Endoscopic Brow Lift
Robert Glasgold
Mark Glasgold
Endoscopic Brow Lift
Rejuvenation of the upper eye lid-orbital rim complex must incorporate techniques that will address hyperfunctional rhytids, brow ptosis, hooding of the upper lid, herniation of orbital fat, eyelid ptosis, and loss of facial volume. Although the focus of this chapter is on the role of the endoscopic brow lift, all of these issues are important in the evaluation of aging of the upper third of the face.
The rejuvenating effect of an endoscopic brow lift is accomplished by repositioning the brow over the orbital rim and softening the hyperfunctional glabella and forehead lines resulting from chronic muscle contracture. The endoscopic brow lift is performed through small, well-hidden incisions placed behind the hairline. This technique relies on adequate undermining of the forehead and scalp to allow appropriate mobilization following release of the brow depressors by performing myotomies of the orbicularis oculi, corrugator supercilii, and procerus muscles. The lift is completed with a variety of fixation techniques to maintain the new brow position. In our experience, the endoscopic approach produces a more natural appearing result than alternative “open” techniques that utilize skin tension in their elevation. The endoscopic approach minimizes the associated alopecia and numbness resulting from the larger incisions of the coronal and pretrichial approaches. We have exclusively used an endoscopic approach with conscious sedation anesthesia for the past 7 years, with high levels of patient satisfaction.
Brow Aesthetics
An understanding of the ideal brow position is important for identifying patients who are appropriate candidates for brow lifting. Ideally, the face is divided into equal thirds, with the upper third extending from the brow to the hairline. The brow should sit at the level of the orbital rim. The male brow tends to be more horizontally
oriented, whereas the female brow tends to arch along its course over the orbital rim (1,2). There is tremendous variation in eyebrow shape and length. Most women and some men will have groomed their eyebrows to what they feel is the most aesthetically pleasing shape for their faces.
oriented, whereas the female brow tends to arch along its course over the orbital rim (1,2). There is tremendous variation in eyebrow shape and length. Most women and some men will have groomed their eyebrows to what they feel is the most aesthetically pleasing shape for their faces.
The aging process results in crowding of the orbital complex due to a brow position below the orbital rim and loss of the upper lid crease. The upper third of the face is lengthened. Brow ptosis often is accentuated by a volume loss in the forehead and temple leading to a hollowed orbit and gaunt appearance to the upper orbital rim. The loss of subcutaneous fat may be evident in patients as early as their mid to late 30s. In the patient who chronically frowns, the medial brow is pulled inferiorly and more medially, adding to a stern appearance.
Preoperative Evaluation
Patients who are candidates for brow lift will generally complain of a tired or stern appearance. They may be bothered by a feeling of heaviness on their eyes. The patient evaluation begins during the initial conversation, at which time it is important to evaluate the face as it appears during dynamic expressions. The neutral brow position then is evaluated in a relaxed state. This can be accomplished by having the patient close his/her eyes and relax the brow, and then slowly open the eyes. The neutral brow position is assessed relative to the orbital rim.
It is important to identify if the patient chronically maintains the brow in an elevated position. These patients with a pseudoelevated brow due to chronic frontalis contraction likely will be unaware of this habit. Some patients with chronic frontalis contraction will reflexively relax after a brow lift. Conversely, other patients will require a period of treatment with botulinum toxin type A (Botox) to break this subconscious habit. This issue should be addressed preoperatively so that patients are not surprised by the need for at least a limited series of Botox injections postoperatively. The use of photographic images is invaluable in helping patients understand these issues by allowing them to view their face in both a dynamic and a relaxed state. The images also are helpful for pointing out the presence of subtle asymmetries preoperatively and making patients aware that these often will not be corrected. In our experience, computer imaging of a projected result of a brow lift has been unsatisfactory, and we do not recommend using it for this purpose.
Within the category of patients with a pseudoelevated brow is a group of patients with undiagnosed upper lid ptosis. These patients may chronically contract their frontalis muscle to compensate for their ptosis. Identifying these patients will help avoid having a dissatisfied patient postoperatively who still complains of a heaviness of the upper lid due to untreated ptosis. If a brow lift is performed without a ptosis repair, these patients likely will have, and complain of, persistent horizontal forehead rhytids secondary to chronic frontalis contraction. If it were to go unrecognized postoperatively and the forehead was treated with Botox to break this habit, the patient will have an exaggeration of their upper lid ptosis. We refer all patients with upper lid ptosis for repair of their lid ptosis prior to considering brow lift.
Assessment of the patient’s hair, in terms of hairline, hair density, and hairstyle, is integral in selecting patients for brow lift. Hairline is a factor because some patients may be very concerned with maintaining their present hairline, whereas others may have a desire to either raise or lower their hairline. An endoscopic brow lift will cause a slight elevation in the patient’s hairline. The endoscopic approach will not allow for lowering of the hairline as with a pretrichial approach, nor will it allow for a significant elevation in the hairline as can be obtained with a coronal
approach. These issues must be clarified with the patient preoperatively so that his/her expectations are met. Hair density is a factor because some patients may not tolerate the periincisional alopecia that may occur with external screw suspension, although this is temporary in most cases. Hairstyle is a factor because some patients who have chronically pseudoelevated brows often wear bangs to hide the horizontal rhytides. If these patients plan to continue with this hairstyle, they may be well served with just an upper lid blepharoplasty even though their neutral brow position is severely ptotic.
approach. These issues must be clarified with the patient preoperatively so that his/her expectations are met. Hair density is a factor because some patients may not tolerate the periincisional alopecia that may occur with external screw suspension, although this is temporary in most cases. Hairstyle is a factor because some patients who have chronically pseudoelevated brows often wear bangs to hide the horizontal rhytides. If these patients plan to continue with this hairstyle, they may be well served with just an upper lid blepharoplasty even though their neutral brow position is severely ptotic.
A brow lift will change the facial proportions, opening up the middle third of the face. Brow ptosis develops as people age, with loosening of the soft tissue supports and loss of volume. In these patients, a brow lift will have the rejuvenating effect of returning them to the appearance of their youth. In contrast, some patients may have had a low brow for their entire life. Old photographs may be helpful in making this distinction. Patients with a congenitally low brow will view the effects of a brow lift not only as making their appearance more youthful, but also as a change in appearance.
The upper eyelid-orbital rim complex needs to be evaluated to determine whether aging in this region is a function of dermatochalasis, brow ptosis, or a combination of both. In patients with brow ptosis who have significant hooding, a combination of upper lid blepharoplasty and brow lift is recommended.
A final aspect of the patient evaluation is psychological. In order to ensure a satisfactory outcome, the patient should be realistic with regard to the expected result and the postoperative course. Some degree of numbness and paresthesia of the scalp lasting weeks and, in rarer instances, up to 1 year is to be expected. Many patients will not tolerate this and will be dissatisfied regardless of a good postoperative appearance. This information should be addressed through a detailed preoperative discussion with the patient and is particularly useful in the decision-making process for patients who would benefit from either a blepharoplasty or a brow lift.
Surgical Anatomy
Brow lifting requires an understanding of the muscular, neural, and vascular anatomy, and the anatomic planes of the forehead. It is imperative to understand which structures affect brow position in both a dynamic and a resting state.
Forehead Muscles
The forehead musculature can be broken down into two groups: the brow elevators and the brow depressors. The primary brow elevator is the frontalis muscle. The brow depressors are the corrugators, the depressor supercilii, the orbicularis oculi, and the procerus muscles. It is through release of the brow depressors and the resulting unopposed action of the brow elevator that much of the brow lift is accomplished.
The frontalis consists of a pair of muscles that originate from the forehead skin and superficial fascia of the orbicularis oculi muscle and insert posteriorly into the galea aponeurosis. Flexion of the frontalis results in elevation of the brow and secondarily creates horizontal folds in the forehead. The unopposed action of the frontalis muscle upon release of the brow depressors plays a significant role in elevating the brow. Innervation of the frontalis muscle is through the frontal branch of the facial nerve, which enters the muscle at its deep lateral aspect (3). During an endoscopic brow lift, the frontalis muscle is not directly visualized because it remains superficial to the plane of dissection.
The corrugator supercilii are a pair of muscles that originate from the superomedial orbit, deep to the procerus and depressor supercilii muscles, and run in a superolateral direction, inserting into the fascia of the frontalis, the orbicularis oculi muscle, and brow skin (3). Contraction of the corrugators moves the medial brow in an inferomedial direction. Knize (4) has shown that as the corrugators run superolaterally, they split into a transverse and an oblique head. He describes the transverse head as being innervated by the temporal branch of the facial nerve and the oblique branch being innervated by the zygomatic branch of the facial nerve. Contraction of the oblique fibers will depress the medial brow and cause oblique wrinkling of the glabellar skin. Contraction of the transverse fibers moves the eyebrow medially, resulting in vertical and oblique wrinkling of the glabellar skin (4).
The procerus muscle originates from the nasal bone and runs superiorly, inserting into the skin of the central lower forehead. Contraction of the procerus muscle pulls the medial brow inferiorly and results in transverse wrinkling of the central lower forehead and glabella. Innervation of the procerus muscle is via the temporal branch of the facial nerve.
The orbicularis oculi is a sphincter muscle consisting of three components: the orbital, the preseptal, and the pretarsal. The muscle originates from the medial orbital rim and medial canthal ligament, encircles the eye, and inserts on the inferomedial orbital rim (3). Contraction of the orbicularis oculi closes the eyelids and depresses the full extent of the brow. Innervation of the orbicularis oculi muscle is via the temporal and zygomatic branches of the facial nerve.
The depressor supercilii muscles originate from the superomedial orbital rim and insert into the skin of the medial brow. Contraction of the depressor supercilii muscle depresses the medial portion of the brow (4).
Sensory and Motor Nerves
Sensory innervation of the upper third of the face is supplied by branches of the ophthalmic and maxillary divisions of the trigeminal nerve. The motor nerve supplying the muscles of facial expression is the facial nerve. Endoscopic brow lifting requires an understanding of the anatomy of the supraorbital nerve, supratrochlear nerve, zygomaticotemporal and zygomaticofacial nerves, and temporal branch of the facial nerve.
The supraorbital nerve is a branch of the ophthalmic division of the trigeminal nerve. In 80% to 90% of people, it arises out of a notch at the roof of the orbit at the midpupillary point. In 10% to 20% of people, it may arise from a distinct supraorbital foramen 1 to 2 cm above the superior orbital rim (Fig. 4.6.1) (5,6). The supraorbital nerve courses immediately lateral to the corrugator muscle after exiting the notch and runs in the forehead superficial to the frontalis muscle. The supraorbital nerve supplies sensory innervation to the skin of the central upper lids, the forehead, and the scalp posteriorly to the vertex.
The supratrochlear nerve also is a branch of the ophthalmic division of the trigeminal nerve and arises medial to the supraorbital nerve. As it passes from a deeper to more superficial plane at the orbital rim, it runs medial to the corrugator muscle and runs superficial to the corrugator once it leaves the orbit. The supratrochlear nerve supplies sensory innervation to the skin of the medial upper eyelid, the central forehead, and the scalp posteriorly to the vertex.
The zygomaticotemporal and zygomaticofacial nerves are branches of the maxillary division of the trigeminal nerve. Collectively these nerves provide sensory innervation to the skin of the lateral upper lid and temporal region. A branch of the zygomaticotemporal nerve runs adjacent to the sentinel vein during endoscopic
dissection (7). Recognition and preservation of this nerve branch when cauterizing the sentinel vein can aid in reducing postoperative numbness.
dissection (7). Recognition and preservation of this nerve branch when cauterizing the sentinel vein can aid in reducing postoperative numbness.
 Figure 4.6.1. Intraoperative photograph demonstrating the supraorbital nerve exiting from the supraorbital foramen. |
The temporal branch of the facial nerve is the primary motor nerve that is of concern during brow lifting. The temporal branch leaves the parotid gland at its superior aspect, then crosses over the zygomatic arch midway between the lateral canthus and the anterior aspect of the auricle. The temporal branch passes over the zygomatic arch within the superficial temporal fascia (also known as the temporoparietal fascia). The nerve continues superiorly, running on the deep aspect of the frontalis muscle where it goes on to innervate the brow and forehead musculature. Understanding the relationship between the temporal branch and the sentinel vein is integral to preventing injury to the nerve. The sentinel vein will be encountered during dissection superior and lateral to the lateral canthus as it crosses from deep to the deep temporal fascia inferiorly into the superficial temporal fascia superiorly. The point where the sentinel vein enters the superficial layers corresponds with where the temporal branch of the facial nerve crosses. Consequently, if the vein is to be cauterized, it should be done at its deep aspect (7).
Anatomic Planes
The central forehead and the lateral forehead have distinct anatomic layers. The temporal line, marked by the superior edge of the insertion of the temporalis muscle, is the dividing line between the central and lateral forehead. From superficial to deep, the central forehead is composed of skin, subcutaneous fat, galea aponeurosis, loose areolar tissue, and periosteum. Anteriorly, the galea aponeurosis splits to surround the frontalis muscle. Toward the apex of the scalp, the galea runs as a single layer and then posteriorly splits again to surround the occipitalis muscle.
Lateral to the temporal line, the anatomic planes, from superficial to deep, include skin, subcutaneous fat, superficial temporal fascia, deep temporal fascia, and temporalis muscle. The superficial temporal fascia is continuous with the galea aponeurosis superiorly and the superficial musculoaponeurotic system inferiorly.
Running within the temporoparietal fascia are the superficial temporal artery and vein, and the temporal branch of the facial nerve once it crosses the zygomatic arch. The deep temporal fascia is a more dense fascial layer just superficial to the temporalis muscle. The deep temporal fascia splits into a superficial and a deep layer at two points. Initially located 2 to 3 cm above the zygomatic arch, it splits to encompass the temporal fat pad and then inferiorly splits again to encompass the zygomatic arch (3). Running within the deep temporal fascia are the middle and deep temporal vessels, which make up the vascular supply to the temporalis muscle.
Running within the temporoparietal fascia are the superficial temporal artery and vein, and the temporal branch of the facial nerve once it crosses the zygomatic arch. The deep temporal fascia is a more dense fascial layer just superficial to the temporalis muscle. The deep temporal fascia splits into a superficial and a deep layer at two points. Initially located 2 to 3 cm above the zygomatic arch, it splits to encompass the temporal fat pad and then inferiorly splits again to encompass the zygomatic arch (3). Running within the deep temporal fascia are the middle and deep temporal vessels, which make up the vascular supply to the temporalis muscle.
Surgical Technique
Routinely we perform endoscopic brow lifts under conscious sedation in conjunction with a field block using a local anesthetic. A 1:1 mix of 1% lidocaine with epinephrine 1:100,000 and 0.5% bupivacaine (Marcaine) with epinephrine 1:200,000 is used. Injections are performed deeply, down to bone along the orbital rim from lateral canthus to lateral canthus and from auricle to auricle across the crown of the head. Subcutaneous injections are performed in the temporal region, fanning out from a point anterior to the ear and staying superior to the zygoma. Each of the incision sites are infiltrated with local anesthetic.
When performing an upper lid blepharoplasty with an endoscopic brow lift, we begin with the blepharoplasty. A conservative excision of skin only is performed. We use five incisions for the endoscopic brow lift: one central, two paramedian, and two temporal. The central and paramedian incisions are 2 cm in length, oriented in a vertical direction, and placed 1 cm into the hairline. The two paramedian incisions are placed 4 to 6 cm lateral to the central incision and must not be placed in either a natural part or a designed part. The temporal incisions are oriented parallel to the lateral brow with the medial extent just crossing the temporal line. The incisions should be placed fairly anterior within the temporal tuft of hair.
The temporal incisions are made first and carried down to the deep temporal fascia. The plane of dissection can be confirmed by incising the fascia and identifying temporalis muscle. Blind blunt dissection posteriorly and medially, breaking through the temporal line into the subperiosteal plane, is performed. Anterior dissection should be done with visualization through all of the incisions. A lifting sweeping motion is used to lift all tissue off of the fascia. The dissection is fairly easy anterolaterally and along the temporal line. As the lateral supraorbital region is approached, there is a confluence of fascial layers that makes dissection more difficult. There is a consistent perforating vein medial and superior to the sentinal vein that will be encountered and cauterized. Dissection continues toward the lateral canthus to identify the sentinel vein. A branch of the zygomaticotemporal nerve travels with the sentinal vein; sparing this will significantly reduce postoperative numbness and paresthesias (Fig. 4.6.2). Dissection is then carried inferomedial to the sentinal vein to the level of the zygomatic arch. The subperiosteal dissection should be performed to the orbital rim and carried laterally to the level of the lateral canthus.
The three central incisions are made down to bone and a subperiosteal dissection is initiated. Blind posterior dissection is performed to allow for scalp mobilization. Anteriorly the dissection should be performed under direct vision because a better periosteal flap will be maintained and sensory nerves originating from a supraorbital foramen can be identified and spared. The dissection is continued inferiorly, exposing the orbital rim from lateral canthus to lateral canthus. The
supraorbital neurovascular bundle is identified and the periosteum is incised from lateral canthus to lateral canthus. Lateral to the supraorbital bundle, the orbicularis muscle is sharply or bluntly divided to reveal the superficial fat. Medial to the neurovascular bundle, the corrugator and procerus are identified and divided to obtain a medial release. Particular care is paid to the corrugator fibers inserting superficial and lateral to the supraorbital nerve (Fig 4.6.3). The supratrochlear nerve branches are encountered as the corrugator is dissected and should be spared (Fig. 4.6.4). Superficial to the corrugator, the depressor supercilii and orbicularis oculi are encountered, and these should be incised. The goal is complete removal of all
depressor muscle function on the brow, which can be confirmed by observing each brow rise as the muscles are released.
supraorbital neurovascular bundle is identified and the periosteum is incised from lateral canthus to lateral canthus. Lateral to the supraorbital bundle, the orbicularis muscle is sharply or bluntly divided to reveal the superficial fat. Medial to the neurovascular bundle, the corrugator and procerus are identified and divided to obtain a medial release. Particular care is paid to the corrugator fibers inserting superficial and lateral to the supraorbital nerve (Fig 4.6.3). The supratrochlear nerve branches are encountered as the corrugator is dissected and should be spared (Fig. 4.6.4). Superficial to the corrugator, the depressor supercilii and orbicularis oculi are encountered, and these should be incised. The goal is complete removal of all
depressor muscle function on the brow, which can be confirmed by observing each brow rise as the muscles are released.
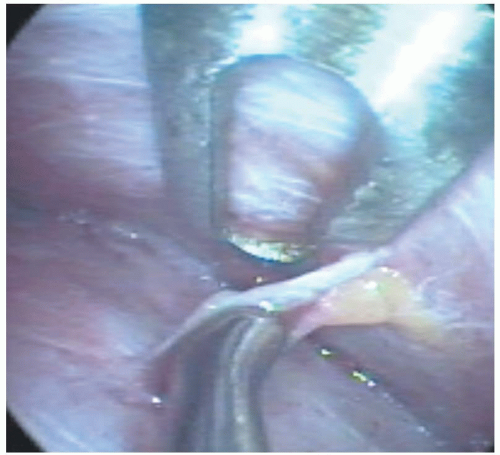 Figure 4.6.2. Intraoperative photograph of the sentinel vein adjacent to a branch of the zygomaticotemporal nerve. The nerve and vein are being separated by the dissecting instrument. |
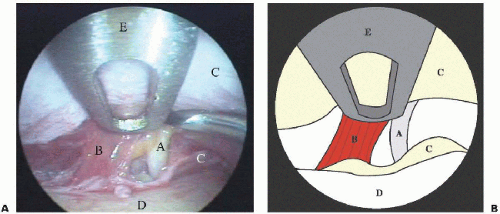 Figure 4.6.3. A: Intraoperative photograph following periosteal release, prior to myotomies. a, supraorbital nerve; b, corrugator supercilii muscle; c, periosteum, d, frontal bone; e, endoscope. B: Diagram demonstrating intraoperative view shown in Figure 4.6.3A. |
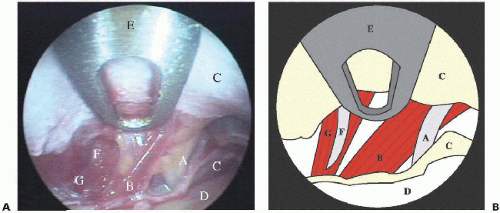 Figure 4.6.4. A: Intraoperative photography demonstrating partially completed corrugator supercilii myotomy. a, supraorbital nerve; b, corrugator supercilii muscle; c, periosteum; d, frontal bone; e, endoscope; f, supratrochlear nerve; g, depressor supercilii muscle. B: Diagram demonstrating intraoperative view shown in Figure 4.6.4A. Corrugator supercilii muscle is shown intact in this drawing. |
After the muscles are released, a lateral suture suspension is performed using 3-0 polydioxanone (PDS), a long-term resorbable monofilament suture. A suture is placed in the superficial temporal fascia at the anterior aspect of the temporal hair tuft and sewn down with significant tension in a posterolateral direction to the deep temporal fascia. This suture is used in all patients and may cause skin dimpling, which should resolve quickly. For patients in whom an aggressive lateral brow elevation is desired, a second suspension suture can be placed near the tail of the brow. This suture also is placed into the superficial fascia and sewn down with tension in a posterolateral direction. Following completion of the suture suspension, fibrin sealant (Hemaseal APR Kit, Haemcaure Corporation, Sarasota, FL) is placed along the superior orbital rim deep to the periosteum. One milligram of fibrin sealant is diluted per the manufacturer’s instructions and injected as the final step. Pressure is applied to the flap after placement of the fibrin sealant for 2 minutes. The incisions are closed in a single layer with a 3-0 Prolene. No dressing is applied.
Endoscopic Brow Lifting: Issues and Controversies
Is the Endoscope Necessary?
Advocates of blind dissection believe the endoscope needlessly adds time and expense to the procedure. The advantages of the endoscope are visualization of the surgical planes and precise and complete dissection of the depressor musculature. We believe that much of the dissatisfaction with this technique is a result of incomplete muscle dissection.
Plane of Dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree