33 Emergency Preparedness in Hair Restoration Surgery
Summary
Keywords: emergency management BLS protocols C-A-B A-B-C office preparedness automated external defibrillator cardiopulmonary resuscitation chest compression-to-breathing ratio “crash cart”
Key Points
•Discuss how a physician can prepare oneself, a facility, and its staff to respond to an emergency.
•Review updated recommendations of Basic Life Support protocols.
•Discuss newer internationally accepted paradigm of Compression, Airway, and Breathing (C-A-B) versus Airway, Breathing, and Circulation (A-B-C).
•Review priorities for managing specific scenarios that may occur in the outpatient hair restoration surgery setting.
33.1 Introduction
Although the likelihood of encountering emergencies in hair restoration surgery is low, the responsible hair restoration surgeon must be alert to the early signs of an evolving emergency and be prepared to respond quickly to prevent a negative or catastrophic outcome. While reports of emergency events occurring during hair restoration procedures have been published infrequently, protected information presented at recent Morbidity and Mortality conferences (International Society of Hair Restoration Surgery meetings, 2013–2019) confirm that serious medical emergencies, including cardiac arrests, myocardial infarction, anaphylactic reactions, seizures, and death, have occurred in the outpatient hair restoration setting.
The goals of this chapter are to describe how a physician, the facility, and its staff can prepare to respond to an emergency should one occur. Approaches to specific emergency situations that may arise in a hair restoration surgeon’s office will be discussed. Updated recommendations pertaining to Basic Life Support (BLS) will be reviewed. It is beyond the scope of this text to review specific protocols pertaining to Advanced Cardiac Life Support (ACLS).
33.2 Being Prepared
Fundamental preparation involves proper training and knowledge, presence of appropriate emergency equipment and supplies, and ability to facilitate transportation via emergency medical services for definitive care. Reviewing specific emergency scenarios and their appropriate responses should be part of every hair restoration physician’s office practice.
The American Heart Association (AHA) BLS and ACLS protocols, which are updated every 5 years, are accepted approaches to management of any deteriorating patient.1 Numerous international organizations have also issued recent resuscitation guidelines that concur with the focus of the updated AHA protocols.2,3,4,5 They focus on detecting and treating life-threatening respiratory and circulatory compromise.
33.3 Basic and Advanced Life Support
33.3.1 The Impact of the Automated External Defibrillator
Within the field of hair restoration, there has been debate concerning what constitutes an appropriate level of emergency preparedness. Some have argued that the physician should maintain ACLS skills, including intubation and familiarity with advanced resuscitative measures and medications, while others have suggested that it is difficult and possibly detrimental for physicians to attempt infrequently used ACLS skills. They feel it is more appropriate for physicians in the outpatient setting to provide initial BLS and to rely on the emergency medical services systems to initiate definitive ACLS skills.
Prospective studies have shown that only two treatment interventions have a significant impact on a cardiac arrest patient’s survival. These are (1) early administration of cardiopulmonary resuscitation (CPR) and (2) early defibrillation.6,7,8,9 Every minute that passes between a patient’s collapse during cardiac arrest and defibrillation decreases the chance of survival by 7 to 10% in the absence of CPR. With CPR, the decline in survival rate per minute is less, at only 3 to 4% (Fig. 33.1).10
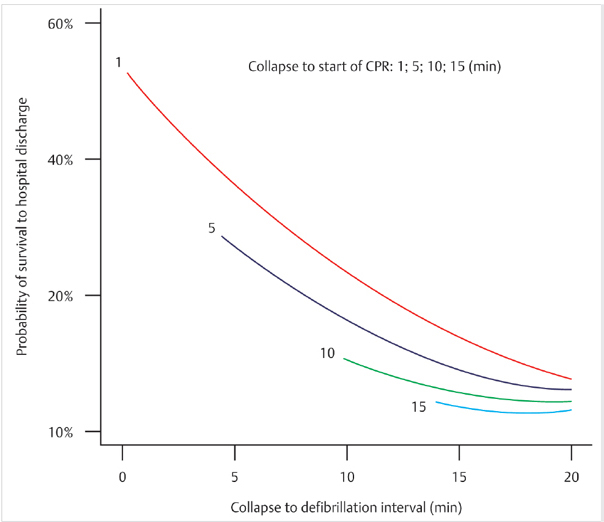
Fig. 33.1 Effect of collapse-to-cardiopulmonary resuscitation (CPR) interval and collapse-to-defibrillation interval on survival to hospital discharge.
These data led to the development of the AED, which is a device that talks an inexperienced operator through the process of attaching the electrode pads, reads and interprets the cardiac rhythm, and advises about the need to defibrillate the patient. If defibrillation is indicated, the AED then instructs the operator to press the shock button. AEDs are effective, easy to use, and the AHA encourages early use of these devices in their BLS training protocols.10,11,12,13,14 By using an AED, the physician no longer needs to maintain rhythm strip interpretation skills. With this technology and the evidence that early BLS and defibrillation are the primary interventions in ACLS that correlate with survival, it seems reasonable that hair restoration surgeons will be able to provide this approach in their practice.15
33.3.2 Basic Life Support in the Medical Office
The AHA BLS Healthcare Provider Adult Cardiac Arrest Algorithm—2020 update is shown in Fig. 33.2.
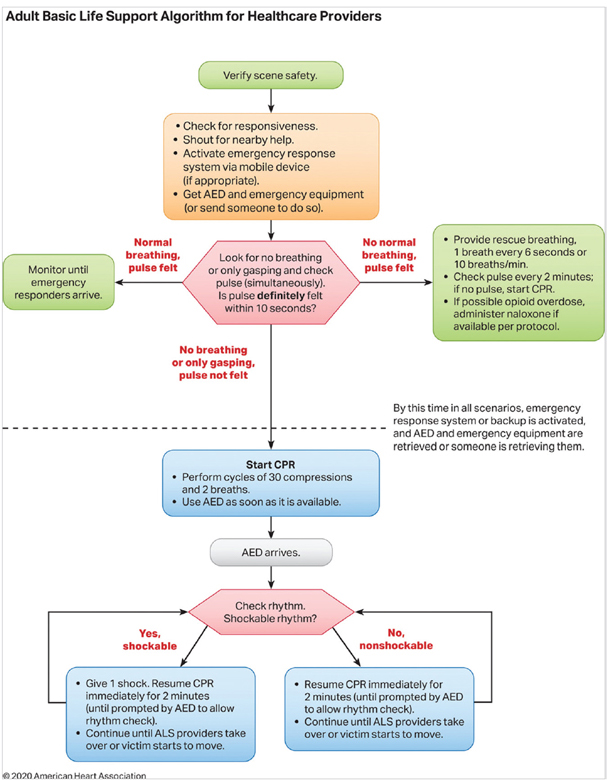
Fig. 33.2 BLS Healthcare Provider Adult Cardiac Arrest Algorithm—2020 Update.
Once victim unresponsiveness is established, and the emergency response system is activated, emergency equipment and AED should be obtained (or send someone to do so.)
Circulatory status can be assessed by feeling for a pulse, observing the skin color, and temperature, and noting patient’s level of consciousness. Peripheral pulses and capillary refill time are a very reliable estimate of BP (BP); therefore, the initial use of a sphygmomanometer in an unstable situation is unnecessary (Table 33.1).
Table 33.1 Correlation of pulses with blood pressure
Femoral pulse = systolic pressure >70 mm Hg |
Radial pulse = systolic pressure >80 mm Hg |
Nail bed capillary refill >2s means vascular compromise |
33.3.3 Initiating CPR with C-A-B Rather than A-B-C
Developments in the AHA and International Guidelines since 2010 with updates in 2015 and 2020 emphasize the reorientation of the sequence Airway, Breathing, and Circulation (A-B-C) to Compressions, Airway, and Breathing (C-A-B) to minimize the time to initiation of chest compressions.1,2,3,4,5,16 For out-of-hospital cardiac arrest (OHCA), it is reasonable for healthcare providers to provide chest compressions and ventilation though the AHA recognizes that chest compressions are the immediate priority in the unresponsive patient. In fact, chest compression-only CPR instructions may be recommended by emergency services dispatchers to inexperienced callers.
The AHA recommendations are made for “a simultaneous, choreographed approach to performance of chest compressions, airway management, rescue breathing, rhythm detection, and shock delivery (if indicated) by an integrated team” of trained rescuers.1
The basic steps in CPR are the following:
•Compressions: Components of high-quality CPR include (1) ensuring chest compressions of adequate rate (100–120/min); (2) ensuring chest compressions of adequate depth (at least 2 inches or 5 cm for an average adult); (3) allowing full chest recoil between compressions; (4) minimizing interruptions in chest compressions; and (5) avoiding excessive ventilation.
•In adult cardiac arrest, “total preshock and postshock pauses in chest compression should be as short as possible” because shorter pauses have been associated with greater shock success.
•Airway: Patients with an altered level of consciousness must have attention given to their airway. The opening and clearing of the airway is a critical intervention of emergency care. There are several techniques for securing an airway; the simplest and most often effective is the jaw thrust (Fig. 33.3).
•Breathing: Verification that the patient is indeed breathing, getting air into their lungs, is the next important step in prioritized basic emergency care. Breathing may be confirmed by watching the patient’s chest expand and listening for breath sounds.
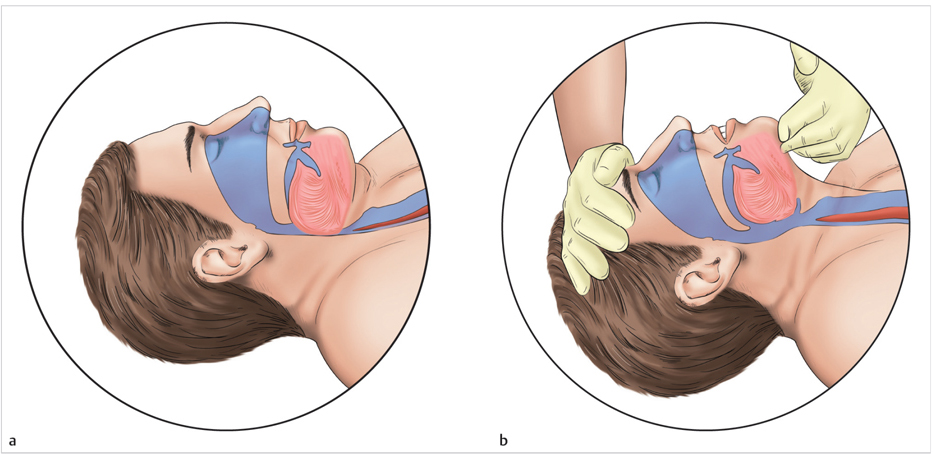
Fig. 33.3 Opening the airway. (a) Airway obstruction produced by tongue and epiglottis. (b) Relief by head tilt and chin lift.
In single-rescuer CPR, if pulses are absent, current BLS guidelines suggest that CPR be initiated at a ratio of 30 compressions to 2 rescue breaths and that an AED be utilized as soon as it becomes available. A ratio of 15 compressions to 2 breaths should be initiated if a second rescuer is available. If pulses are absent and there is more than one rescuer, CPR should commence while the AED is being connected. CPR should continue until the AED is connected to the patient and activated. Early defibrillation has increased the out-of-hospital survival of cardiac arrest patients to nearly 50%.17
Table 33.2 and Table 33.3 provide updated summaries of the AHA guidelines.
Table 33.2 Basic life support sequence
| Step | Lay Rescuer Not Trained | Lay Rescuer Trained | Healthcare Provider |
| 1 | Ensure scene safety. | Ensure scene safety. | Ensure scene safety. |
| 2 | Check for response. | Check for response. | Check for response. |
| 3 | Shout for nearby help. Phone or ask someone to phone 9-1-1 (the phone or caller with the phone remains at the victim’s side, with the phone on speaker mode). | Shout for nearby help and activate the emergency response system (9-1-1, emergency response). If someone responds, ensure that the phone is at the side of the victim if at all possible. | Shout for nearby help/activate the resuscitation team; the provider can activate the resuscitation team at this time or after checking for breathing and pulse. |
| 4 | Follow the telecommunicator’s* instructions. | Check for no breathing or only gasping; if none, begin CPR with compressions. | Check for no breathing or only gasping and check pulse (ideally simultaneously). Activation and retrieval of the AED/emergency equipment by the lone healthcare provider or by the second person sent by the rescuer must occur no later than immediately after the check for no normal breathing and no pulse identifies cardiac arrest. |
| 5 | Look for no breathing or only gasping, at the direction of the telecommunicator. | Answer the telecommunicator’s questions, and follow the telecommunicator’s instructions. | Immediately begin CPR, and use the AED/ defibrillator when available. |
| 6 | Follow the telecommunicator’s instructions. | Send the second person to retrieve an AED, if one is available. | When the second rescuer arrives, provide 2-rescuer CPR and use the AED/defibrillator. |
| * AED indicates automated external defibrillator; BLS, basic life support; and CPR, cardiopulmonary resuscitation. Telecommunicator and dispatcher are terms often used interchangeably. | |||
Table 33.3 Basic life support dos and don’ts of adult high–huality CPR
| Rescuers should | Rescuers should not |
| Perform chest compressions at a rate of 100–120/min | Compress at a rate slower than 100/min or faster than 120/min |
| Compress to a depth of at least 2 inches (5 cm) | Compress to a depth of less than 2 inches (5 cm) or greater than 2.4 inches (6 cm) |
| Allow full recoil after each compression | Lean on the chest between compressions |
| Minimize pauses in compressions | Interrupt compressions for greater than 10 seconds |
| Ventilate adequately (2 breaths after 30 compressions, each breath delivered over 1 second, each causing chest rise) | Provide excessive ventilation i.e., too many breaths or breaths with excessive force) |
| Abbreviation: CPR, cardiopulmonary resuscitation. | |
33.4 Preparing the Staff: A Team Approach
It is important to recognize that the sequence of steps described in BLS is intended to set priorities for the single- or double-person rescue. In actuality, it is much better and efficient to use a team approach where many of these activities are done simultaneously. For example, one person clears and secures the airway, while another checks for a pulse and starts CPR, and yet another gets the AED and calls the emergency medical services. In a medical office, this team approach is very helpful in bringing order to a potentially chaotic situation. Delegating, training and practicing these skills create a level of confidence that prevents panic and encourages a cool, methodical response necessary to handle any critical situation (Table 33.4). Mock emergency drills can be done to give the staff opportunities to practice their skills.
Table 33.4 Emergency “crash cart” equipment
Defibrillator monitor or AED | Oxygen tank |
Stethoscope | Ambu bags |
Sphygmomanometer | Oxygen (nonbreathing) masks |
EKG electrode packs | Nasopharyngeal airways |
EKG paper |







