Direct-To-Implant Breast Reconstruction with Acellular Dermal Matrix
C. Andrew Salzberg
R. Michael Koch
The surgical treatment for breast cancer has evolved considerably since the era of Halsted’s radical mastectomy. For many women today, the innovation of the modified radical mastectomy has given way to breast conservation techniques utilizing oncoplastic principles. The ultimate manifestation of this advance can be seen in skin-sparing and nipple-sparing mastectomies. These innovations have now provided plastic surgeons with the opportunity to perform breast reconstruction with the advantage of an intact skin envelope.
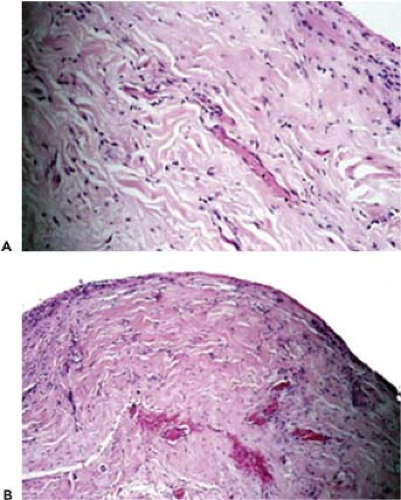
Acellular dermal matrix (ADM) is a biotechnological tissue prepared from either human or porcine skin in which the cellular components that cause rejection and inflammation have been removed. The resulting structurally intact tissue matrix provides the biologic scaffold necessary for normal tissue in growth and cellular repopulation as well as the biochemical components needed to initiate angiogenesis and revascularization, thus inducing intrinsic tissue regeneration. Acellular dermal matrix has been used extensively for soft tissue augmentation, including lip augmentation, depressed scar tissue repair, malar and submalar augmentation, and rhinoplasty. In all of these settings, this graft tissue has proven to become well integrated, with excellent postoperative healing, little resorption, and minimal risk for infection, extrusion, hematoma, or seroma. In addition, because this tissue has no cellular components, it may have a greater tolerance for ischemia, as it appears the graft is capable of remaining in place without breakdown until vascular ingrowth and cellular incorporation develops. This process can be demonstrated by a biopsy of the ADM (Fig. 34.1).
Since 2001, we have utilized these unique properties of ADM to provide coverage for either an implant or an expander. Our choice of which prosthesis to use has relied on two important conditions: the vascularity of the overlying postmastectomy skin envelope and whether or not additional skin surface area is required to create a natural breast shape.
Significantly, skin-sparing mastectomy combined with minimal incisional scarring allows the reconstructive surgeon to focus on how best to replace the glandular volume without the restraint of providing donor skin of similar color and texture. The question of which surgical technique to employ has also become more complex, and the challenge that now exists is how to choose the appropriate procedure for each patient. The current surgical repertoire comprises numerous autologous tissue flaps, including pedicled flaps, free tissue transfers, and perforator flaps. In addition, prosthetic techniques utilizing tissue expanders and implants remain popular choices. The advantage of using a prosthetic approach continues to be the relative simplicity of the procedure as well as the avoidance of distant donor-site morbidity. The disadvantage has been the need for tissue expansion with the inconvenience of serial office visits, whose number can vary considerably depending on the patient’s comfort level and the total fill volume.
With the discovery of genetic markers of breast cancer risk, the demand and indications for prophylactic mastectomy have increased. Furthermore, patients are adamant that their choices include procedures with reduced operative time and postoperative recovery. These issues naturally led to the development of a technique that would provide a combined, single-stage approach for both the mastectomy and the reconstruction. The advantages of a single direct-to-implant operation, particularly in the prophylactic mastectomy patient, are obvious, and the direct-to-implant technique with ADM attempts to make available a viable alternative to the other, better-established reconstructive techniques. The indications for this approach, however, are quite specific and should be thoroughly familiar to both the surgeon and patient prior to selecting this option.
The Consultation
A comprehensive consultation with the patient prior to surgery is crucial. This initial meeting provides the opportunity to review the risks and benefits of all reconstructive options. Patients who are able to have skin-sparing or nipple-areola-sparing mastectomies are prime candidates; however, the essential common denominator is the creation of viable skin flaps that provide adequate soft tissue coverage. Preoperative assessment also includes establishing candidacy for the direct-to-implant technique. This determination is directly related to the patient’s body habitus, the ablative nature of the surgery, and the specific desires of the patient for contralateral breast symmetry. Patient expectations must be reviewed and a realistic understanding of the pros and cons of the surgery established. Finally, preoperative coordination with the surgical oncologist will assure a clear understanding of the surgical strategy being planned.
Indications
Skin-sparing mastectomy is indicated in patients with stages 0 to II breast cancer who are also planning for immediate reconstruction. Prophylactic mastectomy may be offered to patients who present with a high risk for developing breast cancer or for the patient who is considering prophylactic mastectomy on the opposite breast. In either situation, a direct-to-implant technique can be employed.
The ideal candidate for the direct-to-implant technique is a woman with a C cup or smaller breast size, grade 1 to 2 ptosis, and good skin quality. Patients with a history of smoking are required to abstain for 4 weeks prior to and after surgery. Morbidly obese patients are generally poor candidates for implant reconstruction
and are usually better served by an autologous option such as a latissimus dorsi myocutaneous flap.
and are usually better served by an autologous option such as a latissimus dorsi myocutaneous flap.
Contraindications
There are relatively few contraindications to the direct-to-implant technique. The most important consideration is how to proceed in the setting of radiation therapy. If the patient has received prior postlumpectomy radiation treatment and the skin changes are severe with a firm and nonexpansive skin envelope, it is our practice to recommend autologous tissue reconstruction. In our experience with those patients who have mild skin changes after receiving radiation therapy in the past, the chance of a vascular incorporation of the ADM in the radiated-skin milieu is good with an excellent chance for a successful outcome.
In patients who are scheduled to receive adjuvant radiation therapy and who have declined an autologous tissue option, it is our practice to place a tissue expander in lieu of an implant. A pectoralis acellular dermal matrix covering is created in the usual fashion. Expansion is performed rapidly with the goal volume reached prior to the initiation of the radiation treatment.
We have also had patients in our series who required unanticipated radiation treatment. In those patients, the treatments were delivered after adjuvant chemotherapy. In this group, there has been no evidence of capsular contracture developed to date.
If there is any doubt as to the viability of the skin flaps, then the procedure should be modified and an expander placed in the submuscular ADM pocket. A sufficient volume can then be injected into the expander, just enough to gently fill the skin envelope (“hand-in-glove” fit). In this way, skin tension can be avoided and filling of the expander can be performed once the skin has healed sufficiently.
A special consideration must be made for those patients presenting for prophylactic mastectomy who also desire a significant reduction in their breast size. In this situation, we do not recommend a nipple-sparing approach, as the viability of the nipple-areolar complex may be tenuous in the setting of a skin reducing pattern or inverted-“T” incision. Free nipple grafting has been performed in carefully selected settings with good outcome but is subject to nipple loss from poor vascularity.
Preoperative Planning
As stated previously, the quality of the skin flaps after mastectomy is a critical component for a successful outcome. Choosing the appropriately sized implant to fill the space beneath these flaps is also an important consideration. We carefully measure the patient’s chest wall dimensions and also use an array of sizers preoperatively to gauge the anticipated volume that will be required after the mastectomy. In addition, a volumetric computer program can be used.
In our experience, we have found that smooth, round silicone gel implants provide the best projection and shape. A notable point is to have an implant base width that complements the chest diameter, as a concave lateral chest contour will result if the implant is not sufficiently wide. We do not routinely recommend saline implants because they often produce an inadequate aesthetic shape in a reconstructed breast and are prone to greater visibility and palpability as well.
There are many types of ADM available. The two major sources of skin utilize either a human or porcine model that is cleaved of cells and processed to create a framework of collagen into which cells can migrate (Table 34.1).
Table 34.1 Biologic Materials Currently Available For Breast Reconstruction | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The excellent experience with this graft in a wide range of soft tissue procedures has supported the rationale for its use in the postmastectomy setting where an inadequate muscular coverage exists. The potential for revascularization varies with both the source and thickness of the material. These materials,
however, have been utilized extensively throughout the body, significantly in abdominal wall and head and neck reconstruction. See Figure 34.2.
however, have been utilized extensively throughout the body, significantly in abdominal wall and head and neck reconstruction. See Figure 34.2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree