Fig. 10.1
A well-padded pneumatic tourniquet is placed on the upper arm and is typically inflated to 250 mmHg. The remainder of the arm is prepped and draped in standard fashion
10.8.2 Landmarks
Figure 10.2 illustrates typical preoperative marking of the arm.


Fig. 10.2
The medial epicondyle of the arm is marked, as is the tip of the olecranon on the medial aspect. With the arm held in 45–60° of flexion, the usual course of the ulnar nerve is drawn; it can typically be palpated under the skin. If the ulnar nerve subluxes, the arm is held with the nerve in a reduced position, typically in 45° of flexion. The incision is drawn, extending from just proximal to the medial epicondyle to 2 cm distal. This incision is located slightly anterior to the course of the ulnar nerve
10.8.3 Procedure
The skin incision is made with a #15 blade and continued, raising full-thickness anterior and posterior flaps toward the medial epicondyle. Care is taken to identify crossing venous structures; hemostasis is maintained with electrocautery. A branch of the medial antebrachial cutaneous nerve may be identified, but it is not typically encountered.
Figures 10.3, 10.4, 10.5, 10.6, 10.7, 10.8, 10.9, 10.10, 10.11, and 10.12 illustrate the rest of the procedure.
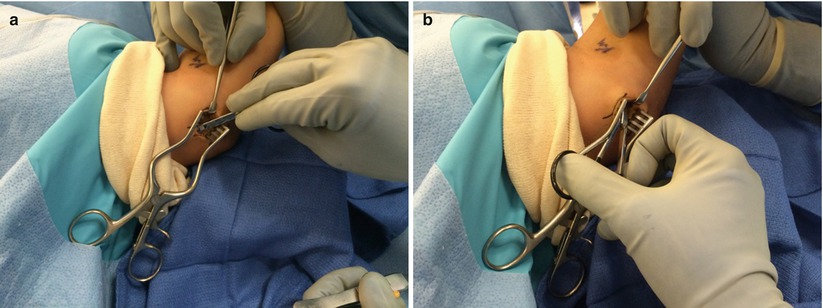

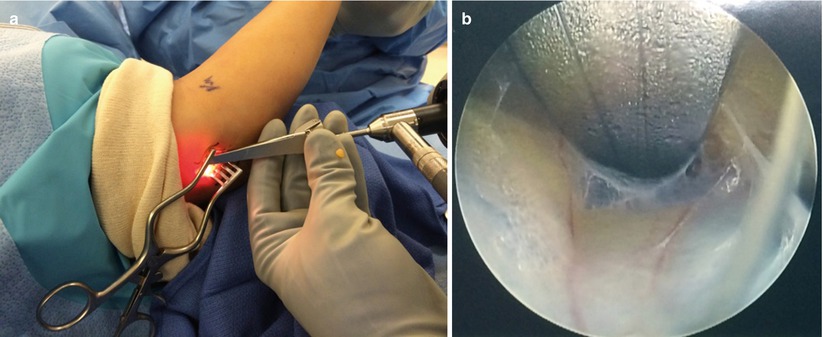
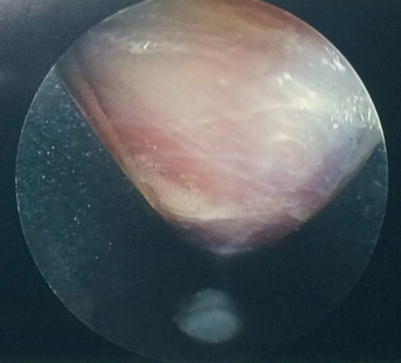
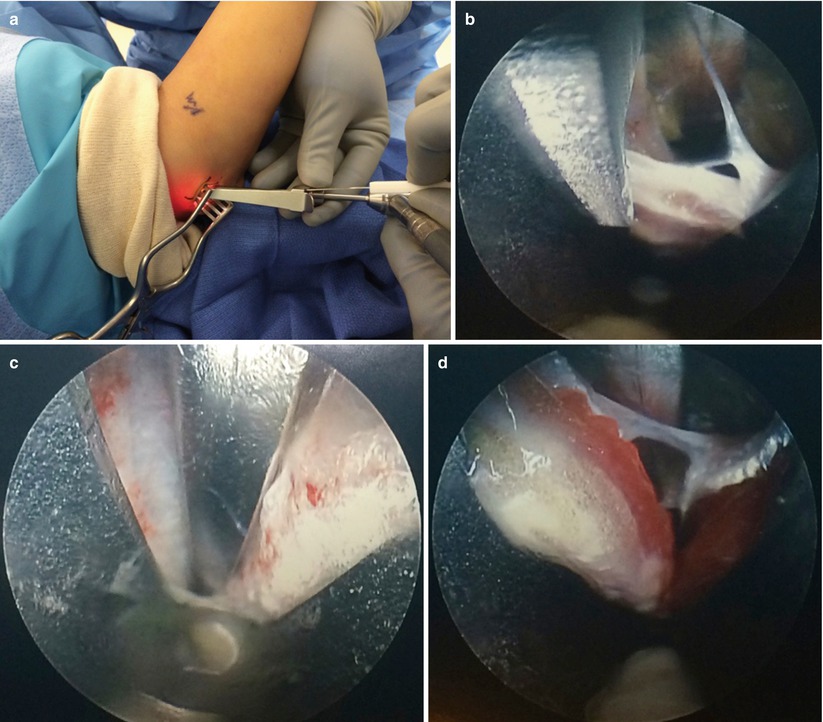
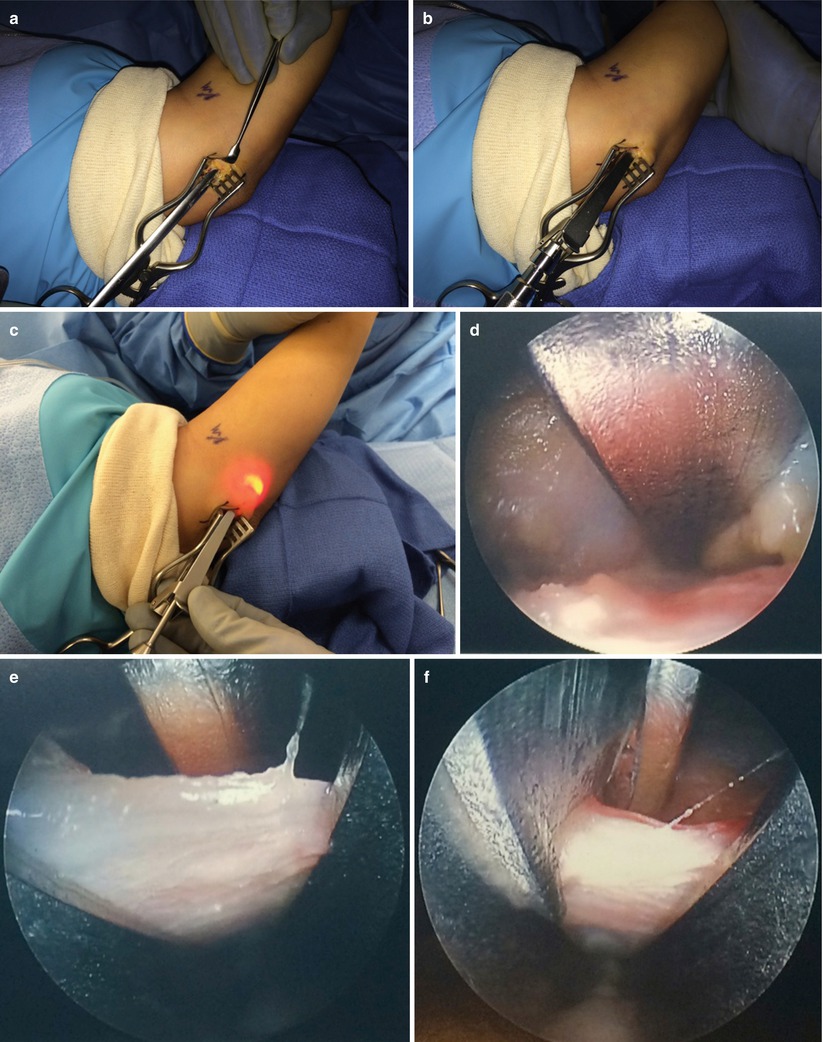
Fig. 10.3
The fascia overlying the flexor carpi ulnaris (FCU) muscle is identified at the distal extent of the incision and marks the depth of the dissection. The fascia of Osborne’s ligament is divided over the cubital tunnel by removing it from the posterior aspect of the medial epicondyle until the ulnar nerve is identified
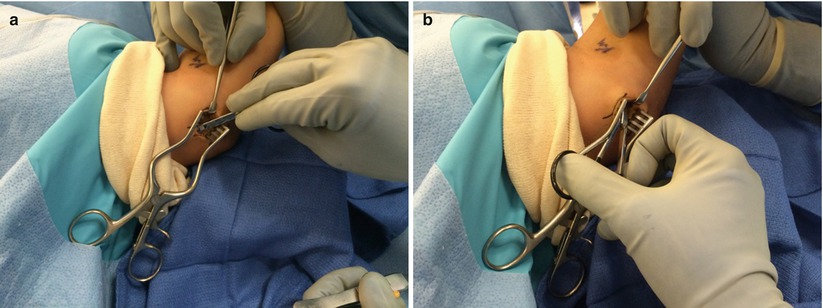
Fig. 10.4
(a, b) A blunt tenotomy scissors is used to develop a pocket superficial to the fascia and Osborne’s ligament both proximally and distally. Any venous structures identified are either retracted or coagulated. Proximally, the ulnar nerve can often be visualized emerging from the arcade of Struthers; distally, it passes deep to the fascia of the FCU
Fig. 10.5
Proximally, a blunt-tipped dissector is inserted deep to the fascia, creating a pocket for the trocar and camera

Fig. 10.6
The trocar is inserted deep to the fascia and superficial to the ulnar nerve. Slots within the posterior cannula should be aligned along the course of the ulnar nerve to ensure maximal nerve protection. The metal soft-tissue protection sleeve should be superficial to the fascia but deep to the subcutaneous tissues
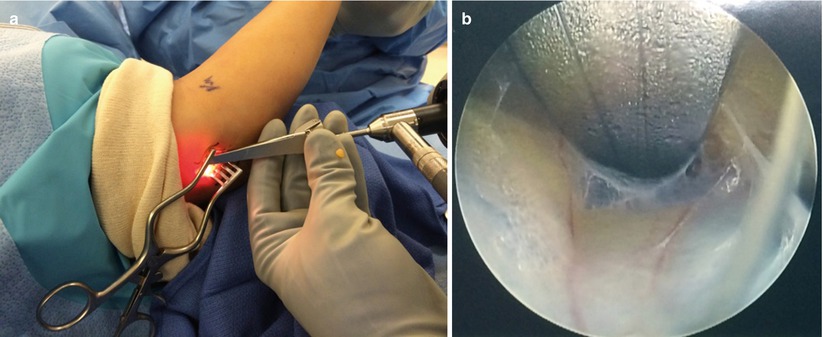
Fig. 10.7
(a, b) The camera is inserted between the fascia and the protection sleeve to verify that no aberrant nerve or vascular structures are present within the path of the intended nerve release. The camera is inserted into the trocar sleeve
Fig. 10.8
The ulnar nerve is visualized through the posterior slots of the cannula, and the trocar is rotated to ensure that the ulnar nerve is safely protected along its entire course
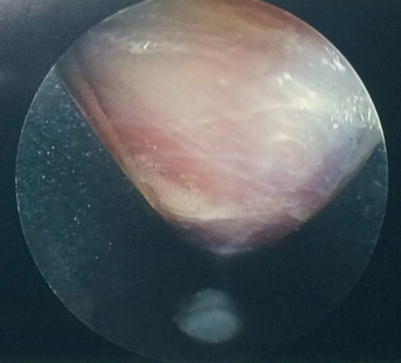
Fig. 10.9
The camera should be rotated to visualize the undersurface of the fascia, ensuring that nerve or vascular structures are not trapped between the trocar and the fascia
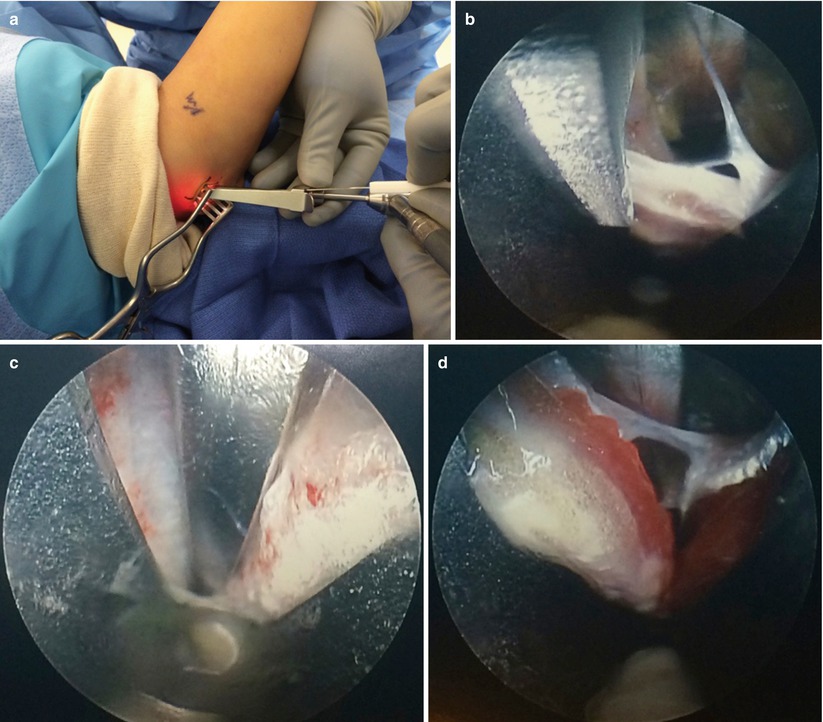
Fig. 10.10
(a–d) Under direct visualization, an antegrade cutting knife is inserted through the cutting slot and is used to divide the fascia. The knife, camera, and cannula are removed and the area is inspected to ensure that the fascia has been divided and no injury to the ulnar nerve has occurred
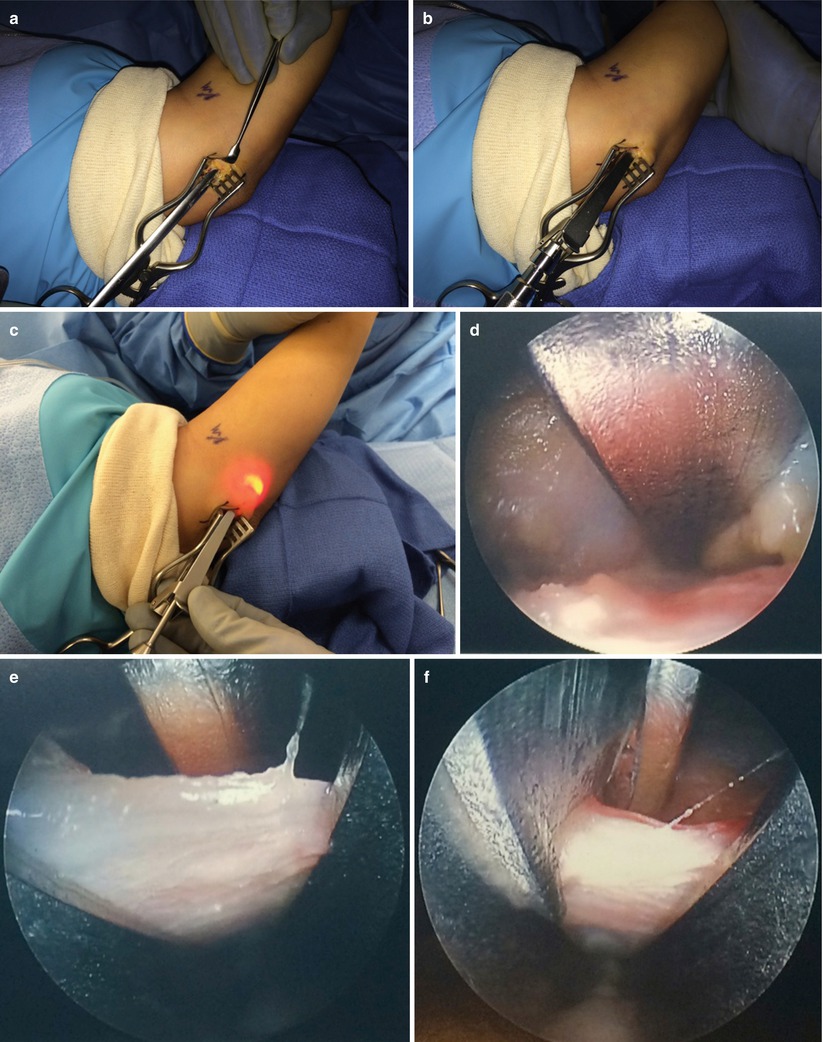
Fig. 10.11
(a–f) The procedure is replicated in the distal direction, ensuring that the ulnar nerve is released to the level of the motor branch to the FCU muscle
Fig. 10.12
After release proximally and distally, the elbow is brought through a full arc of motion from extension to flexion while the ulnar nerve is monitored for subluxation; if the ulnar nerve subluxes, transposition of the nerve should be considered
At the end of the procedure, the tourniquet is deflated and hemostasis is obtained under direct visualization with pressure and electrocautery. The wounds are copiously irrigated with a normal saline solution and closed in a layered fashion. The area is injected with local anesthetic (such as 1 % lidocaine with 1:100,000 epinephrine) for postoperative pain control. The wounds are covered with a nonadherent gauze, sterile gauze, and a compressive overwrap.
10.8.4 Postoperative Care
The patient is given a prescription for pain medication as required. Nonsteroidal anti-inflammatory medications are typically avoided for the first 48–72 h to minimize postoperative hematoma formation. The patient is instructed to elevate the hand and elbow and apply ice for 30 min every 2 h for the first 24 h, except while sleeping. The patient may remove the dressings on postoperative day 2 and shower normally, patting the elbow dry, but the elbow should not be soaked in standing water such as a bathtub or swimming pool while the sutures are in place. Light activity is allowed when comfortable, but heavy activity should be avoided. The sutures are removed 10–14 days after surgery, when the incisions are healed. Activity is then progressed according to the tolerance of the patient.
References
1.
Feindel W, Stratford J. Cubital tunnel compression in tardy ulnar palsy. Can Med Assoc J. 1958;78:351–3.PubMedCentral




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








