CHAPTER 5 Eyelid and Midcheek Anatomy
Eyelid
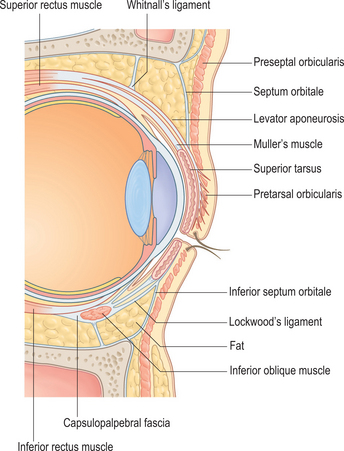
The eyelids are complex dynamic structures that protect the globes while providing a sufficient and appropriately located aperture for vision regardless of the location of the pupil. In higher species, the lids have also assumed a role in facial expression. These functions can only be achieved by the balanced interaction of many individual anatomical structures. It is fundamental in eyelid surgery to appreciate the two distinct surgical lamellae of the lids. The superficial and deep lamellae are fused in the pretarsal area. However, they are separate in the preseptal area and this separation allows mobility of the anterior lamella, the cheek part of the lid separate from the deep lamella, the orbital part of the lid.
Eyelid anatomy
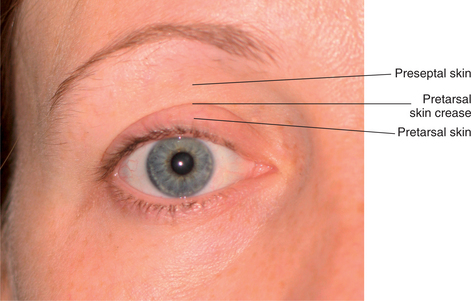
Surface anatomy and skin
The appearance of the ‘eye’ is largely determined by the shape of the palpebral fissure and its position relative to the globe. This aperture between the upper and lower eyelid margins measures 28–30 mm horizontally and 10–12 mm vertically. The upper lid covers up to 2 mm of the upper cornea, with the lower lid typically crossing at the level of the lower corneoscleral limbus. The point of maximum lid margin concavity differs in the two lids: in the upper lid it is medial to the pupil and in the lower it is lateral (Fig. 5-1).
The lid margins are 2 mm wide, with the posterior margin being sharp and applied to the globe. The anterior margin is rounded and holds the eyelashes. The grey line, visible along the middle of each lid margin and formed by the gap between the pretarsal tissue and the underlying tarsal plate, marks the junction of the skin and conjunctiva. The Meibomian glands that contribute to the tear film, reside within the substance of the tarsal plate giving rise to openings just behind the grey line. The apocrine sweat glands of Moll and the specialized sebaceous glands of Zeis are found just anterior to the grey line in association with the lash follicles. Eccrine sweat glands and conventional sebaceous glands are found throughout the eyelid skin, although the sebaceous glands are more numerous on the medial half, contributing to the skin’s smoother and oilier texture medially.
The skin crease of the upper eyelid typically overlies the superior border of the tarsus and is referred to as the supratarsal skin crease. Fascial bands from the underlying pretarsal extension of the levator palpebrae pass through the orbicularis oculi muscle and insert into the pretarsal dermis, maximal near the lash line passing up to the level of the crease (Fig. 5-2). The preseptal skin superior to the crease is comparatively non-adherent and mobile with a degree of laxity to allow movement of the lid. This relatively lax skin hangs over the supratarsal crease to create the supratarsal fold. In the oriental eyelid, the supratarsal skin crease is less well-defined and lower set on the upper lid due to the low insertion of the levator aponeurosis closer to the lashes.
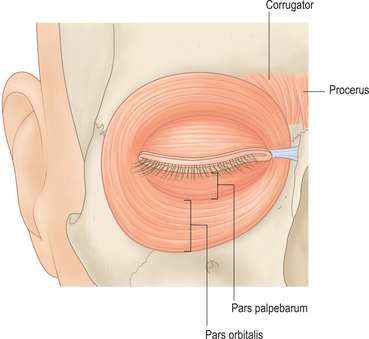
Orbicularis oculi
The orbicularis oculi is the sphincter of the eyelid consisting of two distinct parts: the pars palpebarum and the pars orbitalis (Fig. 5-3). The pars palpebarum overlies the aperture of the orbit within the eyelids and is further subdivided into pretarsal and preseptal parts. The pretarsal part is supported by its close adherence to the tarsal plates and the preseptal part is more mobile overlying the orbital septum in both upper and lower lids. Both the pretarsal and preseptal parts have superficial and deep components medially that are connected to the orbital wall at the medial canthus in a complex anatomical arrangement that is linked to the drainage of the lacrimal sac. Laterally, the muscle fibers do not have a direct bony attachment, but are stabilized to the orbital rim by a ligamentous connection at the lateral canthus. The pars orbitalis is more extensive and less compacted than conventionally described. Superiorly it overlies the lower forehead, lower frontalis and corrugator supercilii muscles, giving off a slip of muscle to form the depressor supercilii. Inferiorly the sheet of orbicularis lies flat across the cheek with a variable descent towards the upper lip. Classical anatomists have labeled this part the muscularis malaris, reflecting its extensive midfacial distribution. It is now considered to be part of the superficial musculoaponeurotic (SMAS) layer (see midcheek section below).
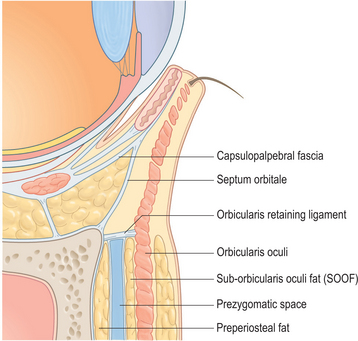
At the junction of the lower lid with the cheek, the orbicularis oculi muscle is attached to the orbital rim at the junction of the pars palpebarum above and the pars orbitalis below. This is a direct muscle attachment medially, from the anterior lacrimal crest to approximately the level of the medial limbus. This tight attachment is largely responsible for the appearance of the nasojugal groove. Lateral to this point, the attachment is continued indirectly through a fibrous connection known as the orbicularis retaining ligament, as far as the lateral canthal region1 (Fig. 5-4). This ligament spans from the periosteum just outside the orbital rim to the fascia on the under-surface of the orbicularis. It can be considered to be a specific part of the ‘peri-orbital septum’2 and has also been described as the ‘orbitomalar ligament’.3 The location of the attachment to the orbicularis correlates with the position of the palpebromalar groove, which appears on the surface of the overlying skin with aging. In the lateral canthal region, the orbicularis retaining ligament expands and merges with a dense fibrous condensation between the superficial and deep fascia lateral to the lateral commissure known as the lateral orbital thickening.1
The microanatomy of the orbicularis reflects its unique function. The myofibers are the smallest of all skeletal muscles and there are distinct microarchitectural differences within the muscle itself. The finest and shortest fibers are in the pretarsal region, progressively increasing in size away from the lid margin. Individual fibers do not extend the full length of the lid and not all myofibers attach to the canthal ligaments. Rather, there is an overlapping arrangement of short myofibers with the pretarsal fibers averaging one-third of the lid length and the preseptal half the lid length, although considerable variation exists.4 Of importance for Botox use is the location of the neuromuscular junctions, which are concentrated at the canthal ends, more laterally. Each fiber has a single innervation and similar to the extraocular muscles, the motor units are small consistent with fine motor control. The dominant fiber type (90%) are fast twitch, fatigueable with low vascularity that are suited to brief, rapid blink movements.5
Eyelid support
The medial canthus is medial to the globe with a rigid fixation to the orbital wall. By contrast, the lateral commissure overlies the lateral part of the globe and is mobile, having up to 6 mm of vertical movement and 2 mm of lateral movement.6 These anatomical landmarks are determined by the medial and lateral palpebral ligaments, which provide the ligamentous support for the tarsal plates. The palpebral ligaments are commonly referred to as the medial and lateral canthal tendons on account of the pretarsal orbicularis fibers that contribute to their superficial surfaces. In addition, the orbicularis muscle and more particularly the fascia on its deep surface forms a continuous fibrous network of support through the orbicularis attachment to the tarsal plates and canthal tendons, and to the lateral orbital rim via the firm fibrous attachment provided by the orbicularis retaining ligament and the lateral orbital thickening.
Medial canthus
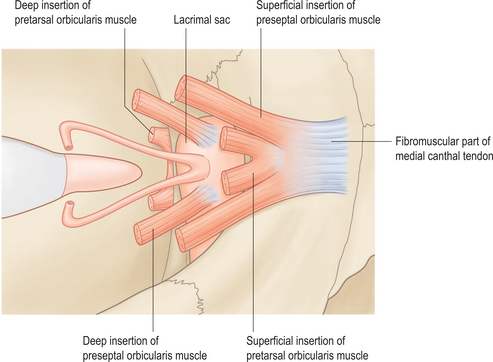
The pretarsal orbicularis muscle inserts medially by a superficial head and a deep head (Fig. 5-5). The superficial head from each lid blends with the fibrous continuation of the tarsal plates to form the anterior part of the medial canthal tendon. The deep head from each lid is also known as the pars lacrimalis, or Horner’s muscle. Its fibers begin at the medial end of the tarsal plates and insert into the posterior lacrimal crest just behind the lacrimal sac. The preseptal muscle also inserts medially by a superficial and deep head. The superficial head from each lid inserts into the upper and lower borders of the medial canthal tendon. The deep heads insert into the fascia overlying the lacrimal sac and the medial orbital wall above and below Horner’s muscle. Closing the eyelids leads to traction on the deep heads which pulls the lacrimal sac fascia laterally, producing a negative internal pressure.7
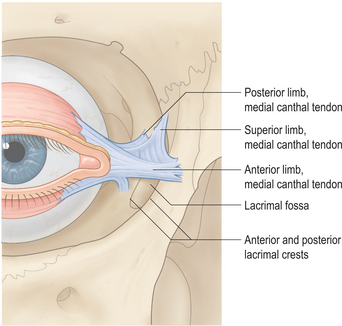
The medial canthal tendon inserts into the frontal process of the maxilla in a tripartite manner: anterior and posterior horizontal elements and a vertical element (Fig. 5-6). The anterior horizontal insertion point is onto the anterior lacrimal crest, level with the upper part of the lacrimal sac. The posterior part leaves the deep surface just before the anterior lacrimal crest and inserts into the posterior lacrimal crest behind the sac. The tendon has a definite inferior margin but the superior border blends with the periosteum having vertically orientated fibers that insert into an ill-defined portion of the medial orbital rim at or close to the nasofrontal suture. This vertical component of the medial canthal tendon is thought to be responsible for suspension and fixation of the medial canthus, while the horizontal components are relatively weak and contribute little to medial canthal stability.8
Lateral canthus
Despite varied anatomical descriptions and nomenclature, the lateral canthus should be considered in terms of a deep skeletal attachment via the lateral canthal tendon and a superficial fibrous attachment via the lateral canthal raphe and lateral orbital thickening. The deep attachment serves to stabilize the tarsal plates whereas the superficial attachment functions to stabilize the orbicularis over the orbital rim.6
The lateral canthal tendon is less well defined than the medial side and has less orbicularis muscle connection. It takes the form of a Y-shaped fibrous condensation measuring 6 mm in transverse length and up to 10 mm in vertical height. It extends from the upper and lower tarsal plates and is reinforced by significant attachments from the lateral horn of the levator aponeurosis and the check ligament of the lateral rectus muscle as well as from Lockwood’s ligament. This confluence of structures (the lateral retinaculum) attaches to the lateral orbital wall at Whitnall’s tubercle, which is located just inside the orbital rim and approximately 10 mm below the zygomaticofrontal suture.9 Whitnall’s (superior transverse) ligament is part of the levator aponeurosis and is not part of the lateral canthus.
Superficially, the preseptal orbicularis fibers of the upper and lower lid interdigitate to form the lateral canthal raphe. The raphe, although often referred to in eyelid texts, has not been clearly described and is difficult to identify as a discrete anatomical structure. It is connected on its deep surface to the underlying septum orbitale and merges laterally with a significant confluence of fibrous tissue known as the lateral orbital thickening1 (Fig. 5-7). This thickening is a condensation of fascia passing over the orbital rim, lateral and superficial to the lateral canthal tendon. It has also been termed the ‘superficial leaf of the lateral canthal tendon’10 and the ‘precanthal web’.11 It is a triangular fibrous adhesion connecting the orbicularis fascia on the under-surface of the muscle to the underlying deep fascia, which in this region is made up of thickened lateral orbital rim periosteum and adjacent deep temporal fascia. The lateral orbital thickening is continuous with the orbicularis retaining ligament inferomedially and must be released surgically if a canthoplasty is to be effective.
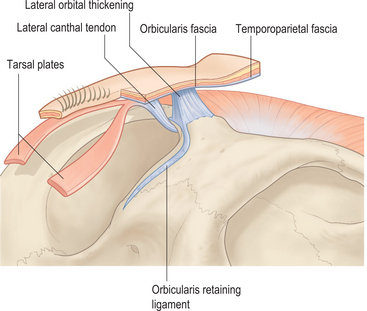
Figure 5-7 Lateral canthus (view from inferiorly).
Modified from Muzaffar AR, Mendelson BC, Adams WP. Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg 2002; 110:873–884.
The lateral canthus is positioned approximately 2 mm higher than the medial canthus. Despite previous assumptions, this is the same for both sexes and does not change with increasing age.12 Inherent variations of the intercanthal angle do, however, have a significant impact on facial aesthetics in normal people and descent of the lateral commissure secondarily to lateral canthal tendon laxity produces an apparent change in the lateral canthus position, which predisposes to a premature aging appearance.
Tarsus and septum orbitale
The tarsal plates are crescentic-shaped, dense condensations of connective tissue that maintain the structural integrity of the eyelids while accommodating the contour of the globe. The upper tarsus is approximately 29 mm long and extends from the lateral commissure to the punctum medially. It is 10 mm wide in the central eyelid, narrowing medially and laterally. The lower tarsus is a similar length to that of the upper but is only 4–5 mm wide at its center. The septum orbitale, or orbital septum, consists of a thin fibroelastic membrane of varying consistency that is notably non-distensible adjacent to the inferolateral orbital rim. It extends from the bony margin towards the tarsus and represents the continuation of the orbital periosteum. At the junction where the periosteum and septum fuse along the orbital rim is a dense white fibrous band termed the arcus marginalis (Fig. 5-8). The arcus marginalis is clearly evident inferomedially where the rim has a sharp edge, whereas it is less defined on the rounded inferolateral rim.
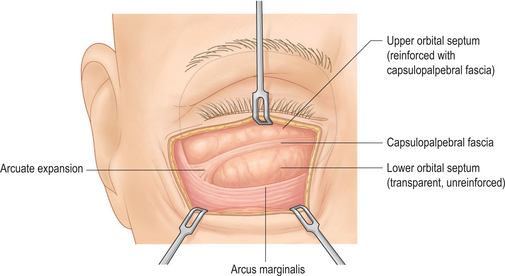
Figure 5-8 Septum orbitale and capsulopalpebral fascia of the lower lid.
Modified from Mendelson BC. Fat preservation technique of lower-lid blepharoplasty. Aesth Surg J 2001; 21:450–459.
In the upper eyelid, the septum attaches to the levator aponeurosis, generally 2–5 mm above the superior edge of the tarsal plate.13 However, this septal-levator attachment can vary from the level of the superior tarsal border to almost 10 mm above. Below this level there is a blending of the connective tissue lamellae from both the septum and the levator aponeurosis called the pretarsal extension of the levator or the conjoined fascia.14 This fascia continues inferiorly to attach to the lower third of the anterior surface of the tarsal plate and sends fibrous slips forward to invest fascicles of the pretarsal orbicularis. In the lower lid, the septum similarly attaches to the capsulopalpebral fascia (which is the equivalent of the levator aponeurosis of the upper lid) below the inferior edge of the tarsus. This line of fusion between the two structures occurs in an oblique direction approximately 5 mm from the tarsal plate medially and 10 mm from the plate laterally. It is usually visible on operative dissection as a thickened white line in the septum that expands out laterally as it attaches to the inferolateral orbital rim by a triangular fascial band known as the arcuate expansion (Fig. 5-8). The lower lid septum can therefore be considered as being divided into an upper part, reinforced by the capsulopalpebral fascia on its deep surface, and a lower unsupported part.15 Orbital fat distension and bulging of this relatively weak lower septum orbitale results in the characteristic lower lid fat bags of aging.
The septum attaches medially to the spine at the lower end of the anterior lacrimal crest, called the lacrimal tubercle. It then extends from the lower eyelid to the upper eyelid medially by passing behind the attachments of the medial orbicularis at the posterior lacrimal crest. Superomedially the arcus marginalis forms the inferior portion of the supraorbital groove and laterally it blends with the lateral canthal raphe.16
Eyelid fat
The fat of the eyelid consists of preseptal (extraorbital) and postseptal (intraorbital) components.
The preseptal fat occurs mainly outside the orbital rim on the lower lateral brow and upper malar areas. Superiorly, this fat is positioned deep to orbicularis and frontalis, extending over the brow onto the surface of the adjacent septum orbitale of the upper lid. This ‘brow fat pad of Charpy’ has more recently been termed the retro-orbicularis oculi fat (ROOF)17 and the lid part as the preseptal fat pad. It can be up to 6 mm thick as it passes over the rim, tapering as it descends toward the lid margin to terminate where the fibers of the septum orbitale fuse with the fascia on the undersurface of orbicularis just millimeters above the supratarsal crease. Aesthetically, the ROOF provides fullness and projection for the brow and the preseptal component contributes to the supratarsal fold fullness. The equivalent layer inferiorly is the sub-orbicularis oculi fat (SOOF), which differs in being thinner and it usually does not cross the orbital margin into the lid. The SOOF is discussed in the midcheek anatomy section.
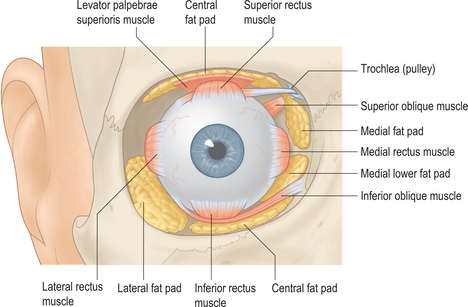
The postseptal fat is conventionally divided into compartments: two (medial and central fat pads) in the upper lid and three (medial, central and lateral fat pads) in the lower lid (Fig. 5-9). These compartments are made up of fat extensions from the adipose body of the orbit except for the upper lid central fat pad, which is separate preaponeurotic fat. The two types of fat differ in their color and consistency, however all the fat is linked by interconnecting septa that transgress the intrinsic muscle cone. Hence traction on fat just posterior to the septum orbitale can produce forces in the posterior extraconal and even intraconal and perioptic nerve region.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree