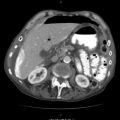
Fig. 43.1
Resuscitation using blood products and fluid warmer
43.4.2 Haemostatic Resuscitation (Fig. 43.1)
Early identification of patients with ongoing haemorrhage and the need for blood transfusion is essential so that the massive transfusion protocol can be activated. A ratio of 1:1:1 packed red blood cells (PRBCs)/fresh frozen plasma (FFP)/platelets has been adopted by most institutions as (though not perfect) the most ideal protocol for avoiding coagulopathy.
This ratio in combination with viscoelastic clotting studies such as thromboelastography (TEG) can guide therapy by identifying specific component deficiencies that need to be added to the current therapy. TEG has become standard of care in most major trauma institutions.
43.5 Stages of Damage Control
Damage control surgery (DCS) is regarded as having five stages:
Stage 1: Patient selection
Stage 2: Operative control of haemorrhage and contamination
Stage 3: Resuscitation in the intensive care unit (ICU)
Stage 4: Definitive surgery
Stage 5: Closure of the abdomen
43.5.1 Stage 1: Indications for Damage Control (Patient Selection)
Although the evidence is clear that damage control decreases mortality, it can be associated with an increase in morbidity, length of ICU stay, number of surgical procedures and cost; hence overzealous use should be avoided.
The decision to initiate damage control surgery should be taken early. The decision to do or not to do damage control is a dynamic process and can be changed as the patient’s physiological parameters change or if the magnitude of organ injury found during surgery forces damage control with packing to control haemorrhage. Care should be taken not to prolong ‘damage control surgery’ by trying to do too much in a patient that will benefit with minimal surgery (Fig. 43.2).


Fig. 43.2
Massive bleeding possibly mandating damage control surgery
Possible damage control surgery can be initiated by the following factors:
- 1.
Physiological parameters:
Nonresponder to resuscitation with systolic BP <70 mmHg
Temp <34 °C
pH <7.2
Lactate > 5 mmol/L
Worsening of intraoperative acidosis, hypothermia and coagulopathy
Increased inotropic requirements during surgery
- 2.
Anatomical parameters:
Injury Severity Score (ISS) > 25
Multiple cavity or multiple injuries that will need prolonged surgery to correct
Massive transfusion or fluid resuscitation with risk of abdominal compartment syndrome
Packing to control haemorrhage
Severe contamination
During disasters, damage control is standard to allow maximum use of available resources.
43.5.2 Stage 2: Operative Control of Haemorrhage and Contamination
43.5.2.1 General Principles
For damage control to be successful, it needs a team effort. The anaesthetic team should adopt the haemorrhagic resuscitation principles, cutting down on their clear fluids, the nursing staff should have a trauma cupboard ready with all possible equipment available for damage control (i.e. nasogastric tubes for shunting, GI staplers, packs for packing and the most likely sutures that are usually used during damage control).
The set temperature in the trauma theatre should be as high as possible (36 °C), the patient should be cleaned from the chin to the knees but cavities that are not being operated upon should be covered and warm fluids should be used all to combat hypothermia.
The cell saver should be available to return the patient’s blood cell loss. Some studies have shown that the usage of cell-saved blood is safe even in the setting of bowel perforation.
For damage control to be successful, there should be continuous communication between all the parties involved. The surgeon should inform all about the injuries sustained and ongoing blood loss and planned surgery; the anaesthetist should keep the surgeon and ICU informed about the physiological status, inotropic requirements, number of units of blood transfused and the duration of the surgery.
43.5.3 Chest
Damage control in the chest often ends up as definitive surgery as the chest will only present with haemorrhage, tamponade or a large air leak from the lung (Fig. 43.3).
Fig. 43.3
Massive bleeding (>1500 mL from the chest, mandating surgical intervention)
The most difficult decision is which incision to use to get the best possible access.
Median sternotomy is preferred for injuries to the anterior mediastinum, anterior cardiac surface and proximal control of the neck vessels. Sternotomy is usually indicated for any injuries to the chest medial to the midclavicular line and zone 1 neck wounds with active bleeding or large haematomas. The performance of a sternotomy does, however, require the use of a sternal saw, a Lebsche knife or a Gigli saw – equipment which is not always available in an emergency department (Fig. 43.4).
Fig. 43.4
Median sternotomy. Finochietto retractor insertion
The anterolateral thoracotomy is often used in the emergency department due to the speed in getting access into the chest. It is used for lung injuries, for cardiac injuries and for cross clamping the aorta. It can also be extended across the sternum to get access to both the chest cavities and right side of the heart – the so-called ‘clamshell’ incision.
The posterolateral thoracotomy is seldom used in patients in extremis due to the time it takes to position the patient and the time to get into the chest cavity due to the muscle bulk. The posterolateral thoracotomy is the incision of choice for injuries to the posterior mediastinum, to the oesophagus and to the descending aorta and also for bleeding posterior intercostal arteries.
Packing of the chest is not frequently performed, due to the large spaces and the effects on the haemodynamics and ventilation, but can be used as a desperate measure to control haemorrhage from penetrating trauma if direct control is not accessible.
43.6 Lung Injuries
The two indications to operate in an emergency on the lung are a large air leak and massive haemorrhage.
In both cases it is best to get initial control at the hilum to help assess the injury under controlled situation, avoid air embolism and allow adequate ventilation of the healthy lung and to slow haemorrhage down. To get access to the hilum, the inferior pulmonary ligament must be divided. It is best obtained with the ligament in your hand between your fingers and the lung being pulled towards you. Care should be taken so that the pulmonary vein is not damaged when approaching the hilum. A Foley catheter can be put around the hilum with a clamp, or the hilum can be clamped with a Satinsky vascular clamp applied from the superior aspect. Sometimes with hilar injuries, the proximal control should be obtained from within the pericardial sac.
With peripheral penetrating lung injuries, the tract should be opened with a tractotomy, performed with GI staplers or using bowel clamps. Once the tract is open, look for bleeding points or air leaks, and these should be suture ligated, or the tract resected with the linear GI stapler. If the injury is at the edge of the lung, a nonanatomical resection can be done with the stapler.
Large bronchial tears can be repaired, and very seldom is a lobectomy or pneumonectomy indicated (Fig. 43.5).
Fig. 43.5
(a) Patient with a stab wound anteriorly to the left of the sternum. (b) Ultrasound scan of the same patient showing cardiac tamponade
43.7 Cardiac Injuries
Releasing any tamponade and control of haemorrhage are the main priority in the management of cardiac injury. Whenever cardiac surgery is anticipated, always have warm wash and internal defibrillators ready to manage any arrhythmia as they occur.
Releasing the tamponade is often challenging, as the pericardium is usually very tense and a blade is needed to puncture the pericardium. Scissors should be used to extend the incision superiorly and inferiorly, thus avoiding the phrenic nerve. Care should be taken superiorly, as the pericardium reflects onto the ascending aorta.
Temporary control of the bleeding catheter in a penetrating cardiac injury can be obtained by inserting a Foley catheter into the hole, inflating the bulb using fluid and applying gentle traction with the bulb being inflated and the catheter clamped against the myocardium, using light forceps, e.g. a mosquito, to obtain haemostasis. Skin clips can be used to close the wound temporarily. Bleeding from the atrium can be controlled with a Satinsky clamp, and care must be taken to avoid obstructing venous return. Satinsky clamps should not be used on the ventricles as they may tear the cardiac muscle.
Permanent closure is then achieved with Prolene sutures with or without pledgets, depending on the status of the heart.
43.8 Tracheobronchial Injuries
These injuries are usually associated with a large leak on the ventilator or bubbling intercostal drain with a lung that doesn’t expand. Respiratory compromise determines how urgently surgical intervention is needed (Fig. 43.6).


Fig. 43.6
Chest drain bottle showing massive air leak
The best access to tracheobronchial injuries is with a posterolateral thoracotomy, and the transected bronchus is debrided and can be stapled or repaired with absorbable monofilament sutures.
43.9 Oesophageal Injuries
Ideally, Early oesophageal injuries should be primarily repaired as it is the best circumstances with possible the best outcome. As the mucosa of the esophagus is the strongest layer decent bites should be taken during repair. If there is an associated tracheal injury, a muscle flap (sternocleidomastoid or intercostal muscle depending on level) is usually secured between the oesophagus and the trachea to decrease the risk of a fistula.
Oesophageal repairs should have prophylactic drains placed close to the repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree