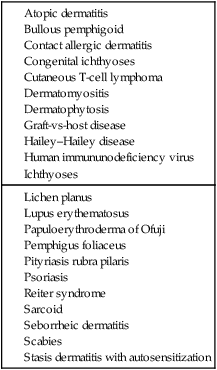
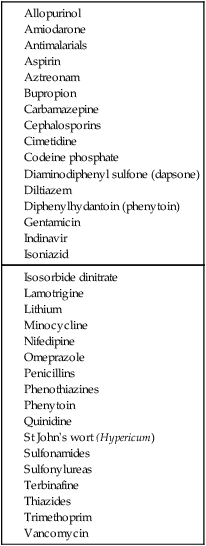
Erythroderma (exfoliative dermatitis) is defined as inflammation of at least 90% of the body surface, characterized by generalized erythema and a variable degree of scaling or desquamation. Erythroderma is commonly the result of generalization of a pre-existing chronic dermatosis or a systemic disease (see Table 75.1). These include genodermatoses and congenital disorders such as severe ichthyoses and ichthyosiform erythrodermas; severe cases of dermatoses such as psoriasis, atopic or seborrheic or contact allergic dermatitis; cutaneous T-cell lymphoma; allergic reactions to drugs (see Table 75.2); and internal malignancies (especially lymphoma and other lymphoreticular malignancies). Some cases develop without any apparent trigger and erythroderma remains ‘idiopathic’ in up to 25% of the cases.
Erythroderma

Specific investigations
Survival outcomes and prognostic factors in mycosis fungoides/Sézary syndrome: validation of the revised International Society for Cutaneous Lymphomas/European Organisation for Research and Treatment of Cancer staging proposal.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree