Fig. 12.1
Large flaps would include the perforators anyway. On the other hand, it is difficult to design small flaps
The classic approach was to confirm the design after making a long incision and locating the perforator, or to harvest a large flap and trim it afterwards. By providing added information about the exact location of the perforator, endoscopes make it possible to avoid extra skin incision or extra tissue harvesting (Fig. 12.2).
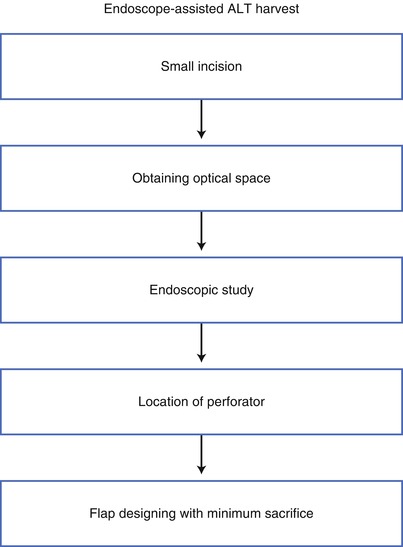
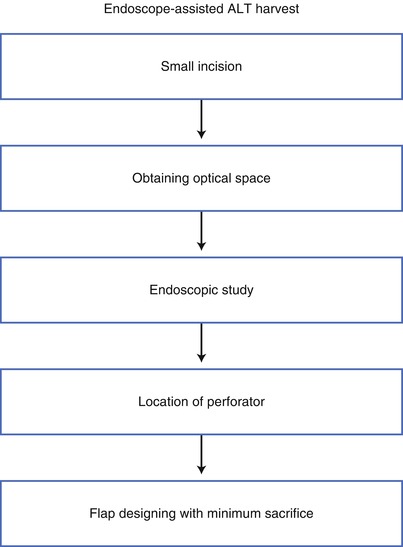
Fig. 12.2
Steps of harvesting anterolateral thigh (ALT) flaps using an endoscope. By obtaining information about the exact location of the perforator, the endoscope makes it possible to avoid extra skin incision or extra tissue harvesting
12.1 Training
Handling of endoscopes requires some training, for which we recommend using suitable animal models. Perforator flaps of pigs are a preferable animal model, considering their size and the structure of the subcutaneous tissue. For the example shown in Fig. 12.3, a female Yorkshire pig weighing 35 kg was used at our Animal Laboratory in compliance with the Guide for the Care and Use of Laboratory Animals for Institutions of the Governing Agency published by the Japanese Ministry of Health, Labor and Welfare. A 2-cm skin incision is first made in the thigh of the pig, and the cavity for the endoscopic camera is made using manual retractors.


Fig. 12.3
An incision (2 cm in length) made in the thigh of a pig for endoscopic training
Then a standard 10-mm, 0°-angle endoscopic camera is put into the subcutaneous layer (Fig. 12.4).
Fig. 12.4
Two retractors are inserted to obtain optic space. A standard 10-mm, 0°-angle endoscopic camera is put into the subcutaneous layer
Standard surgical endoscopic instruments such as scissors, dissectors, and monopole coagulators are used to dissect the subcutaneous layer and to cut the tissue surrounding the perforator (Fig. 12.5).
Fig. 12.5
Standard surgical endoscopic instruments, including scissors, dissectors, and monopole coagulators
The subcutaneous tissue is loose, so dissectors are applied first to make this layer honeycomb-like (Fig. 12.6); then scissors are used to cut the remaining fibrous tissue (Fig. 12.7).
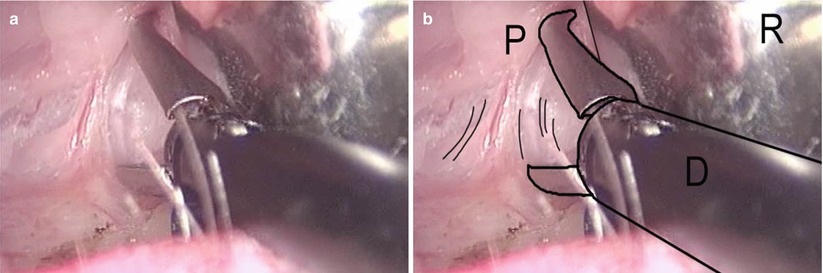
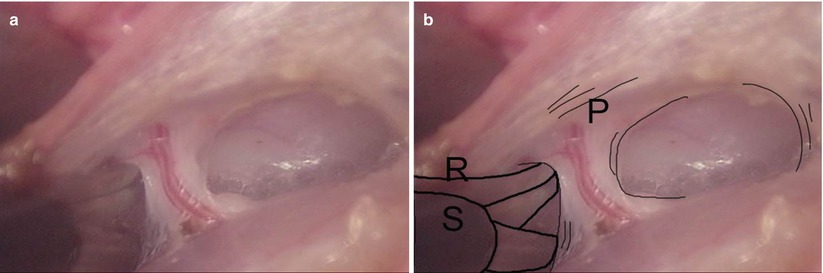
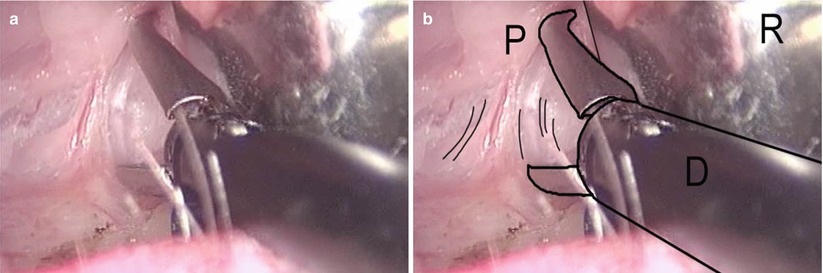
Fig. 12.6
(a, b) The loose subcutaneous tissue is first dissected to become honeycomb-like. D dissector, R retractor, P perforator
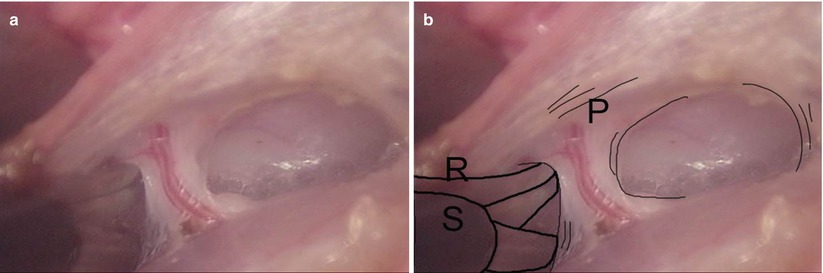
Fig. 12.7
(a, b) Scissors cutting the remaining fibrous tissue. P perforator, R retractor, S scissors
Tissues including vessels are coagulated by monopole diathermy. An aspirator at the incision helps to clear the misty view. Though the skin incision is short, the surgeon and the assistants can see everything more closely and much more clearly because the lens of the camera has a wide angle and high magnification, so it is not difficult to find the perforator in the subcutaneous tissue. After detecting the perforator and marking its location, the flap is designed and the skin incision is performed to harvest the flap (Figs. 12.8, 12.9, and 12.10).
Fig. 12.8
After the location of the perforator has been confirmed, the flap is designed
Fig. 12.9
Endoscopic dissection can isolate the perforator
Fig. 12.10
The perforator flap is harvested
12.2 Surgical Technique
After a brief survey of the perforators with a hand-held Doppler, a 2-cm skin incision is made at the anterior aspect of the thigh (Fig. 12.11).
Fig. 12.11
Skin incision to the lateral aspect of the thigh
This incision can be made either medial or lateral to the line through the anterior superior iliac spine and the lateral margin of the patella, but the lateral approach does not require the procedure to cross the septum to find the musculocutaneous perforators arising from the vastus lateralis (Fig. 12.12).
Fig. 12.12
Schema of endoscopic harvesting of an ALT flap
Subcutaneous tissue is dissected with two retractors to the femoral fascia. An incision is made through the fascia, and the edges of the fascia are clamped by a Kocher or mosquito clamp (Fig. 12.13).
Fig. 12.13
After dissection of the subcutaneous tissue with two retractors, the femoral fascia is incised and the edge is clamped by Kocher or mosquito clamps
After dissection of the subfascial layer under direct vision, one retractor is inserted to pull up the fascia and one to push down the rectus femoralis or the lateral vastus muscle to obtain an optical cavity (Fig. 12.14).
Fig. 12.14
One retractor is inserted to pull up the fascia to obtain an optical cavity
A 3-mm, 0°-angle endoscopic camera (Fig. 12.15) is inserted into this working space, and microdissecting forceps are placed to perform subfascial dissection.
Fig. 12.15
A 3-mm, 0°-angle endoscopic camera
The procedure is performed under endoscopy, which enables the surgeons to find even the smallest perforators with large magnification. The video monitor also allows the assistants to have the same view as the surgeons (Fig. 12.16).


Fig. 12.16
The video provides both the surgeon and the assistants with a wide-angle, high-magnification view
Though the subfascial tissue is loose, the first view would look like Fig. 12.17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree