Chapter 43 Exfoliative diseases of the integument and soft tissue necrotizing infections
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
![]() IN THIS CHAPTER
IN THIS CHAPTER ![]() PowerPoint Presentation Online
PowerPoint Presentation Online
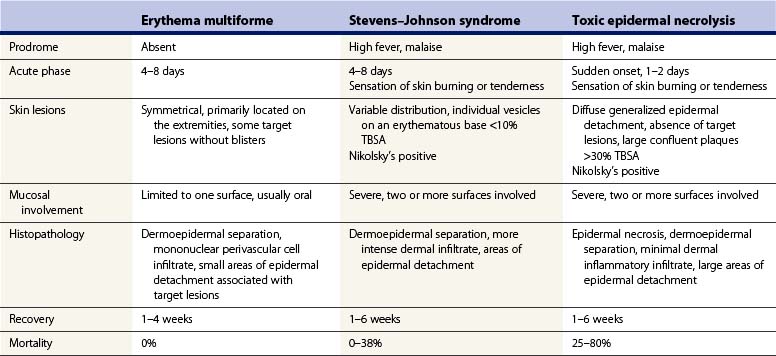
Severe exfoliative disorders
Erythema multiforme minor (EM), Stevens–Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN) are severe exfoliative diseases of skin and mucous membranes. There is great controversy on the classification of these exfoliative skin disorders and the terminology is confusing. Erythema multiforme minor is characterized by skin lesions isolated to no more than one mucosal surface. Erythema multiforme major involves two or more mucous membranes and may affect internal organs with systemic symptoms. However, most authors consider erythema multiforme major, SJS, and TEN to be the same disease entity, differing only by the area of involved skin. In this classification, SJS is considered to affect <10% total body surface area (TBSA), whereas TEN covers >30% TSBA, leaving a zone of overlap between 10% and 30% TBSA, which is referred to as SJS/TEN.1,2 The most common characteristics of these disease entities are defined in Table 43.1.3,4 The incidence of TEN is estimated at 0.4–1.2 cases per million persons per year. The incidence of SJS has been reported to be 1–7 cases per million persons per year.5–9 These exfoliative disorders occur in all age groups; however, the incidence is increased in the elderly and females.3,10–13 In addition, TEN is seen more often in patients with HIV infection14 and in bone marrow transplant recipients.15 Mortality of TEN ranges from 25 to 80%. However, reports are variable and usually based only on small patient populations.16–18 Death may occur early in the course of the disease, with sepsis being the most frequent cause. Pseudomonas aeruginosa and Staphylococcus aureus are the predominant organisms involved.16 Pulmonary embolism and gastrointestinal hemorrhage are other causes of death.10,16 The prognosis of SJS/TEN is worse than that of a burn victim with the same extent of skin loss.16 Mortality is increased significantly in those patients at the extremes of age, and in relation to the percentage of denuded skin and serum urea nitrogen levels.16,19 Cartotto et al. created a scoring system (SCORTEN) to predict mortality in the first 20 hours of individuals presenting with TEN.20 The scoring system evaluates seven parameters at presentation but recently has been challenged as to its true accuracy. SJS is associated with a mortality rate of 0–38%.11,20 Erythema multiforme rarely causes death.21
Etiology
TEN and SJS both appear to be caused by immunological reactions to foreign antigens. TEN, as the more severe entity, has a much higher percentage associated with antecedent drug therapy. Drugs are implicated in 77–94% of cases of TEN.6,22 Antibacterials and antifungals (36%), anticonvulsants (24%), analgesics and non-steroidal anti-inflammatory agents (38%), and even corticosteroids (14%) have been implicated.22,23 Attempts to identify drugs suspected of having caused exfoliative necrolysis by skin test and laboratory tests seldom have been rewarding.16 Upper respiratory tract infections, pharyngitis, otitis media, or viral illness are frequently reported.10–12,24–26 Mycoplasma pneumoniae and herpes viruses (cytomegalovirus, Epstein–Barr virus, herpes simplex, and varicella zoster) have been implicated in the cause of EM and SJS, but not TEN.11,27,28 It can be difficult to differentiate some prodromal symptoms as due to viral or other infectious agents, or due to the primary disease process. Recently, the incidence of HIV infection in patients with toxic epidermal necrolysis has risen.14,29 Whether this increase is due to their immunocompromised state or to the increased prescription of high-risk drugs, particularly sulfonamides, is debated. No history of drug ingestion or preceding illness may be noted in these patients. Many of these cases may actually suffer from lack of patient recall of current medication because of the severity of the underlying disease or the patient’s age. Idiopathic cases, not related to drugs, accounted for only 3–4% of TEN.6,7
Morphology/histopathology
An early skin biopsy is essential for diagnosis. Skin manifestations vary from patient to patient and with the age of the lesion (Fig. 43.1). Skin lesions may evolve to different stages of development with recurrent attacks of EM in a single patient.30 Advancing edges of the target lesions show scattered necrotic keratinocytes in the epidermis and only mild dermal inflammation. In older lesions and central zones of target lesions, the dusky appearance corresponds to areas of extensive keratinocyte necrosis, often with the formation of subepidermal bullae and dermoepidermal separation. The surrounding erythematous zone shows papillary dermal edema, vascular dilation with endothelial cell swelling, and perivascular mononuclear cell infiltrate.13 Extravasated erythrocytes may be seen in the surrounding papillary dermis. The reticular dermis is normal.

Figure 43.1 Toxic epidermal necrolysis (TEN) is characterized by massive sloughing of the epidermal tissue.
Epidermal and dermoepidermal suppressor/cytotoxic T-lymphocytes in addition to dermal infiltrates of helper T-lymphocytes have been demonstrated.31–33 Hertl has confirmed that these epidermal cells are cytotoxic T-cells.34 Langerhans cells appear to be reduced in the epidermis, although numerous dermal macrophages are observed.35 A more intense dermal cell infiltrate is present in SJS, especially in postherpetic cases.27,31 Dendritic lymphoid cells are observed, opposed to damaged dermal macrophages and necrotic keratinocytes. Further, at the point where the cytoplasmic processes contact the keratinocyte, the plasma membrane of the keratinocyte is absent.35 Aberrant expression of HLA-DR on keratinocytes has been observed, a phenomenon which has been observed in many other inflammatory skin disorders.32,36
Immunofluorescence microscopy has demonstrated IgM and C3 along the dermoepidermal junction and dermal vessels in cases of postherpetic SJS and EM.27,31 There have been only two reports of basal cell immunofluorescence in TEN.35,37 The pathogenesis of TEN is not completely understood. Type IV delayed hypersensitivity reaction, type II cytotoxic reaction, keratinocyte cytotoxicity mediated by lymphocytes, drug-related non-immunological mechanisms, and keratinocyte apoptosis mediated by receptors of the TNF superfamily are possible mechanisms which amplify predisposing factors of infection and genetic susceptibility.14,38–40 Positive patch tests in patients with TEN have been used to support the delayed hypersensitivity hypothesis.33 This view is somewhat at odds with the fact that HIV patients display increased frequency of TEN.14,41
Suppression/cytotoxic T-cell infiltrates are observed in the epidermis in TEN33,35 and graft versus host disease.42 It is hypothesized that cytotoxic T-cells recognize drug metabolites which are complexed with the MHC-I molecule on the surface of keratinocytes, migrate into the epidermis, react with keratinocytes, and cause epidermal necrolysis. The occurrence of sicca syndromes in patients with TEN and graft versus host disease further supports the autoimmune theory.43 The observation of blebbing of the keratinocyte plasma membrane in TEN is considered a reliable morphological finding of cytotoxic T-lymphocyte cytolysis.35 Further, the observation that cyclophosphamide aids TEN patients supports this theory, as cyclophosphamide is known to inhibit cytotoxic T-lymphocyte activity.35 Type II cytotoxic reactions involve the binding of either IgG or IgM antibodies to a cell-bound antigen. The antigen–antibody complex then activates the complement cascade and results in the cell destruction. This mechanism is not generally supported since nuclear fragmentation, common to keratinocytes of toxic epidermal necrolysis patients, is not a consequence of complement-mediated cytolysis.35,37,44 Keratinocyte apoptosis as the primary mechanism in the pathogenesis of TEN has been favored recently.39 This event is thought to be mediated by ligand/receptor interaction of the tumor necrosis factor (TNF) superfamily (as TNFα/TNF receptor or FasL/Fas interaction).39,45 In SJS, keratinocyte DNA fragmentation has been found in about 90% of cases associated with dermal perforin-positive lymphocytes.40 Non-immunological mechanisms include keratinocyte injury by either drug, drug metabolite, or toxic products derived from a drug in the epidermis.14,29,46
Clinical features
A prodromal phase of TEN/SJS is identified frequently and usually consists of low-grade fever, malaise, and cough, all of which may suggest a respiratory tract infection. These symptoms may precede any cutaneous manifestation by 1–21 days, but usually last for 2–3 days.2,11 Additionally, patients may present with conjunctivitis, sore throat, and generalized, tender erythema. This may evolve from morbilliform eruptions or discrete erythematous or purpuric macules.38 Later, vesicles and large bullae emerge from areas of erythema. Patients may exhibit diffuse red erythema immediately followed by epidermolysis.16 On light digital pressure, the epidermis desquamates in sheets: Nikolsky’s sign is positive (Fig. 43.2). Generally, a lag period of 1–3 weeks is observed from initiation of drug until skin eruption, which may be shorter on reexposure of a previously sensitized individual.1,2
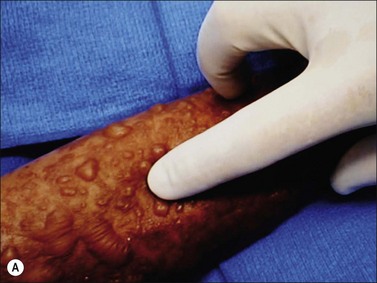


Figure 43.2 (a–c) Nikolsky’s sign. Epidermal separation induced by gentle pressure on the skin surface.
Two or more areas of mucosa involvement are typical of SJS or TEN. Mucosal involvement precedes skin lesions by 1–3 days in one-third of cases.13,47 Several sites are usually affected, in the following order of frequency: oropharynx, ocular, genitalia, and anus. Most TEN patients have multiple mucosal lesions, and they generally persist longer than cutaneous lesions.16
Complications
Toxic epidermal necrolysis is frequently associated with serious complications. The skin re-epithelializes from the dermal elements without scarring. Some patients experience hemodynamic instability and shock, and secondary full-thickness necrosis of the skin may develop; however, abnormal pigmentation is common. Nail plates are frequently lost and nail regrowth may be abnormal or absent.13 Mucosal membrane erosions may result in cicatricial lesions causing phimosis in men and vaginal synechiae in women. Oropharyngeal involvement is common and often results in severe dysphagia (Fig. 43.3).48 Although mucocutaneous erosions are the most common features of TEN/SJS, the disease may present with multisystem involvement. The onset of intestinal symptoms generally occurs concurrently with the cutaneous lesions.49 Epidermal and epithelial sloughing may extend into the gastrointestinal mucosa, and may induce esophagitis with frequent subsequent stricture formation.46 Gastrointestinal erosions macroscopically resemble ulcerative or pseudomembranous colitis and massive hemorrhage requiring resection has been reported.10,16,24 Intestinal involvement worsens the prognosis.16,49 Respiratory tract involvement occurs and is associated with increased mortality.48,50 These complications include diffuse erythema to extensive confluent tracheal and bronchial erosion covered by fibrinous exudate.38,48 Epiglottal swelling, necessitating intubation, has been reported.48 Desquamation of alveolar lining cells also has been reported and these patients require frequent tracheobronchial toilet.49 Subclinical interstitial edema is often noticed and 30% of cases progress to frank pulmonary edema and respiratory decompensation.13,51 Bronchopneumonia was found to be the most frequent complication, occurring in 50% of patients.21,24,50 Pulmonary embolism is an important cause of death in patients with TEN.16 Renal manifestations like glomerulonephritis and acute tubular necrosis,52 as well as hepatitis and hepatocellular necrosis, have been described.13,38 Hypoalbuminemia, asymptomatic hyperamylasemia, increased erythrocyte sedimentation rate, leukocytosis, thrombocytopenia, and normochromic and normocytic anemia are not uncommon.21,48 Leukopenia is a frequent and poor prognostic sign.12,13,16,24 This is due, in part, to depletion of the T-helper/inducer lymphocyte population (CD4+).53 Ocular sequelae are the most severe long-term complications and occur in half of the survivors. Pseudomembranous or membranous conjunctivitis resulting from coalesced fibrin and necrotic debris can lead to opacification, secondary infection, and blindness (Fig. 43.4).4 Conjunctival scarring may result in lacrimal duct destruction, leading to reduced tear production and keratoconjunctivitis sicca, a Sjögren-like syndrome. Ectropion, entropion, trichiasis, and symblepharon can also occur.11,43
Management
Toxic epidermal necrolysis is a life-threatening disease. Such a patient is best managed in a burn intensive care unit where goal-directed fluid resuscitation, nutritional support, wound care, physical therapy, and social services are provided routinely utilizing a multidisciplinary approach.10,12,17,18,24,25,38
Surgical approach
Debridement of necrotic epidermis and coverage of the large wound surface with biological or synthetic dressings are essential.10,54–56 Sloughed epidermis should be removed in order to reduce bacterial growth and the risk for infection. The exposed and tender dermis should be covered. Debridement is best undertaken under general anesthesia as soon as diagnosis by histology is established. Blood loss associated with debridement is minimal, so over-resuscitation must be avoided. Synthetic dressings, such as Biobrane™, and biological dressings, such as homograft (cadaver allograft) and porcine xenograft skin, greatly reduce the pain, decrease fluid loss, promote healing, and reduce the risk of wound infection and sepsis.10,54–57 Biobrane™ is readily available as a commercial shelf product; however, in our own experience it is associated with increased local infection when covering greater than 40% TBSA wound areas. Porcine xenograft adheres well to the skin and is commercially available in large quantities.55,56 Homograft is more likely to become vascularized and therefore reduces the number of graft changes.10,58 However, this must be weighed against the potential poor cosmetic results of vascularized homograft (Fig. 43.5). Grafted areas must be immobilized and protected from shear forces. In children, Steinmann pins to suspend extremities may be useful.55 In both adults and children, continuous rotation or air fluidized (Clinitron) beds frequently are used.
Topical therapy
As separation occurs at the dermal–epidermal junction, varying depths of viable dermis remain. If this dermis can be protected from toxic detergents, desiccation, mechanical trauma, and wound infection, then rapid re-epithelialization by proliferation of basal keratinocytes from the skin appendages will occur.54 However, bacterial proliferation on the unprotected wound surface with invasive infection leads to full-thickness skin necrosis. Hydrotherapy and topical antimicrobials provide debridement and infection control which should be initiated early in the course of the disease.11,26 Effective topical antimicrobial agents include silver sulfadiazine cream,30 silver nitrate solution,13,24,26 chlorhexidine gluconate solution,13 and polymyxin-bacitracin ointment.11 Silver sulfadiazine is widely used but may exacerbate the disease process due to its sulfonamide component. Additionally, an inhibitory effect on epithelialization and leukopenia requiring discontinuation has been observed. Silver nitrate solution does not contribute to the ongoing drug reaction, and epithelialization is not inhibited. However, silver nitrate solutions are hyponatremic, and thus associated with approximately 350 mmol of sodium loss per day/m2 treated. Therefore, serum electrolytes and osmolarity must be carefully monitored. For patients with contaminated wounds due to delayed initiation of treatment, silver nitrate soaks can reduce contamination and prepare the wound for eventual biological dressing. Chlorhexidine gluconate and polymyxin ointment are effective against Gram-negative organisms, including P. aeruginosa, with low incidence of sensitivity. Moreover, chlorhexidine gluconate also shows bactericidal effects against Gram-positive organisms.
Immunomodulation therapy
Corticosteroid therapy
Corticosteroid treatment of toxic epidermal necrolysis has produced much controversy. In regard to the delayed hypersensitivity reaction or antibody-dependent cytotoxicity theories of pathogenesis, corticosteroids would seem to be an appropriate form of medical therapy.38,59 However, the practice of administering continuous high-dose corticosteroid in an attempt to stop the progression of the disease is widely rejected.11–13,38,42,46,60,61 Rational assessment of the benefit of corticosteroids administration is not possible due to the lack of randomized, controlled, prospective trials. Many authors feel that steroids enhance the risk of sepsis,24,55 increase protein catabolism, delay wound healing,16 cause severe gastrointestinal bleeding,16,24 prolong hospitalization,61 and increase mortality.12,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree