertion
2. *Decreased height of pretarsal segment (caudal fusion of orbital septum and levator aponeurosis)
3. *Increased fullness (increased amounts of ROOF and SOOF)
4. *Presence of epicanthal folds
Figure 19-7. Sensory innervation of the eyelids. (From Tasman W, Jaeger EA, eds. Duane’s Opthamology on CD-ROM. 2006 ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
III. PREOPERATIVE EVALUATION OF EYELID AND CANALICULAR FUNCTION
A. Visual acuity using a Snellen chart
B. Assessment of tear production and drainage
1. *Schirmer’s test
a. Place paper strip in inferior fornix for 5 minutes
b. Topical anesthetic can prevent reflexive tearing (false-positive)
c. More wetting on the paper strip means less eye dryness
i. Normal: Greater than 10 mm
ii. Abnormal: Less than 10 mm
2. Tear film break-up time
a. Add 2% fluorescein dye to the eye and observe junction of globe and lower lid margin for evaporation of tear film using slit lamp
b. Longer time to evaporation means the tear film is more stable
i. Normal: Greater than 10 seconds
ii. Abnormal: Less than 10 seconds
3. *Jones dye test
a. Determines patent lacrimal system versus functional obstruction
b. Jones I
i. Place 2% fluorescein in the inferior fornix and a cotton-tip applicator in the inferior meatus of the nose for 5 minutes
ii. Presence of fluorescein (positive) indicates patency
iii. Absence of fluorescein (negative) indicates obstruction
c. Jones II
i. Gently irrigate the puncta with saline after a negative Jones I
ii. Presence of fluorescein (positive) indicates distal partial obstruction at the nasolacrimal duct
iii. Absence of fluorescein (negative) indicates proximal partial obstruction at the puncta or canaliculi
iv. Complete reflux indicates complete obstruction
C. *Snap-back test to assess for lower lid laxity
1. Pull the lower eyelid away from the globe. Upon release, it should immediately return to its normal position without blinking.
2. If this takes longer than one second, then significant laxity is present.
D. *Hertel exophthalmometry evaluates the position of the anterior border of the globe in relation to the most anterior point of the lateral orbit rim.
1. Enophthalmos: Less than 14 mm
2. Exophthalmos: Greater than 18 mm
3. Greater than 2 mm difference between eyes is clinically significant
E. *Vector refers to the position of the anterior border of the globe in relation to the most anterior point of the inferior orbital rim on lateral view
1. Neutral vector: Vertical line (no inclination) from the cornea to the rim
2. Negative vector: Posteriorly inclined line from the cornea to the rim—increased risk of postoperative ectropion.
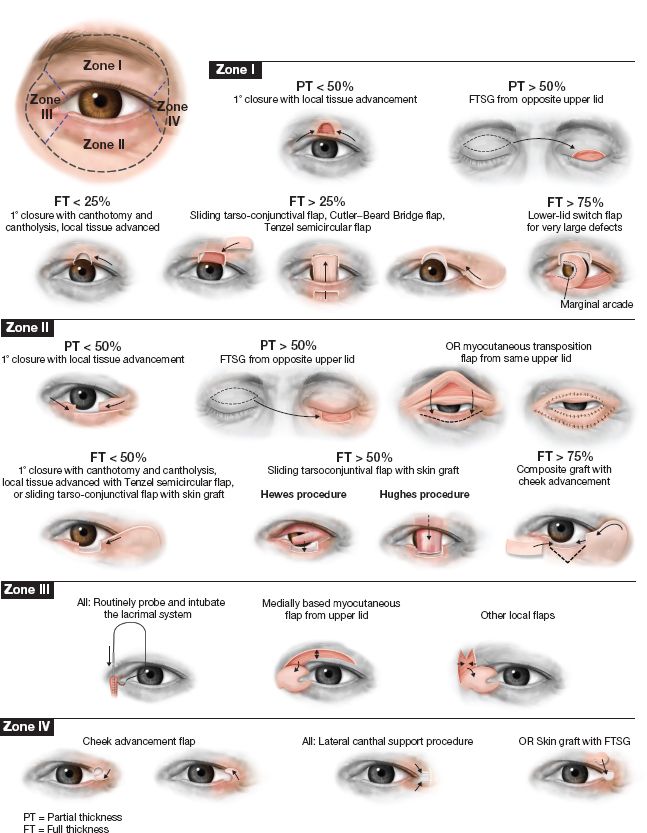
IV. RECONSTRUCTION OF EYELID AND CANTHAL DEFECTS (FIG. 19-8)
A. Lid margin repair
1. Rule out globe (loss of turgor) and septal injury (presence of orbital fat)
2. Missing tissue is unusual—Gap is due to pull of orbicularis oculi muscle
3. Align lid margin using a vertical mattress suture (6-0 silk) at the gray line
a. Evert wound edges to prevent postoperative notching
b. Secure long suture ends under skin sutures away from the cornea
4. Strength layer—Repair the tarsus using 5-0 or 6-0 absorbable suture
a. Partial-thickness bites protect the cornea from suture irritation
b. Bury all suture knots closer to the skin than to the conjunctiva
5. Close skin using 6-0 nylon suture (no conjunctival sutures required)
6. Remove skin sutures in 5 days and lid margin sutures in 7 to 10 days
7. Complications: Notching (most common), trichiasis, and eyelash alopecia
B. Partial-thickness defects (Fig. 19-8)
1. Anterior lamellar defects
a. Less than 50%: Local tissue rearrangement
b. *Greater than 50%: Skin graft from contralateral lid (preferred)
c. Avoid vertical incisions to prevent postoperative lid retraction.
2. Posterior lamellar defects
a. Involves conjunctiva only: Primary repair for smaller defects and nasal/buccal mucosal or amniotic membrane grafts for larger defects.
b. Involves tarsus and conjunctiva: Primary repair for smaller defects and nasal chondromucosal (septal cartilage), ear cartilage, donor scleral, or hard palatal mucosal grafts for larger defects.
C. Full-thickness defects of the upper eyelid (Fig. 19-8)
1. Less than 25%
a. Primary closure with meticulous lid margin repair.
b. In elderly patients, pre-existing laxity may allow closure up to 40%.
2. Between 25% to 75%
a. Lateral canthotomy and cantholysis with primary closure.
b. Tenzel semicircular flap: Lateral canthotomy and cantholysis with advancement of lateral myocutaneous flap
c. Switch flap: Lid sharing between the ipsilateral lower eyelid and a central upper lid defect. Flap is divided and inset 3 weeks later.
3. Greater than 75%
a. *Cutler–Beard flap
i. First stage: Full-thickness flap is developed in the ispilateral lower eyelid below the inferior tarsus—flap width equals the defect size—and passed beneath the lower lid margin into the upper lid defect (may include cartilage for additional support).
ii. Second stage: Flap is divided and inset 3 weeks later.
Figure 19-8. Eyelid reconstruction. FT, full thickness; PT, partial thickness.
b. Paramedian or temporal forehead flaps are reserved for extensive upper lid defects when other local options are not available.
c. Free tarsoconjunctival graft from contralateral lid
D. Full-thickness defects of the lower eyelid (Fig. 19-8)
1. Less than 25%: Refer to full-thickness defects of the upper eyelid
2. Between 25% to 75%
a. Lateral canthotomy and cantholysis with primary closure or Tenzel semi-circular flap.
b. Unipedicled myocutaneous Fricke transposition flap: Ipsilateral upper lid skin–muscle flap based on either a medial or lateral pedicle is transposed into a lower lid defect.
c. Bipedicled myocutaneous Tripier flap: Similar to the Fricke flap, except based on both the medial and lateral pedicles.
a. *Hughes tarsoconjunctival flap
i. First stage: Ipsilateral upper lid conjunctiva and a portion of the superior tarsus (must leave 4 mm for upper lid support) are transferred into a lower lid defect and covered with a full-thickness skin graft. Mueller’s muscle is included in smokers.
ii. Second stage: Flap is divided and inset 3 weeks later
b. Mustardé cheek rotation-advancement flap
i. Combine with mucosal graft for total lower lid defects.
ii. Anchor to the deep temporal fascia and the periosteum of the infraorbital rim to prevent postoperative ectropion.
iii. Subcutaneous plane: For a thinner flap
iv. Deep plane: Prevents distal flap necrosis in smokers
E. Lateral canthal defects (Fig. 19-8)
1. Produces a rounded lateral canthus and a shortened palpebral fissure.
2. Simple disruption: Primary repair if both ends of the LCT are present
3. Complex disruption: Canthoplasty if lateral end of the LCT is absent
a. Medial end present: Suture to periosteum of lateral orbital rim
b. Medial end absent: Use lateral tarsal strip or periosteal flap
4. Canthopexy for LCT laxity—slight overcorrection prevents recurrence.
5. A local flap, regional flap, or skin graft can be used for soft tissue coverage.
F. Medial canthal defects (Fig. 19-8)
1. Rule out injury to the canalicular system.
2. Simple disruption: Primary repair if both ends of the MCT are present
3. Complex disruption: Canthoplasty if medial end of the MCT is absent. *If avulsed, may require transnasal wiring (posterosuperior to the posterior lacrimal crest) to prevent postoperative telecanthus.
4. Canthopexy for MCT laxity—slight overcorrection prevents recurrence.
5. A local flap, regional flap, or skin graft can be used for soft tissue coverage.
V. RECONSTRUCTION OF THE CANALICULAR SYSTEM
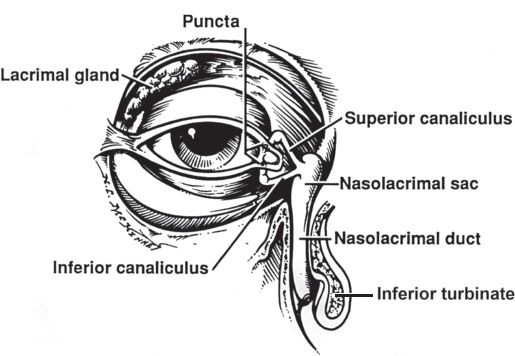
A. Lacrimal apparatus (Fig. 19-9)
1. Lacrimal gland
a. Located within the lacrimal fossa in the superolateral orbit.
b. Lateral horn of the levator aponeurosis separates the orbital and palpebral lobes with approximately 10 to 12 ducts passing from the orbital lobe through the palpebral lobe into the superior fornix.
c. Supplied by the lacrimal artery, a branch of the ophthalmic artery.
d. The lacrimal vein empties into the superior ophthalmic vein.
e. Lacrimal nerve via ophthalmic division of CN V provides sensation.
f. Pterygopalatine ganglion provides parasympathetic innervation.
g. Superior cervical ganglion provides sympathetic innervation.
2. Tears
a. Tear film is composed of a trilaminar fluid layer
i. Outer lipid layer: Meibomian glands, accessory sebaceous glands of Zeis and Moll—prevents tear evaporation
ii. Middle aqueous layer: Lacrimal gland, accessory lacrimal glands of Krause and Wolfring—90% tear film thickness
iii. Inner mucoprotein layer: Goblet cells—hydrophilic and facilitates tear film distribution across the globe
b. Functions of tear film
i. Provides lubrication to promote a smooth gliding surface
ii. Mechanically removes foreign bodies and other irritants
iii. Increases the refractive power of incoming light
iv. Provides 80% to 90% of the cornea’s oxygen requirement
v. Contains lysozyme that imparts antimicrobial properties
c. Tear pump mechanism
i. Lacrimal puncta open into the superior and inferior canaliculi at medial end of the upper and lower lids, respectively
Figure 19-9. The lacrimal system. (From Mills SE, ed. Histology For Pathologists. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.)
ii. Both canaliculi travel 2 mm vertically and then 6 to 8 mm horizontally before uniting to form the common canaliculus
iii. The common canaliculus empties into the lacrimal sac through the valve of Rosenmüller
iv. The lacrimal sac empties into the nasolacrimal duct which travels 18 mm inferiorly before entering the inferior meatus
v. Nasolacrimal duct opening is covered by a mucosal fold (valve of Hasner) to prevent reflux of air and nasal contents
vi. *Eyelids open: Sac is empty, diaphragm is in resting position, canaliculi at normal length, and puncta are open
vii. *Eyelids close: Diaphragm is pulled laterally creating negative pressure within the sac, the canaliculi shorten, the puncta close, and the sac fills with tears
viii. *Eyelids reopen: Diaphragm returns to its resting position expelling tears into the nasolacrimal duct
B. Canalicular repair
1. Recommended to prevent postoperative epiphora
2. Identify both the proximal and distal ends of the lacerated canaliculus
a. Proximal end is more difficult to find, usually more posterior
b. Irrigation of the uninjured canaliculus aids in the identification of the proximal end by observing for the backflow of saline
3. Use an indwelling silicone stent to bridge the laceration
4. Some authors recommend microsurgical anastomosis of the lacerated canaliculus over the stent, while others recommend simple reapproximation of the orbicularis oculi muscle and repair of the MCT
5. The stent should be left in place for at least 12 weeks
C. Lacrimal bypass surgery for a blocked lacrimal drainage system
1. Silicone tube intubation: Obstructions at the lacrimal puncta
2. Conjunctivodacryocystostomy: Obstructions at the canalicular level
3. Conjunctivodacryocystorhinostomy: Also for obstructions at the canalicular level, or in patients with congenital absence of the lacrimal sac—requires use of a permanent Pyrex glass tube (Jones tube)
4. *Dacryocystorhinostomy (DCR): Obstructions at the nasolacrimal duct
5. Canaliculodacryocystorhinostomy: Obstructions at the junction of the common canaliculus and lacrimal sac—combination of DCR and microsurgical repair of the stenotic common canaliculus
A. Mechanics of eyelid function
1. Refer to Section “Eyelid Anatomy and Physiology”
2. True ptosis: Drooping of the lid margin below its normal anatomic position due to levator complex dysfunction.
3. Pseudoptosis: Lid margin appears low, but levator complex is normal
a. Brow ptosis
b. Enophthalmos (e.g., posttraumatic, iatrogenic)
c. Hypotropia (after an orbital floor fracture)
d. Blepharochalasis: Recurrent episodes of eyelid edema in young women which stretches the eyelid tissue over time
e. Contralateral exophthalmos with associated upper lid retraction (e.g., Graves’ ophthalmopathy)
f. Duane syndrome: Limited abduction of the affected eye due to absent CN VI and aberrant innervation of the lateral rectus muscle by CN III, resulting in impaired movement followed by fibrosis of the extraocular musculature and subsequent globe retraction
B. Preoperative evaluation of ptosis
1. Refer to Section “Preoperative Evaluation of Eyelid and Canalicular Function”
2. Degree of ptosis: Decrease in MRD1
a. Mild: 1 to 2 mm
b. Moderate: 3 mm
c. Severe: Greater than 4 mm
3. Levator function (excursion): Examiner uses nondominant hand to stabilize the patient’s brow and measures the distance between the upper lid margin in maximal downgaze compared to maximal upgaze
a. Good: 10 to 15 mm
b. Fair: 6 to 9 mm
c. Poor: Less than 5 mm
4. *Elevated Supratarsal Crease: Levator dehiscence
5. CN III palsy or Horner’s syndrome (triad of miosis, anhidrosis, and partial ptosis)
6. Hering’s law of equal innervation
a. Severe ptosis may mask a contralateral mild ptosis because each levator complex receives the same amount of neural input determined by the more ptotic eyelid.
b. If not recognized preoperatively, then it may become more prominent after corrective surgery because the amount of neural input to both levator complexes will be diminished
c. Hering’s test: Examiner uses nondominant hand to stabilize the patient’s brow and elevates the ptotic eyelid with a cotton-tip applicator while simultaneously observing for contralateral ptosis
C. Classification of ptosis
1. Involutional (senile)
a. Most common type of ptosis due to aging
b. *Levator aponeurosis stretches or dehisces from the tarsus, but dermal insertions are preserved causing the supratarsal crease to rise
c. Levator function often remains good
2. Traumatic
a. Due to direct injury of the levator complex
b. Either the muscle itself or the nerve can be involved
3. Neurogenic (paralytic)
a. *Myasthenia gravis
i. Ptosis that worsens with activity and improves with rest.
ii. Diagnosed by the intravenous administration of edrophonium or neostigmine causing temporary relief of the ptosis.
b. CN III palsy or Horner’s syndrome can cause paralysis of the levator palpebrae superioris or Mueller’s muscle, respectively.
a. Due to excess weight from tumor infiltration or dermatochalasis
b. Also caused by tissue edema in the early postoperative period
5. Congenital
a. Due to fibrofatty replacement of the levator complex.
b. The supratarsal crease may be absent.
c. Levator function often remains poor.
d. Classic finding on physical examination is lagophthalmos on downward gaze (i.e., the ptotic eyelid remains higher than the contralateral side on downward gaze due to levator fibrosis).
e. Surgical correction is delayed until age 3 to 5 years unless corneal exposure risks ulceration or visual field obstruction risks amblyopia.
f. *Associated with blepharophimosis syndrome, which consists of the triad of telecanthus, bilateral ptosis, and epicanthus inversus.
g. Marcus Gunn jaw-winking phenomenon
i. Synkinetic movement of the upper eyelid and jaw due to aberrant crossover from the motor branch of the lateral pterygoid muscle (mandibular division of CN V) to the superior division of CN III.
ii. At rest, the upper eyelid is ptotic, but with jaw opening it briefly elevates simulating a “wink”.
D. Nonsurgical Management of Ptosis
1. If myasthenia gravis is suspected, referral to a neurologist is warranted.
2. Alpha-adrenergic agonist drops if the cause is botulinum toxin injection or Horner’s syndrome (stimulates Mueller’s muscle contraction).
3. If the patient wears eyeglasses, they can be modified with a projecting flange to support the drooping upper eyelid.
E. Surgical management of ptosis
1. Intravenous sedation is preferred to be able to wake the patient up during surgery and accurately assess the degree of ptosis correction
2. Degree of ptosis and levator function determine the type of ptosis repair
a. Good levator function/mild ptosis
i. Levator plication: Levator aponeurosis is plicated—1:1 ratio of millimeter plication to ptosis correction suffices for mild ptosis, but a 4:1 ratio is required for more severe ptosis.
ii. Levator advancement: Levator aponeurosis is released from its insertion on the tarsus and advanced—1:1 ratio of millimeter advancement to ptosis correction suffices for mild ptosis, but a 4:1 ratio is required for more severe ptosis.
iii. *Tarsoconjunctival mullerectomy (Fasanella-Servat procedure): Conjunctiva, tarsus, and Mueller’s muscle are removed en bloc via a posterior approach—*4:1 ratio of millimeter resection to ptosis correction is required. If the tarsus is spared, it is called the Putterman procedure.
b. Good levator function and moderate ptosis: Levator plication or advancement.
c. Good levator function and severe ptosis: Levator advancement only
d. Fair levator function and any ptosis: Levator advancement only
e. Poor levator function and any ptosis: *Frontalis sling or suspension
i. Most often used in cases of congenital ptosis
ii. Relies on movement of the frontalis muscle to provide lid excursion by slinging the upper eyelid to the brow
iii. Patients require nocturnal eye protection and lubrication due to lagophthalmos while sleeping.
iv. Our preference is to use autologous tissue (e.g., fascia lata, palmaris longus tendon), but alloplastic material can also be used (e.g., silicone, Gore-Tex, Alloderm).
v. Modified Crawford technique
a) Four stab incisions are made just above the lash line and three just above the brow.
b) Two strips of fascia lata are tunneled beneath the orbicularis oculi muscle from the upper eyelid to the brow forming two opposing triangles.
c) The degree of ptosis correction is tailored by tightening the knots to the desired tension.
VII. ECTROPION
A. Defined as eversion, or rolling outward of the lid margin.
B. Loss of normal lid-globe apposition leads to scleral show, keratinization of the exposed cornea and conjunctiva, and ultimately loss of vision.
C. Nonsurgical management of ectropion
1. It is important to protect the cornea and prevent dryness with artificial tears, taping of the eyelid, and eye patches or moisture shields.
2. If scarring is present, consider digital massage or steroid injections.
3. Punctal occlusion can help relieve dryness
4. Treat infection, if present
D. Classification and surgical management of ectropion
1. Involutional (senile)
a. Most common type of ectropion due to aging
b. *Hallmark feature is horizontal lid laxity
c. Surgical repair
i. Medial conjunctival spindle procedure: Medial conjunctiva and retractor muscles are horizontally excised.
ii. Kuhnt–Szymanowski procedure: Subciliary blepharoplasty combined with shield excision of redundant orbicularis oculi muscle, middle lamella, and posterior lamella.
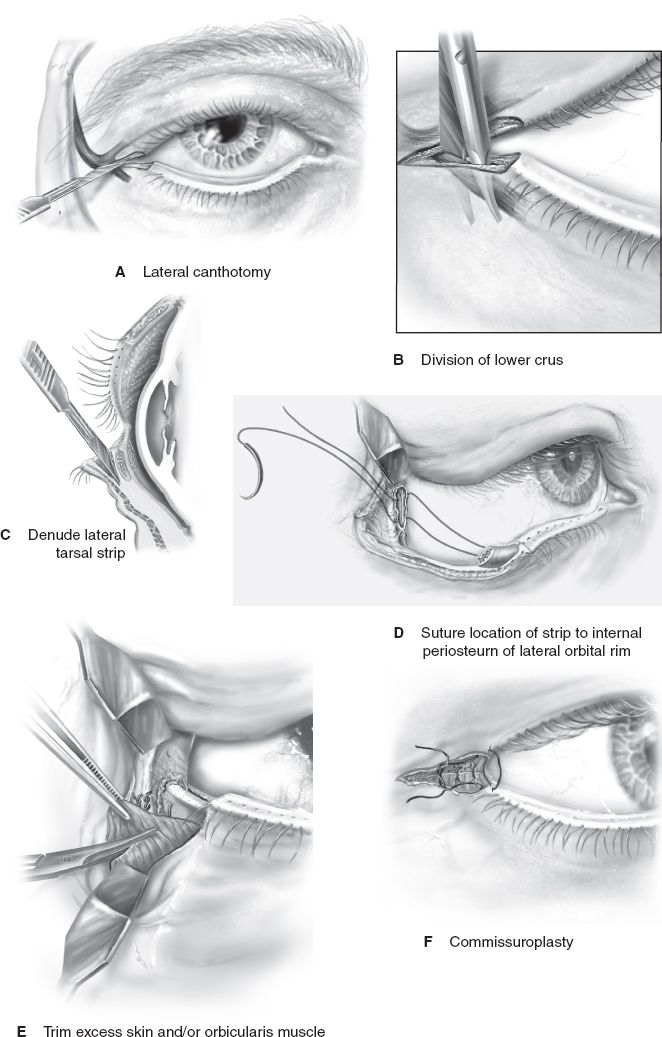
iii. *Lateral tarsal strip procedure (canthoplasty) (Fig. 19-10)
a) Lateral canthotomy followed by cantholysis of the inferior crus of the LCT.
b) A strip of lateral tarsus is then denuded and sutured to the periosteum of the lateral orbital rim with slight overcorrection.
c) Excess skin and orbicularis oculi muscle is excised, and a commisuroplasty is performed.
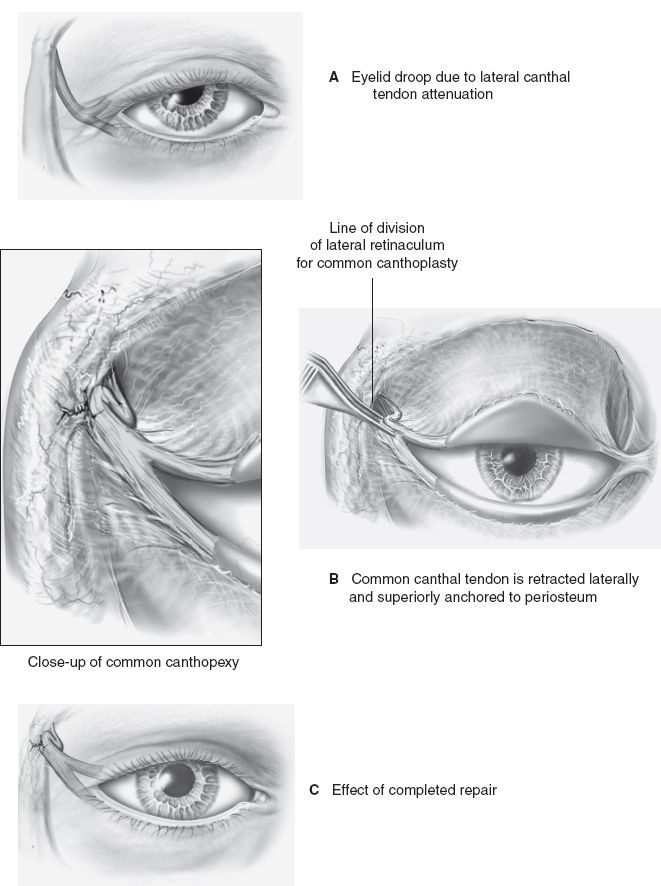
iv. Standard canthopexy (Fig. 19-11): The lax LCT is retracted laterally and either plicated or sutured to the periosteum of the lateral orbital rim. This technique differs from a canthoplasty in that no cantholysis is performed.
2. Neurogenic (paralytic)
a. Due to a deficit in CN VII function
b. Neurotrophic keratitis associated with absent corneal sensation
c. Surgical repair
i. If poor Bell’s phenomenon, a tarsorrhaphy can be helpful
ii. Botulinum toxin injection of the levator palpebrae superioris or gold weight implantation may be a useful adjunct in patients with lagophthalmos
iii. Mild cases: Lateral tarsal strip with or without midface lift
iv. Severe cases: A static sling is recommended
3. Cicatricial
a. Due to scarring in or around the anterior lamella
b. Surgical repair
i. If conservative measures fail (e.g., digital massage, steroid injections), then treatment involves surgical release of the scar and lengthening of the anterior lamella once the scar is mature
ii. In some cases, tension can be reduced by local tissue rearrangement in the form of V-, Y-, or Z-plasties
iii. Additional tissue often needed in the form of local flap, regional flap, or skin graft (full-thickness preferred)
iv. Temporary traction suture taped to the forehead is used postoperatively to counteract downward pull of tissue edema
Figure 19-10. The lateral tarsal strip procedure.
Figure 19-11. Standard canthopexy.
4. Mechanical
a. Due to excess weight from tumor infiltration or dermatochalasis
b. Also caused by tissue edema in the early postoperative period
c. Surgical repair
i. Excision of the offending agent followed by eyelid reconstruction as outlined above depending on defect size
ii. If tissue edema is responsible, initial recommendations include head of bed elevation and expectant management. Improves in 2 to 3 months when new lymphatic channels form.
a. Least common type of ectropion due to vertical deficiency of the anterior lamella
b. Rarely an isolated finding—usually associated with blepharophimosis syndrome
c. May be complicated by a neurogenic (paralytic) component
d. Surgical repair
i. Manage initially with artificial tears and lubrication to see if it spontaneously resolves on its own
ii. May require a temporary tarsorrhaphy, but avoid prolonged use to prevent iatrogenic amblyopia
iii. Severe cases will require skin grafts or local flaps and are usually performed in conjunction with medial and lateral canthoplasties and ptosis repair
VIII. ENTROPION
A. Defined as inversion, or rolling inward of the lid margin
B. Patients usually complain of epiphora, and corneal irritation occurs due to posteriorly directed eyelashes (trichiasis)
C. Nonsurgical management of entropion
1. Protection of the cornea is paramount with use of artificial tears, eye patches or moisture shields, and electrolysis or argon laser to remove irritating eyelashes (or wear contact lens to deflect eyelashes)
2. Taping of the eyelid to the cheek may assist in everting the lid margin
3. Treat infection, if present
D. Classification and surgical management of entropion
1. Involutional (senile)
a. Most common type of entropion due to aging
b. *Hallmark features are horizontal lid laxity, disinsertion of the retractor muscles, and an overriding preseptal segment.
c. Surgical repair
i. Quickert procedure: Multiple sutures are placed below and perpendicular to the lid margin to evert the eyelid. Results are temporary and recurrence is expected.
ii. If horizontal lid laxity is the prominent finding, a lateral tarsal strip procedure is recommended.
iii. If vertical lid laxity is the prominent finding, reattachment of the capsulopalpebral fascia to the tarsus is required.
iv. Weis procedure: Full-thickness rotational procedure of the lid margin back to its normal position involving a transverse blepharotomy and a lateral tarsal strip procedure.
2. Acute spastic
a. Due to ocular irritation or inflammation leading to sustained contraction or overactivity of the orbicularis oculi muscle.
b. Surgical repair
i. Temporizing measures include taping of the eyelid, local anesthetic infiltration, or botulinum toxin injection into the orbicularis oculi muscle, which can sometimes break the spasm and lead to resolution of the lid malposition
ii. If horizontal or vertical lid laxity also exist, then a lateral tarsal strip procedure or reattachment of the capsulopalpebral fascia to the tarsus may be required, respectively
3. Cicatricial
a. Due to scarring in or around the posterior lamella.
b. More common in underdeveloped nations as a result of trachoma.
c. Surgical repair
i. Do not operate if the conjunctiva is actively inflamed.
ii. Treatment involves surgical release of the scar and marginal rotation. Conjunctiva is replaced with either nasal mucosa, buccal mucosa, or amniotic membrane.
iii. If the tarsus is also missing or deformed, it can be fractured and repositioned, or replaced with an interpositional graft
a. Least common type of entropion due to vertical deficiency of the posterior lamella
b. Rarely an isolated finding caused by dysgenesis of the retractor muscles or structural abnormalities of the tarsus
c. *Commonly confused with epiblepharon in which a congenital horizontal redundant fold of skin is located near the lid margin due to the abnormal insertion of the pretarsal orbicularis oculi muscle. No rotational lid margin abnormality exists with epiblepharon and it may resolve spontaneously, which differs from congenital entropion.
d. Surgical repair
i. Congenital entropion: Transverse blepharotomy with marginal rotation is performed
ii. Epiblepharon: Elliptical excision of the redundant skin and muscle is performed
PEARLS
1. Asian upper eyelids have an absent supratarsal crease, more caudal fusion of the orbital septum with the levator aponeurosis, increased amounts of ROOF and SOOF, and presence of epicanthal folds
2. Lateral canthotomy and cantholysis may facilitate primary closure of eyelid defects
3. In Graves’ ophthalmopathy, first perform orbital decompression, followed by strabismus surgery, and finally eyelid reconstruction
4. Take photographs both pre- and postoperatively for documentation
5. Avoid vertical scars on or near the eyelid to prevent postoperative ectropion
6. If levator function is good, the choice of ptosis repair is either levator plication or advancement
7. If levator function is poor, the choice of ptosis repair is frontalis sling or suspension
8. Aging is the most common cause of ptosis, ectropion, and entropion
9. The most important thing to remember about any eyelid procedure is to protect the cornea!
QUESTIONS YOU WILL BE ASKED
1. What is the most common complication following lower lid procedures?
Lower lid malposition
2. What structure attaches to the superior margin of the tarsus and is often visualized in cases of levator dehiscence?
Mueller’s muscle
3. Patients with a negative vector are at increased risk for what postoperatively?
Xerophthalmia
4. What ratio of levator plication/advancement is usually required for adequate ptosis correction?
4:1
THINGS TO DRAW
Draw the upper and lower eyelid in cross section.
Recommended Readings
Cherubini TD. Entropion and ectropion of the eyelids. Clin Plast Surg. 1978;5(4):583–591. PMID: 729343.
Codner MA, McCord CD, Mejia JD, Lalonde D. Upper and lower eyelid reconstruction. Plast Reconstr Surg. 2010;126(5):231e–245e. PMID: 21042070.
DiFrancesco LM, Codner MA, McCord CD. Upper eyelid reconstruction. Plast Reconstr Surg. 2004; 114(7):98e–107e. PMID: 15577335.
McCord CD Jr. The evaluation and management of the patient with ptosis. Clin Plast Surg. 1988; 15(2):169–184. PMID: 3280214.
Spinelli HM, Jelks GW. Periocular reconstruction: a systematic approach. Plast Reconstr Surg. 1993; 91(6):1017–1024; discussion 1025–1026. PMID: 8479966.
< div class='tao-gold-member'>