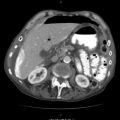
Fig. 22.1
Grasp the abdominal wall with towel clips and inject saline
You should confirm that you are in the peritoneal cavity by watching saline flow easily from the needle into the abdomen; double-check this by disconnecting the syringe and watching the saline flow freely down the needle. Then place the wire through the needle, and withdraw the needle over the wire, leaving only the wire in place. Some DPL kits come with a dilator, which you should use at this point to make the placement of the catheter easier. Next, you insert the DPL catheter over the wire and into the abdomen, again aiming toward the pelvis (Fig. 22.2). Holding the catheter close to its point of insertion and gently rotating it continually as it is inserted helps it pass through the abdominal wall more easily. Once the catheter is in place, you should aspirate it gently, looking for the presence of >10 mL of blood or enteric contents such as bile or vegetable matter. If none of these are present, infuse a liter of warmed saline into the patient’s abdominal cavity. As some DPL kits have relatively small catheters, you will normally find it necessary to squeeze the fluid in at this point or place it on a pressure bag. A very rapid infusion can be accomplished using the Level 1 Rapid Infuser to infuse the saline into the patient.
Fig. 22.2
Insert the DPL catheter over the wire and into the abdomen
It is important to retain a small amount of saline in the bag at the end of the procedure and to not allow air to enter the tubing; otherwise the capillary effect will be lost. After about 970–980 mLs have been instilled, you should lower the bag below the level of the patient, and the capillary effect will draw back the fluid that has been instilled (Fig. 22.3). You can help this with gentle pressure and agitation on the patient’s abdomen and also with some careful rotation and movement of the catheter while being vigilant not to withdraw it and allow air to enter the tubing. It is important to try and get out as much fluid as possible, as this can influence the results of the cell count. Although prior studies have shown that a negative DPL can be obtained with as little as 100 mLs of fluid, you should wait until at least 400 mLs have been collected before sending the effluent for analysis.


Fig. 22.3
Lower the bag below the level of the patient, and the capillary effect will draw back the fluid that has been instilled
22.1.2 Open Technique
The open technique does not differ in its initial steps, but instead of just a vertical stab, a 2–5-cm vertical incision is usually necessary, with the exact size depending on the thickness of the abdominal wall and the operator’s skill. Again you should make this just above or below the umbilicus, depending on the presence or absence of pelvic fractures or a gravid uterus. Next, dissect down to the level of the fascia, taking care to minimize bleeding from the subcutaneous tissues and fat, which could potentially interfere with the result. Although having an electrocautery device is useful, if it is not available, using lidocaine with epinephrine can help to reduce any bleeding. Once you visualize the linea alba, make a small incision in the fascia (Fig. 22.4). Then grasp the peritoneum with two fine hemostats, and under gentle upward tension, make a small nick to safely enter the peritoneal cavity. Place the DPL catheter under direct vision into the peritoneal cavity and aspirate using a 10-mL syringe (Fig. 22.5). If it is not grossly positive, infuse a liter of warmed saline into the patient as per the closed technique.
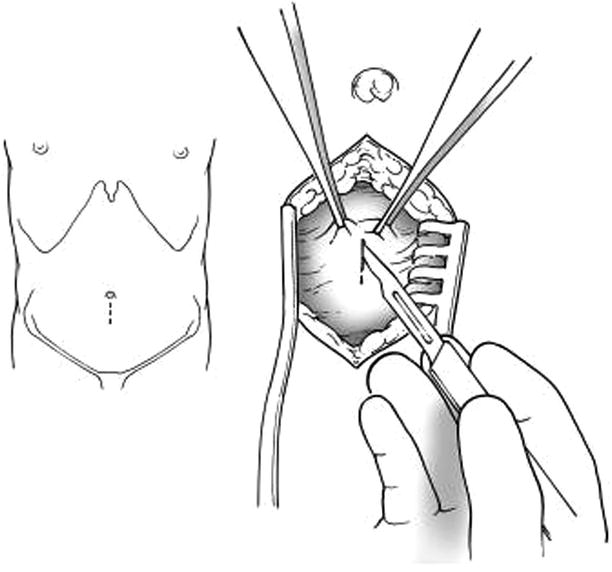
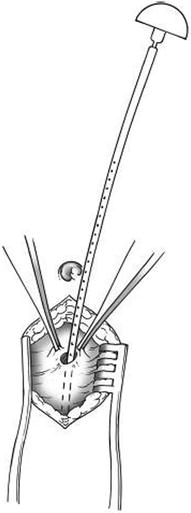
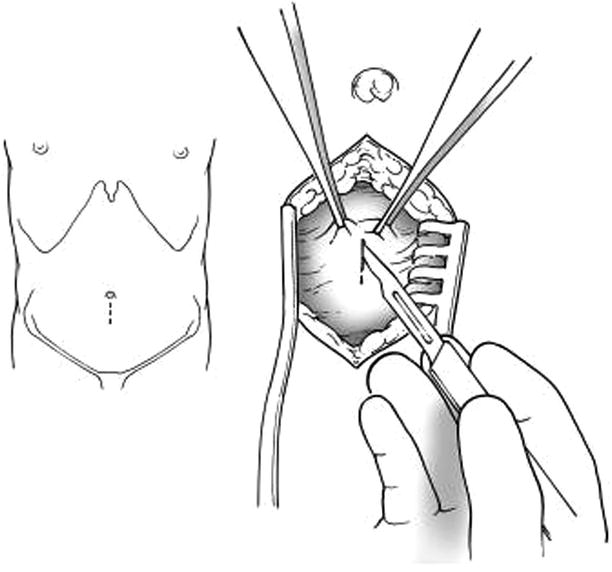
Fig. 22.4
Make a small incision in the fascia
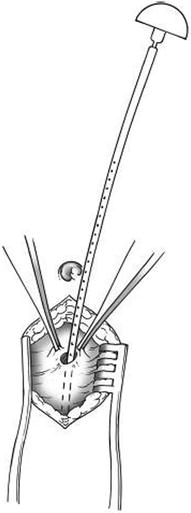
Fig. 22.5
Place the DPL catheter under direct vision into the peritoneal cavity and aspirate using a 10-cc syringe
22.2 Interpretation
If after placing the catheter into the abdominal cavity your initial aspiration yields greater than 10 mL of blood or if bile or vegetable matter is present, then this is considered a positive test, and the patient should be taken directly to the operating room. While there is a general agreement of what constitutes a positive test for blunt trauma patients (>100,000 RBCs/mm3, >500 WBCs/mm3, bile, food fibers, or amylase higher than the serum amylase), the same is not true for patients sustaining penetrating trauma.
If a red cell count of 100,000/mm3 is used, there is a low risk of a nontherapeutic procedure, but some authors feel there is a greater risk of a missed injury (false negative) of 9–11 %. The converse is also true; if the cell count is lowered to 10,000 RBCs/mm3, there is a false-positive rate of between 12 and 14 %. One must weigh the risk/benefit of a missed injury vs. a nontherapeutic celiotomy. Recent data would suggest that if the same criteria are used for penetrating trauma as recommended above for blunt trauma (RBCs, WBCs, bile, food fibers, and amylase), there will be no greater risk of a missed injury. It is our preference to use 100,000/mm3 as a positive cell count, but observe the patient closely for 23 h even if it is negative to prevent missed injuries. If there is a suspicion for a diaphragm injury, then diagnostic laparoscopy is preferred, as DPL has a low sensitivity for this injury. The white cell count, although also controversial, is helpful in identifying bowel injuries if the DPL is performed at least 3 h after injury. The accuracy of enzyme assays from lavage fluid has unfortunately been shown to be of limited value.
Although rarely used in the pediatric population, there are some variances that need to be considered. The amount of fluid infused should be 10–15 mL/kg, and the cell counts must be adjusted for the smaller amount of fluid infused. The values used for adult patients are then adjusted on the basis of a 1-L dilution. If only 500 mL is infused, a positive red cell count would be greater than 200,000.
22.3 Current Status of DPL
As paradigms shift, so does the management of patients. With the advent of nonoperative management of many trauma patients and the introduction of newer studies such as the FAST and newer high-speed CT scans, diagnostic peritoneal lavage has assumed far less of a role than in years past. Because of its limited use, it has been abandoned in some centers and newer trainees now have little or no experience with its use. In spite of the popularity of the FAST, one must take into account that it is operator dependent and there are technical limitations. Likewise, a CT scan can be time-consuming, expensive, and exposes the patient to considerable radiation exposure. Table 22.1 summarizes the advantages and disadvantages for the various investigative modalities.
Table 22.1
Summary of DPL versus other diagnostic modalities
DPL | FAST | CT scan | |
|---|---|---|---|
Time | 20–30 min | 1–2 min | Variable |
Repeatability | Possible, but rarely performed | Easy, often performed | Repeatable |
Safety | Low risk (<2 %) | No risk | Unknown risk (long-term radiation) |
Reliability | Not organ specific | Operator dependent | Obesity, movement |
Not indicated for retroperitoneal injuries | Not organ specific | Misses some injuries | |
Sensitivity | High | Medium | High |
Specificity | Low | High | High |
Advantages
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|