Dermatology for Plastic Surgeons I–Skin Care and Benign Dermatologic Conditions
Renato Saltz
Bianca M. B. Ohana
INTRODUCTION
The skin is the largest organ in the human body. It serves as a mechanical and immunologic barrier and is responsible for thermoregulation and sensibility. Healthy skin imparts the impression of health and beauty, while unhealthy skin suggests premature aging and illness. Plastic surgeons require a working knowledge of both benign and malignant skin conditions; appropriate treatment can only be rendered if the correct diagnosis is made. This chapter reviews the most common benign skin changes and presents a protocol for skin care that can be applied before or after facial aesthetic surgery or independent of aesthetic surgery. The next chapter addresses malignant skin conditions.
ANATOMY
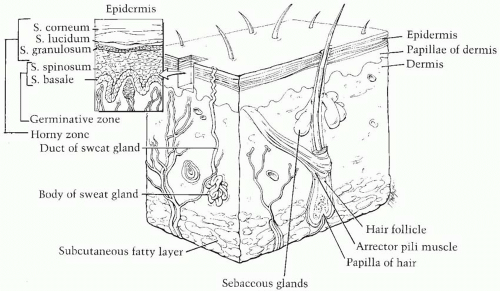
The skin is composed of two layers: the thin epidermis and the thicker dermis (Figure 13.1). Deep to the dermis is subcutaneous fat. There are two types of human skin: skin with hair and glabrous skin (without hair). The latter is found on the palms and soles and has a much thicker epidermis.
The epidermis consists of four layers: stratum corneum, stratum granulosum, stratum spinosum, and stratum basale. In glabrous skin, an additional layer (stratum lucidum) lies between the stratum corneum and the stratum granulosum. The epidermis contains predominantly keratinocytes, melanocytes, Langerhans cells and Merkel cells.
The dermis is divided into the more superficial papillary dermis and the deeper reticular dermis. The dermis contains predominantly fibroblasts, mast cells, histiocytes, monocytes, lymphocytes, and Langerhans cells. The integrity of the dermis is maintained by a supporting matrix containing ground substance and two types of protein fibers: collagen, which has great tensile strength and forms the major constituent of the dermis, and elastin, which makes up only a small proportion of the bulk.1 The skin appendages like hair follicles, sebaceous glands, and apocrine and eccrine glands are also found in the dermis.
BENIGN LESIONS
Pigmented Lesions
Nevus or Melanocytic Nevus.
Nevi are acquired lesions that present after birth and consist of a concentration of nevus cells that are classified according to their location as junctional (at the epidermal-dermal junction), intradermal, or compound (both in the dermis and at the junction). Junctional nevi are frequently found on the palms and soles and tend to be uniform, macular, and round with smooth and regular borders. Intradermal nevi are found on the face and are usually homogeneous, elevated, dome-shaped, skin-colored lesions. Compound nevi are raised above the epidermal surface and may be round or oval. The color varies with the natural pigmentation of the patient and may be very dark. There is usually little if any pigment on the flat surrounding epidermis in a classic, non-dysplastic, compound nevus.1 Nevi are rarely premalignant. See dysplastic (atypical) nevi below (Figure 13.2).
Congenital Melanocytic Nevus.
Congenital nevi are present at birth, usually singular and small. They are classified in three types depending on the size: small, intermediate, and giant (>20 cm) (Chapter 20). They have some potential to develop melanoma, although this risk is low except in the giant variety. Except for size, the overall appearance of congenital melanocytic nevi and acquired nevi is similar.2 Congenital nevi, however, may have dark, thick hair. Histologically, congenital nevi are distinguished by the presence of nevomelanocytes in the epidermis and in the dermis as sheets, nests, cords, or single cells.2 For treatment, see Chapter 20 (Figure 13.3).
Blue Nevus.
Blue nevi appear bluish because the nevus cells are deep in the dermis. These lesions are usually benign but the literature suggests they can be malignant. Clinically, blue nevi are solitary, nodular lesions with a smooth surface that tend to be blue or blue-gray. These lesions are generally treated conservatively unless there has been a change in their appearance or the patient requests excision for cosmetic reasons. The excision should include the subcutaneous component to ensure complete removal of deep dermal melonocytes.3
Halo Nevus.
When a melanocytic nevus is surrounded by a hypopigmented halo, it is termed a halo nevus. These lesions tend to occur on the torso in older children and teenagers. They are common, frequently multiple, usually acquired and asymptomatic. The central nevus tends to gradually disappear leaving a macular area of non-pigmented skin. This hypopigmented area may persist for years and may gradually return to a normal color. When biopsies are performed,
there may be no trace of the original lesion.1 The treatment is expectant, avoiding sun exposure at the hypopigmented areas unless there are cosmetic concerns or the lesions have atypical features.
there may be no trace of the original lesion.1 The treatment is expectant, avoiding sun exposure at the hypopigmented areas unless there are cosmetic concerns or the lesions have atypical features.
Spitz Nevus.
This is a common and usually acquired lesion predominantly in children and young adults but can be found in older people as well. Spitz nevi are usually firm, domedshaped, reddish or dark brown nodules, frequently on the head and neck. They are compound nevus variations, which have distinctive histologic features that make the differentiation from malignant melanoma difficult.1 The treatment is surgical excision. There is controversy over whether an entity known as a malignant Spitz nevus exists or if these lesions are malignant melanomas. For these reasons, Spitz nevi require complete excision with histologic confirmation of clear margins.
Nevus of Ota.
Nevi of Ota are hamartomatous melanocytic lesions that occur on the face in the distribution of the ophthalmic and maxillary division of the trigeminal nerve. They are much more common in women. The sclera is involved in two-thirds of cases.1 The treatment consists of laser therapy, using the Q-switched ruby, neodymium:yttrium-aluminumgarnet (Nd:YAG) or alexandrite lasers,4 or make up camouflage (Chapter 18).
Atypical Moles–Dysplastic Nevi.
Dysplastic nevi are melanocytic nevi that have the clinical features of melanoma: asymmetry, border irregularity, color variability, and diameter greater than 6 mm (Chapter 14). When patients present with many atypical moles, they are at higher risk for melanoma. Patients who present with many atypical moles and a strong family history of malignant melanoma are at much higher risk for melanoma and must have at least annual full body examinations for their entire lives. It is difficult for even an experienced dermatologist to know when to recommend excisional biopsy. The best indication for biopsy is a change in clinical appearance. The ideal surveillance involves total body photographs, which are compared annually with the patient’s current condition in order to determine if any lesions have changed over time. The treatment is excisional biopsy. If step-sectioning of the entire specimen reveals melanoma, then further treatment is required (Chapter 14).
Solar Lentigo.
Solar lentigines occur on sun-exposed areas of the face, arms, and dorsum of hands, especially in lighter skinned white people with light eye color. These acquired lesions are pigmented macules that can be small or large, with a tendency to confluence and range in size from 0.2 to 2 cm. They become more numerous with advancing age. Treatment is not required. A biopsy is taken to exclude melanoma from any lentigo that develops a highly irregular border, a localized increase in pigmentation, or localized thickening.2 Bleaching agents like hydroquinone are not particularly effective. Topical tretinoin, microdermabrasion, or cryotherapy can be used.
Ephelides (Freckles).
These are small, less than 3 mm, red or light brown macules that appear on sun-exposed areas predominantly in fair skinned people with red or blond hair, but can appear in darker skinned individuals as well. There is no increase in the number of melanocytes, but rather an increase in the amount of melanin in the skin. They are common in childhood; however, they can be seen at any age. They are usually confined to the face, arms, and back. The number varies from a few spots on the face to hundreds of confluent macules on the face and arms. Treatment is not required, but sunscreen is recommended. Bleaching agents such as hydroquinone, peels, and intense pulsed light (IPL) can be used for cosmetic reasons.
Epidermal Lesions
Seborrheic Keratosis.
This is a common benign, usually pigmented, neoplasm in elderly people, arising from the basal layer of the epidermis and consisting of keratinocytes. The etiology is unknown, and factors like virus infection, genetics, and sun exposure can be related. Usually seborrheic keratoses are not photoinduced. These lesions occur in any body site (frequently in the face and upper trunk) and are usually asymptomatic or associated with itching. They are superficial verrucous plaques, smooth or rough, varying from 1 mm to several centimeters in size and varying from dirty yellow to dark brown. Histologically, they are characterized by hyperkeratosis, acanthosis, and papillomatosis. The classic description is of a “stuck-on,” waxy appearance. Surgical excision or shave excision is appropriate if the patient complains of cosmetic appearance. Other treatment options include curettage, cryotherapy, or trichloroacetic acid (TCA). There are times when the lesion is atypical and an excisional biopsy is indicated for diagnostic purposes (Figure 13.4).
Keratoacanthoma.
This is a common epithelial tumor related to sun exposure than may be better placed in the next chapter on malignant lesions. It is more common in white phototypes and is usually found on the face or upper limbs. Classically, it presents as a solitary papule that develops a crater-like central, keratotic core.5 The history is one of rapid growth over a few weeks. Spontaneous regression is said to occur, but most lesions are excised before it becomes clear if regression would have ever occurred. The histology is similar to squamous cell carcinoma and many consider it a low-grade squamous cell cancer. Surgical excision is usually the treatment of choice. Other potential treatment options are curettage, coagulation, and topical 5-fluorouracil.
Verrucous Nevus.
These are congenital lesions that present as verrucous papules or plaques that are skin colored or brown. A linear configuration is common and it can be found in any body site. Malignant transformation is very rare. The treatment options due to cosmetic concerns are surgical excision, laser, electrodissection, dermabrasion, cryotherapy, TCA, or topical retinoic acid.
Skin Tags (Acrochordon).
Skin tags are composed of loose fibrous tissue and usually occur as multiple skin-colored or tan, filiform or smooth-surfaced papules that are 2 to 3 mm in diameter. These small, soft, pedunculated lesions are frequently located on the neck or major flexures. The simplest and most expeditious treatment is shave excision with scissors or a scalpel blade.
Premalignant Lesions
Actinic Keratosis.
Actinic keratoses may be the most common of the premalignant skin conditions. Caused by sun exposure in people with Fitzpatrick skin types I, II, and III, they are macules or papules with a scaly surface, generally between 1 mm and 2 cm in diameter. Actinic keratoses occasionally evolve into squamous cell cancers and are therefore considered premalignant. These lesions frequently require biopsy to rule out a carcinoma. Multiple lesions are usually treated with 5-fluorouracil or the immune stimulator imiquimod (Aldara) (Figure 13.5).
Leukoplakia.
Leukoplakia is white intraoral plaque and is the most common precancerous lesion of the oral cavity. These lesions do not frequently become squamous cell cancer but must be followed and biopsied if they persist or undergo a change in appearance.
Cutaneous Horn.
A cutaneous horn is different from a skin tag and is considered a premalignant lesion. They are usually yellowish brown protuberant “horns” and are found on the face and ears. Histologically, they are characterized by a compact proliferation of keratin. The treatment is surgical excision.
Bowen’s Disease.
Bowen’s disease is squamous carcinoma in situ of the skin. This tumor presents as a slowly growing, red lesion with a scaly surface and irregular borders. Ulceration or bleeding may be a sign of invasive malignancy. The treatment of choice is surgical excision, but cryotherapy, curettage, cauterization, topical agents like 5-fluorouracil, and topical photosensitizer can also be considered.
HAIR FOLLICLE TUMORS
Trichofolliculoma
This is a rare hamartoma of the pilosebaceous follicle. They are typically solitary, small, raised nodules with two or three hairs, usually white, protruding together in a tuft. They frequently appear on the face and scalp. Malignant change is not typical but has been reported in a single case with perineural invasion.1 The treatment recommended is surgical excision.
Pilomatricoma, or Benign Calcifying Epithelioma of Malherbe
A pilomatricoma is a hamartoma characterized by a firm, solitary nodule covered with intact but often discolored skin. The calcification makes the lesions particularly firm. They can occur on any body part but are most commonly found on the face and upper extremities. In general, the lesions are 0.5 to 5 cm in diameter. There is no malignant potential. The treatment is surgical excision.
Trichoepitheliomas
Trichoepitheliomas are hamartomas of the hair follicle typically found in the center of the face. They tend to be small, skin-colored or slightly pink papules that are usually distributed symmetrically on the cheeks, eyelids, and the nasolabial region. Treatment is not required; excision may be contemplated for cosmetic reasons. Other options include electrodissection and curettage or cryotherapy. Recurrence is common.
ECCRINE TUMORS
Syringomas
This is a benign tumor that usually presents as firm, skin-colored to yellowish dermal papules on the lower eyelids, predominantly in females. Syringomas can be sporadic or familial and are frequently associated with Down’s syndrome. The treatment is punch or surgical excision for cosmetic reasons only. Electrodissection, curettage, and carbon dioxide laser can be considered.
Eccrine Poroma
An eccrine poroma is a solitary, firm, skin-colored or erythematous papule, usually on the sole or palm in adults. Ulceration and bleeding may occur at points of pressure. The treatment is surgical excision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree