Fig. 31.1
Example of a case with good local conditions for delayed breast reconstruction with definitive implants
31.2.3.2 Contraindications for Definitive Implants
Patients in this group have an absent pectoralis major muscle, rather tense cutaneous flaps, scars from very wide mastectomies, previous radiotherapy or a large, ptotic contralateral breast (Fig. 31.2). Such women need greater expansion and possibly require a contralateral breast procedure to improve the outcome.


Fig. 31.2
Example of a case in which reconstruction with a definitive implant is contraindicated owing to late side effects of radiotherapy
31.2.3.3 Indications for Temporary Expanders
Tissue expansion prior to the definitive implant is the first stage in the two-stage technique. The expander is used to distend the cutaneous flaps and to obtain more volume when the definitive prosthesis is inserted. It is indicated in a similar fashion to definitive implants. Also, older patients, those with significant medical comorbidity, and women with minimal abdominal tissue, in whom the autologous technique would be unsuitable, also benefit from this technique. Besides, the expander/implant technique is indicated for those patients devoid of sufficient skin or preserved subcutaneous tissue in flaps resulting from mastectomy. This may occur when there is little elasticity of the cutaneous flaps from mastectomy or in the case of a contralateral breast with a rather large volume. In these situations, the two-stage implant reconstruction usually yields esthetically superior results (Fig. 31.3).


Fig. 31.3
Example of case with good local conditions for reconstruction with a tissue expansion device
31.2.3.4 Contraindications for Temporary Expanders
These are basically the same as those for the use of definitive implants, with even more emphasis on the risk of expanders after radiotherapy [14]. A large number of authors have realized that several postoperative complications can ensue when attempting to distend previously irradiated tissues [12, 14–16], since the radiation decreases the elastic distension capacity of the tissue. In these cases, the most frequent complications are painful and difficult expansion with possible extrusion of the expansion device or periprosthetic capsule (Table 31.1). Even though one achieves the final stage of expansion, the cutaneous coverage of the prosthesis becomes too thin and fragile to protect the definitive implant (Fig. 31.4).

Table 31.1
Indications and contraindications of delayed breast reconstruction with temporary expanders and implants
Indications | Contraindications |
|---|---|
Patient preference | Previous radiotherapy |
Good quality of skin | Previous failure of breast reconstruction with implants |
Bilateral mastectomy | Morbid obesity |
Smokers |

Fig. 31.4
Example of case in which reconstruction with a temporary expander is contraindicated
31.3 Preoperative Evaluation
The primary objective in breast reconstruction is to obtain symmetry [17, 18]. For this reason, it is essential to prepare a preoperative plan that includes a detailed analysis of the healthy breast’s characteristics and the most suitable technique for treating this breast [19]. The aim is to obtain a breast with low projection in the upper pole, with no ptosis or tear shape. These characteristics are fundamental in order to achieve a successful reconstruction result (Fig. 31.5). Firstly, a clinical and radiologic preoperative evaluation is fundamental in order to properly choose the surgical technique. Secondly, apart from all the standardized examinations required in the anesthesiological preoperative appointment, it is also important that an oncologic evaluation be performed, surveying the following topics: type and size of tumor; number of positive lymph nodes; type of surgical procedure to be performed; chemotherapy, radiotherapy or hormone therapy procedures the patient is adherent; follow-up period; and the most recently performed radiologic examinations and blood tests. Furthermore, the evaluation of the contralateral breast is also mandatory in order to exclude bilateral neoplasm and should include mammographic and ultrasound examinations. It should also be noted that contralateral breast surgery—a reductive mastoplasty, a mastopexy, or an additive mastoplasty—is frequently required to obtain a pleasing symmetry. Moreover, the contralateral breast evaluation should also aim to examine any palpable nodule or any mammographic alteration, such as microcalcifications or imaging patterns consistent with a suspicious lesion. Finally, it is important to state that no therapy of any sort is permitted prior to the surgical procedure itself aside from the prophylactic endovenous antibiotic administration of a first-generation or second-generation cephalosporin before skin incision.
Fig. 31.5
Preoperative breast measurements
31.4 Operative Outline
31.4.1 Before the Operation
Firstly, the preoperative outline is designed on the day before the operation and the whole of the procedure is explained to the patient again so that informed consent is obtained. The patient is then placed standing and photographs are taken of the patient in profile and in a forward-facing position. It is very useful to make precise measurements of the contralateral breast on this occasion, such as base width, thickness of subcutaneous adipose tissue, height, and anterior projection.
31.4.2 Choosing the Implant
To help decide which implant one should use, it is important to compare the contralateral breast with the future implant with regard to the parameters of base, height, and anterior projection. This is done during the preoperative period in order to choose two or three models and sizes of implants that are most likely to be used during the surgical procedure (Fig. 31.6). The final decision can be made at the intraoperative stage, sometimes after the use of a sample. Surgeons should pay attention to whether the use of samples is prohibited in the country in which they work. In the European Union, for instance, the resterilization of samples is strictly forbidden. Nevertheless nonsterilized implants can be thoroughly coated with a highly adherent and resistant sterile plastic envelope, therefore permitting their repeated use. This technique for choosing the implants based on the aforementioned measures is much more precise and useful in cases in which it is necessary to use an expander and, subsequently, perform a contralateral augmentation mammoplasty. In cases that require breast augmentation surgery, we can use highly cohesive anatomic implants [20–22] or round implants. In cases of definitive implants with mastopexy or reductive mammoplasty of the contralateral breast, the decision as to the type and volume of the implant must also take into consideration the volume reduction, the change of shape, and the size reduction of the breast base. These calculations are based on augmentation mammoplasty articles [20, 23] which employed these methods to calculate the volume and shape of implants for esthetic improvement.
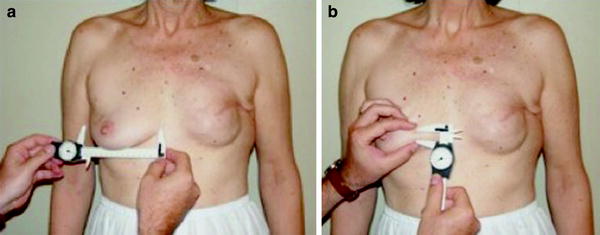
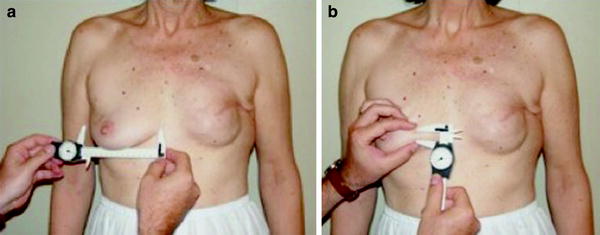
Fig. 31.6
a Example of taking the measurement of the base of contralateral breast for the choice of model and size of prosthesis to be used. b Example of “pinch” measurement, which gauges the thickness of the cutaneous and the subcutaneous tissue
31.4.3 Surgical Markings
Afterwards, lines are drawn on the patient’s chest to ensure the correct understanding of the anatomic condition. A median line should be drawn from the sternal notch to the xiphoid appendix, and the inframammary fold should be placed at the same height as for the contralateral breast. In the operating room, the patient is placed supine and with her arms parallel to her trunk. The operating table must be set in a way that the patient can be placed in a 90° position, i.e., sitting, at the end of the procedure.
31.4.4 Skin Incision and Scar Excision
The incision into which the implant will be inserted is made in the preceding mastectomy scar and, if possible, in the pectoralis major muscle. This technical detail allows a safer suture of the prosthetic pocket in two layers, namely, the muscular and the cutaneous layers. If a contralateral mammoplasty is required, the drawing is performed according to the technique chosen (Fig. 31.7). The skin incision with either partial or complete removal of the scar is chosen on the basis of three clinical situations:
Get Clinical Tree app for offline access










