Introduction928
INTRODUCTION
CLINICAL AND MORPHOLOGICAL FEATURES
Time of development
Clinical aspects
Location of metastases
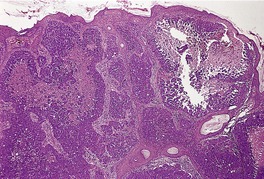
Fig. 39.1
Sites of the primary tumor
Prognostic aspects
Histopathological features
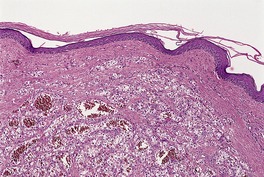
Fig. 39.2
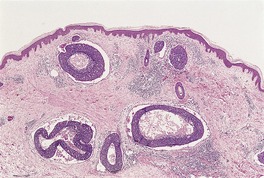
Fig. 39.3
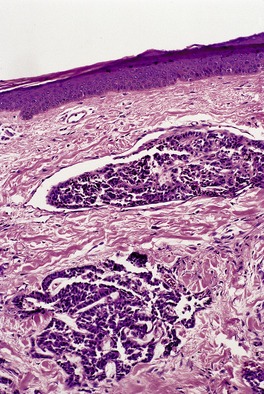
Fig. 39.4
SPECIFIC METASTASES
Breast
Histopathology
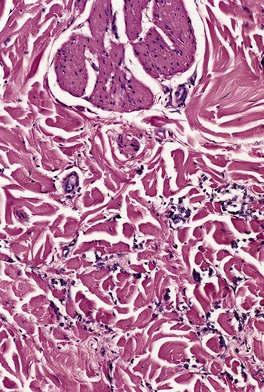
Fig. 39.5
CK7
Positive in two-thirds of cases
CK20
Negative
CK5/6
Negative
Estrogen receptor
Positive in 50%; high specificity
Progesterone receptor
Positive in nearly half; high specificity
GCDFP-15
Positive in 90% of lobular tumors with signet-ring cells, 70% of ductal carcinomas, but positive in some salivary gland and adnexal tumors
CEA
Positive in nearly 75%
S100
Positive in rare cases
Lung
CK5/6
Squamous cell carcinoma positive, mesothelioma positive, adenocarcinoma negative
CK7
Adenocarcinoma positive, squamous cell carcinoma negative, small cell negative
CK20
Squamous cell carcinoma negative, adenocarcinoma negative, small cell negative but Merkel cell carcinoma positive
TTF1
Adenocarcinoma positive, squamous cell carcinoma negative, small cell positive but thyroid also positive
CAM5.2 (CK8/18)
Small cell dot positivity
Ber-EP4
Adenocarcinoma positive, small cell positive
CEA
Adenocarcinoma positive, squamous cell carcinoma negative
Oral cavity and gastrointestinal system
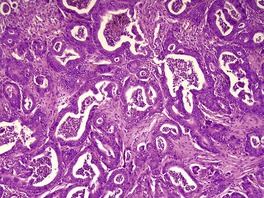
Fig. 39.6
CK5/6
Esophagus positive, other sites negative
CK7
Esophagus negative, gastric some positive, colorectal negative
CK20
Esophagus negative, gastric positive, colorectal positive
CEA
Gastric positive, colorectal positive
Ber-EP4
Esophagus and mouth positive
HIK1083
Gastric positive, adnexal carcinomas negative
Liver, pancreas, and gallbladder
Kidney
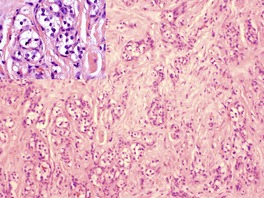
Fig. 39.7
CK7
Negative, but transitional cell tumors positive
CK20
Negative, but transitional cell tumors positive
RCC
Positive in two-thirds or more
Vimentin
Positive
CD10
Positive
Bladder and urethra
Male genital system
Female genital system
Thyroid
Carcinoid tumors
Histopathology
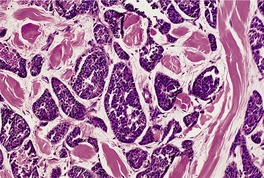
Fig. 39.8
Neuroblastoma
Histopathology
Melanoma
Histopathology
Miscellaneous tumors
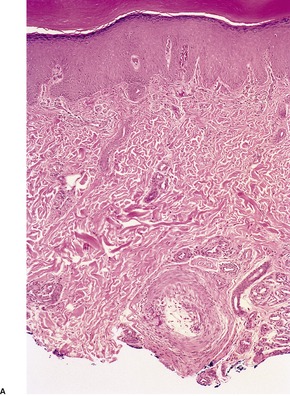
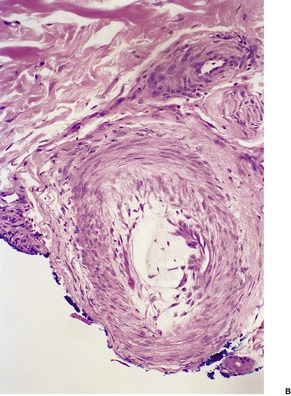
Fig. 39.9
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cutaneous metastases
Clinical and morphological features928
Virtually any tumor can metastasize to the skin, but some do so more often than others. 1 The identification of the primary site is not always easy and this process is further complicated by the occurrence of primary adnexal tumors of the skin that mimic various metastases. Immunohistochemistry has assisted in the specific diagnosis of these tumors but it should be remembered that the specificity of a particular marker declines with successive studies.
Metastasis represents the end stage of a complex series of interactions between the tumor cells and the host tissues.2. and 3. There are many factors which influence the localization of metastases other than the natural lymphatic and vascular connections of the primary tumor. In the past, the concept of ‘favorable soil’ and ‘unfavorable soil’ was invoked in an attempt to explain why certain organs were only rarely involved by metastases. There are now some scientific explanations available to account for the ‘unfavorable soil’ of some organs, although none has been advanced that explains satisfactorily why the skin generally is an uncommon site for visceral metastases. The vascularity of the scalp may explain why this is sometimes a favored site. The tumor cells may reach the skin by direct invasion from an underlying tumor, by accidental implantation during a surgical or diagnostic procedure, and by lymphatic and hematogenous spread.
Based on several large autopsy series of patients with visceral cancer, the incidence of cutaneous metastases is about 2% of all cases. 2 The usually quoted range from several different studies is 1.2–4.4%.4. and 5. A retrospective study in 1993 of 4020 patients with metastatic disease found that 10% had cutaneous metastases. 6 A study of 3827 autopsies carried out between 1914 and 1943, but published in 2008, found that 6% had cutaneous metastases. 7 The breast accounted for more than a half of these metastases. 7 In one series the skin was the 18th most frequent metastatic site for all tumor types. 8
Although it has little relevance to cutaneous metastasis, it should be noted that the Halstedian hypothesis of cancers arising in an organ, spreading to the regional area, and subsequently metastasizing is no longer tenable. 9 Widespread metastases can develop despite extensive loco-regional treatment. 9 Perhaps this has relevance to the management of melanoma!
There are many generalizations that can be made about cutaneous metastases. These relate to the time interval between their manifestation and the diagnosis of the primary tumor, their clinical appearance, their location, the site of origin of the primary tumor, and their prognostic significance. 10 These aspects will be considered below, followed by an account of the cutaneous metastases derived from various viscera.
Cutaneous metastases may be the first indication of a visceral cancer, 11 the incidence in one series being 0.8%. 12 These precocious metastases are particularly likely to present at the umbilicus, or less frequently on the scalp. The kidney, 13 lung, 14 thyroid, 15 and ovary11 are organs whose tumors may present in this way. 16
With most tumors the metastases develop some months or years after the primary malignancy has been diagnosed11– so-called ‘metachronous metastases’. In about 7% of cases, this interval exceeds 5 years. Tumors of the breast and kidney and malignant melanomas may give rise to delayed metastases. 17
The term ‘synchronous metastasis’ is used when the cutaneous metastasis and the primary tumor are diagnosed simultaneously. 18 This sometimes occurs with tumors of the breast and oral cavity.
Cutaneous metastases are more likely to be found in older individuals. 19 In neonates they are usually derived from a neuroblastoma or, less commonly, from a rhabdomyosarcoma. 20 Metastases from germ cell and trophoblastic tumors, although rare in the skin, develop there particularly in young adults.
Cutaneous metastases usually present as multiple, discrete, painless, freely movable nodules of sudden onset.6.16. and 21. They usually show rapid enlargement. 22 Sometimes several small nodules are localized to one area. 23 Solitary metastases occur in about 10% of cases. The nodules are usually 1–3 cm in diameter. Much larger lesions and also occult lesions have been recorded.24. and 25. They vary in color from red to bluish-purple to light brown or flesh colored. Occasionally plaques are formed. One variant of this form develops in the scalp as patches of alopecia (alopecia neoplastica), sometimes resembling alopecia areata.26.27.28.29. and 30. Cicatricial plaques also form: metastases from the breast,26. and 27. lung, and kidney may give this pattern on rare occasions.
There are isolated reports of other patterns of cutaneous metastases. 5 For example, they may resemble erythema annulare, 5 a chancre, 31 a hematoma, 32 an epidermal cyst, 33 a condyloma, 5 or an ulcer. 5 They may present in a zosteriform or target-like pattern.34.35.36.37.38.39.40.41.42.43.44.45.46.47. and 48. In one case, herpes zoster was associated with the metastases. 49 Elephantiasis of the lower limbs due to lymphatic obstruction and facial or eyelid lymphedema are rare clinical presentations.50.51. and 52. Metastases have also been reported in an area of radiation dermatitis. 53
There are three clinical patterns of metastasis which are almost exclusively related to carcinomas of the breast: carcinoma erysipelatoides (‘inflammatory carcinoma’), carcinoma telangiectaticum, and carcinoma en cuirasse.19.54.55.56.57.58. and 59. The inflammatory pattern presents as a large, tender, warm plaque which may resemble erysipelas.17.54. and 60. It is found in less than 2% of all breast carcinomas. Some would regard this as being due to direct extension from the underlying carcinoma, and not a true metastasis. 16 Rarely, this pattern is seen with metastases from melanoma61 and mesothelioma, 62 and from carcinomas of the esophagus, 63 stomach, 64 pancreas, 65 colon,58. and 66. rectum,67. and 68. prostate, 55 bladder, 69 and lung.35. and 70. It follows the obstruction of lymphatics at all levels of the dermis, with resulting edema. 60 There are often some perivascular and perilymphatic inflammatory cells. Carcinoma telangiectaticum presents as a telangiectatic sclerotic plaque, often studded with pink papules and pseudovesicles.54. and 71. There is massive subepidermal edema resulting from obstruction by tumor of small blood vessels and lymphatics in the upper dermis. Other vessels are congested. Rarely, metastases from the lung will give this picture. Carcinoma en cuirasse is a diffuse induration of the breast resulting from some dermal fibrosis and a diffuse infiltrate of tumor cells between collagen bundles, sometimes in an ‘Indian-file’ pattern. 54
Metastases tend to occur on the cutaneous surfaces near the site of the primary tumor, although there are many exceptions. 6 Metastases from tumors of the lung often involve the chest wall and proximal parts of the upper extremities, whereas those from the oral cavity and esophagus may metastasize to the head and neck, and those from the gastrointestinal and genitourinary systems to the abdominal wall.23. and 72. Approximately 5% of metastases involve the scalp.6.11. and 73. This is a common site for metastases from the thyroid. 74 In a series of 398 Taiwanese patients with malignant cutaneous tumors of the scalp, metastatic tumors accounted for 51 of these cases; 18 of these 51 cases were from the lung. 75
Metastasis to the umbilicus is also quite common.76. and 77. The lesion that results has been called the Sister Mary Joseph nodule, in recognition of a nursing superintendent at the Mayo Clinic, Rochester, Minnesota, who is credited with recognizing the clinical significance of these nodules. 77The underlying primary tumor is usually an adenocarcinoma of the stomach, large bowel, ovary, pancreas, gallbladder, endometrium, or breast (Fig. 39.1).76.77.78.79.80. and 81. Rare primary tumors have included transitional cell carcinoma of the bladder, 82 a peritoneal mesothelioma, 83 a carcinoid, and a leiomyosarcoma of the intestine. In one case the umbilical tumor resembled an ovarian serous papillary tumor, but no ovarian tumor was ever found. 84 Other rare sites are listed in the review of all cases reported between 1960 and 1995. 85 Leukemia cutis rarely presents in this way. 86 Sister Mary Joseph nodules are usually solitary and firm, sometimes with surface fissuring. In 12 of a series of 85 cases reported in 1984, the umbilical nodule was the initial presentation of the tumor. 77 There are various routes by which tumor cells can reach the umbilicus. They include contiguous extension and spread by lymphatic and venous channels, often associated with embryological vestiges in this region. 77
Umbilicus: Sister Joseph’s nodule. The dermis is replaced by metastatic carcinoma of ovarian origin. (H & E)
The penis may be the site of metastases from the bladder and prostate.87. and 88. The deposits are usually multiple and sometimes associated with priapism. 87 Metastatic tumors involving the vulva are rare, although 66 cases were reported from one institution (the M.D. Anderson Cancer Center) in 2003. 89 In 29 cases the site of origin was non-gynecological, while in 31 cases the primary was in a gynecological site, 15 of these being in the cervix. The primary site was unknown in six cases. 89
The lower extremities, excluding the thighs, are uncommonly involved with metastases. 11 Other rare sites include the nail bed,90. and 91. thumb, finger, 92 big toe, 93 scrotum, eyelid, eyebrow, nasal tip, and ear.2.5.94.95.96. and 97.
Cutaneous metastases may develop at the site of a surgical or diagnostic procedure.2.98.99. and 100. Metastases are sometimes seen in abdominal, perineal, mastectomy, and nephrectomy scars, around colostomy sites, and along the tract produced by a thoracentesis needle. However, seeding along the needle tract is unexpectedly rare following percutaneous biopsy of prostatic carcinomas. 101 Metastases to soft tissue are beyond the scope of this book. 102
The detailed studies of Brownstein and Helwig (1972) have provided valuable information regarding the most frequent sites of origin of the tumors that give rise to cutaneous metastases. 72 They studied 724 patients in whom there was histopathological confirmation of both the primary tumor and the secondary deposit in the skin. Their studies complement the earlier report by Gates in 1937. 94
The most frequent primary tumors in men were carcinoma of the lung (24%), carcinoma of the large intestine (19%), melanoma (13%), and squamous cell carcinoma of the oral cavity (12%). 72 In women, they were carcinoma of the breast (69%), carcinoma of the large intestine (9%), melanoma (5%), and carcinoma of the ovary (4%). 72 A study from India in 1988 showed that the lung and esophagus were the most common sites of the primary tumor in men and the breast and ovary in women. 105 Breast cancer and melanoma were the most common origins for skin metastases in the study of 4020 patients with metastatic carcinoma, 6 a finding repeated in a recent report from Spain. 22 A study in 2004 from a large Veterans Administration hospital in the United States showed that the lung, melanoma, and gastrointestinal tract were the three most common primary sites of cutaneous metastases. 106
Sometimes, despite exhaustive investigations, no primary lesion can be identified. 107 This may result from an extremely small primary tumor or its regression.
The development of cutaneous metastases is usually a grave prognostic feature, as dissemination to other organs has usually already occurred. The average survival time after the appearance of cutaneous metastases is 3–6 months, 23 although this has improved slightly in recent times. 6 However, there are many reports of patients with carcinoma of the breast, neuroblastoma, and other tumors15 who survived many years after the appearance of the cutaneous metastases.
More than 60% of metastases are adenocarcinomas, usually arising in the large intestine, lung, or breast.6.17. and 23. If the glandular structures are well differentiated, the colon or rectum should be suspected as the primary site. Tumors from the breast usually have a very undifferentiated pattern, with sheets of cells or sometimes columns between the collagen bundles. Signet-ring cells can be found in some metastases of mammary origin, but they are more usual in secondary deposits of gastric origin. 108
About 15% of metastases are of squamous cell type. They usually arise from the oral cavity, lung, or esophagus. The remainder of cutaneous metastases are melanomas, anaplastic tumors, or other rare specific patterns. 109
Metastases usually resemble the primary tumor, although the features are sometimes more anaplastic. 23 The metastases from a clear cell renal cell carcinoma can appear disarmingly benign: 110 a mistaken diagnosis of a benign appendage tumor may be made in these circumstances (Fig. 39.2). Clear cell hidradenoma shows a vesicular to finely vacuolated cytoplasm, in contrast to the sometimes granular cytoplasm seen in renal cell carcinoma. 109
Metastatic renal cell carcinoma in the skin. A mistaken diagnosis of eccrine hidradenoma is sometimes made in such a case. (H & E)
Metastases are centered on the dermis, although there is sometimes extension into the subcutis. The epidermis is usually intact, and there is an underlying narrow zone of compressed collagen separating the tumor from the epidermis (grenz zone). Occasionally a metastatic squamous cell carcinoma will touch the undersurface of the epidermis, making distinction from a primary carcinoma difficult. 111 Epidermotropic metastases are exceedingly rare, except for cutaneous melanomas. 112 Dermal sclerosis is uncommon, but can be seen with some breast carcinomas.
Lymphatic permeation is a prominent feature of the so-called ‘inflammatory carcinomas’ (see p. 928). It is sometimes present at the edge of a cutaneous metastasis. Uncommonly, lymphatic channels throughout the dermis are involved (Fig. 39.3 and Fig. 39.4).
Metastatic adenocarcinoma with widespread lymphatic permeation. (H & E)
Lymphatic permeation in another case of metastatic adenocarcinoma. (H & E)
Immunohistochemistry is of increasing value in the interpretation of cutaneous metastases.109. and 113. Monoclonal antibodies against thyroglobulin, calcitonin, prostatic antigens, leukocyte common antigen (CD45), epithelial membrane antigen, S100 protein, neuron-specific enolase, various cytokeratins, vimentin, and desmin can be used to elucidate or confirm the nature of the primary tumor that gave rise to the cutaneous metastasis. A truncated immunohistochemical battery using CK7, CK20, and S100 protein has been recommended as a starting point in the assessment of a suspected cutaneous metastasis; 106 often they need to be combined with other markers. 114 A different panel, including p63, B72.3, calretinin, and CK5/6 has been used to differentiate metastatic carcinoma from primary skin adnexal tumors. 115 The majority of primary adnexal tumors express p63 whereas cutaneous metastases from internal adenocarcinomas are usually negative.116.117. and 118. In a more recent study p63 was positive in 5 of 45 (11%) cutaneous metastases. 119 This investigative field is expanding rapidly, with many new markers appearing.
The anterior chest wall is commonly involved by recurrences of carcinoma of the breast, although distant cutaneous metastases are uncommon.120. and 121. In his review of cutaneous metastases, Rosen mentions two autopsy series of carcinoma of the breast where cutaneous metastases were found in 18.6% and 37.7% of cases, respectively. 2 Brownstein and Helwig, in their study of 724 patients with cutaneous metastases, recorded 168 cases in women with carcinoma of the breast (69% of the total number of women in the series) and 9 in men. 72 In 20 of these there were single distant metastases; in 3 there were multiple metastases. 72 In the remainder, only the chest wall was involved. Extensive cutaneous metastases are sometimes observed with carcinoma of the breast, in both males and females.122.123.124. and 125.
The scalp is a favored site of distant metastases, 120 but the thigh may also be involved. 126 Patches of alopecia resembling alopecia areata (alopecia neoplastica) may result.26.27.28.127.128.129.130. and 131. Other clinical patterns found on the chest wall include the so-called ‘inflammatory carcinoma’,55.56.57.58. and 132. carcinoma telangiectaticum, 133 and carcinoma en cuirasse.54.134. and 135. Pigmented metastases mimicking malignant melanoma have also been reported.136. and 137. Prolonged survival has been recorded after the appearance of the cutaneous lesions.128. and 138.
Carcinoma of the inframammary crease is an uncommon but distinctive pattern of presentation which results from early invasion of the skin by a peripherally situated tumor.139. and 140. It is exophytic and fissured and may simulate a primary epidermal tumor both clinically and microscopically. 141
The histopathology is usually that of a poorly differentiated adenocarcinoma (Fig. 39.5). There may be sheets or large clusters of tumor cells in the dermis. Sometimes the cells are in linear array between the collagen bundles, resulting in an ‘Indian-file’ pattern. 72 Rarely, the cells resemble those seen in a granular cell tumor142 or have a sarcomatous appearance. 143 Lymphatic permeation may be prominent, particularly in those with an inflammatory or telangiectatic clinical pattern. 132 Prominent epidermotropism has been reported; the pattern mimicked Paget’s disease and melanoma.144. and 145. Sclerosis of dermal collagen is sometimes present, particularly in the scalp lesions associated with alopecia neoplastica. 27 Rarely, intraepidermal vesicles form, secondary to prolonged lymphatic obstruction. 145 Tumor cells have been seen in these vesicles. 146
Metastatic carcinoma of breast origin. The tumor cells are arranged in an ‘Indian-file’ pattern. (H & E)
Occasionally only scattered small tumor cells are present in the dermis, and these cells may be difficult to distinguish from inflammatory cells. 72 Epithelial membrane antigen, cytokeratin 7 (CK7), and some newer mammary specific antigens are detectable on these cells by immunoperoxidase methods. Gross cystic disease fluid protein-15 (GCDFP-15), estrogen receptor, and progesterone receptor proteins are valuable markers for cutaneous metastatic breast carcinoma when used in combination.145.147. and 148. In one series of cutaneous metastases from breast cancers the following profiles were obtained: CK7 (66%), CK19 (91%), ER (50%), PR (42%), CEA (73%), E-cadherin (55%), and Ber-EP4 (27%). 148 All metastases were negative for CK20, CK5/6, CD10, and TTF1. 148 It should be remembered that an occasional carcinoma of the breast will have S100-positive cells or contain melanin pigment, 149 which could lead to a mistaken diagnosis of malignant melanoma. Breast cancer cells strongly express cathepsin B. 150 A summary of the immunohistochemical profile is presented in Table 39.1. Metastasis to a benign intradermal nevus has also been reported. 103
Cutaneous metastases are found in 4% or less151 of patients with carcinoma of the lung. In a small number of cases these are precocious metastases. 14 The chest wall and abdomen are the usual sites, although ‘oat-cell’ (small cell) carcinomas appear to have a predilection for metastasizing to the back. 18 The finger and skull are extremely rare sites.152. and 153. Rarely, an inflammatory or zosteriform pattern is produced. Death usually occurs within 3 months of the development of the skin lesions. Eyelid edema, secondary to superior vena cava syndrome, can be the presenting sign of a primary bronchogenic carcinoma. 154 The histopathological pattern is squamous cell carcinoma in 40%, adenocarcinoma in 20%, and undifferentiated carcinoma in 40%.18.155. and 156. One bronchiolar and one mucoepidermoid bronchial carcinoma were among the tumors of lung reported by Brownstein and Helwig in their review on cutaneous metastases. 72 Fetal adenocarcinoma of the lung with preceding cutaneous metastasis, and basaloid carcinoma of the lung presenting concurrently with cutaneous metastasis have been reported.157. and 158. Pleural mesotheliomas rarely metastasize to the skin.62.159.160.161. and 162. Metastasis to the lip was the initial presentation of mesothelioma in two cases. 163 The cells stained with cytokeratin (CK) 5/6, epithelial membrane antigen (EMA), HBME1, calretinin, and CK7. 163
Tissue-specific transcription factor (TTF1), expressed in epithelial cells of thyroid and lung, is often expressed in cutaneous metastases of lung tumors. 148 It is not present in Merkel cell carcinomas. The immunohistochemical profile of lung metastases is shown in Table 39.2.
Tumors of the oral cavity usually spread to the face or neck. 72 In some instances this results from direct extension of the tumor rather than true metastasis. 16 The tumors are usually squamous cell carcinomas.
Less than 2% of esophageal carcinomas metastasize to the skin. 18 The primary lesion is usually a squamous cell carcinoma in the lower esophagus; 18 metastatic adenocarcinoma is sometimes seen.164. and 165. The metastases are multiple nodules with a predilection for the upper part of the trunk and the neck. Acral metastases, and metastases to the breast, masquerading as an inflammatory breast carcinoma have been recorded.63. and 166. Squamous cell carcinomas of the esophagus are usually CK5/6 positive. 148
Brownstein and Helwig reported 29 cases of gastric carcinoma with metastasis to the skin. 72 The trunk, particularly the umbilical area, is a favored site.77.167. and 168. The tip of the finger,92. and 169. the face, 170 the axilla, 171 and a congenital nevus on the occiput104 are uncommon sites of involvement. The tumors are usually poorly differentiated adenocarcinomas. Signet-ring cells and extracellular mucin pools may be present. 170 Eczematous and erythematous lesions on the face, resulting from cutaneous metastases, have also been reported.172. and 173. A monoclonal antibody HIK1083 specific for gastric O-glycan can be used in differentiating a cutaneous metastasis of gastric carcinoma from primary sweat gland carcinoma in which it is negative. 174 This stain is superior to CK20, which while often present in metastatic carcinomas of skin, is also found in metastatic colorectal cancer and occasional metastases from the lung and breast. 174
The colon is a common source of cutaneous metastases. Brownstein and Helwig recorded 90 males and 22 females in this category. 72 This makes it the second most common primary site in both males and females. Brady et al reported a 3.5% incidence of cutaneous metastases in patients coming to autopsy with adenocarcinoma of the colon and rectum. 18 The metastases are usually multiple and metachronous, and most often are in the skin of the abdominal wall or perineal region.18.68. and 72. The umbilicus, or the colostomy site, may be involved.77.175.176. and 177. The appearance of multiple metastases is a bad prognostic sign. The deposits are usually composed of well-differentiated adenocarcinoma, although mucinous, less well-differentiated variants are found. The metastases are typically ‘dirty’, with some neutrophils and degenerate cells in the lumina of the glands (Fig. 39.6).
Metastatic colonic adenocarcinoma. This nodule from the eyelid shows a metastatic adenocarcinoma with luminal necrotic material and debris (‘dirty necrosis’). (H & E)
The immunohistochemical profile of gastrointestinal metastases is listed in Table 39.3.
Cutaneous metastases occur in nearly 3% of patients with malignant hepatomas of the liver.179.180. and 181. Rarely, it is the presenting manifestation,182. and 183. although death still follows in several weeks. 180 A 12-year-old child with cutaneous metastases on the thorax and epigastrium has been reported. 184 In another case, a metastasis to the gingiva mimicked a pyogenic granuloma. 185 The histopathological pattern may be either a cholangiocarcinoma or a hepatocellular carcinoma.180.186.187.188. and 189. A sarcomatoid carcinoma is extremely rare. 190 An immunohistochemical marker of hepatocellular differentiation is now available for use on paraffin sections (Hep Par 1). 191
Brownstein and Helwig recorded 15 cases of metastatic pancreatic carcinoma involving the skin. 72 The umbilicus is a favored site for these metastases.76.192.193. and 194. Rarely, an inflammatory or epidermotropic pattern is present.65.195. and 196. Metastasis to the skin from a vasoactive intestinal polypeptide tumor (VIPoma) of the pancreas has been reported. 197
Metastases have been reported in the skin in from 2.8% to 6.3% of renal carcinomas. 18 They accounted for 6% of the cutaneous metastases in males, and 0.5% in females, in the series of Brownstein and Helwig. 72 As such, they rank after breast, lung, gastrointestinal tract, and melanoma in order of frequency. 72 The metastases are solitary in from 15% to 20% of cases.91.110. and 202. The head, particularly the scalp, is a common site of involvement.110.202. and 203. They may also be found in nephrectomy scars and the external genitalia. 202 The metastases are sometimes precocious. Metachronous metastases usually appear within 3 years of the nephrectomy, 72 although an interval of 23 years has been recorded. 110 The deposits can be quite vascular, and even resemble a pyogenic granuloma204 or Kaposi’s sarcoma. 205
Most cases are clear cell renal cell carcinomas in which the cells contain considerable glycogen and some fat (Fig. 39.7).110. and 206. Mitoses are sparse. There is usually extravasation of blood, with subsequent deposition of hemosiderin in the stroma. Metastasis to the skin of a transitional cell carcinoma of the renal pelvis,207. and 208. and of a Wilms’ tumor is occasionally reported. 110
Metastatic renal cell carcinoma. The inset shows the tumor cells in more detail. (H & E)
A renal cell carcinoma marker (RCC-Ma), a monoclonal antibody to a proximal tubule antigen, is positive in nearly two-thirds of cutaneous metastases of renal cell carcinomas. 209 It is highly specific for this tumor and is not expressed by other clear cell tumors of the skin. 209 The cells often express epithelial membrane antigen. 210 Less than 10% of conventional renal cell carcinomas express CK7 or CK20. 211 The immunohistochemical profile of renal metastases is shown in Table 39.4.
Cutaneous metastases from carcinomas of the urinary bladder are rare,82.212. and 213. ranging from 0.18%214 to 1.8%. 18 Brownstein and Helwig reported only 10 cases in their review of 724 patients with cutaneous metastases. 72 The urethra is more rarely the primary site.212. and 215. Most patients die within months of the diagnosis of a skin metastasis. 216
Metastases from the bladder are usually multiple and at a single site. 18 When solitary, they may be confused with primary skin cancers. 217 The upper extremities, trunk, abdomen, scrotum, and penis are the usual sites.186. and 212. Rarely, they are zosteriform or herpetiform in distribution.218. and 219. The tumors are transitional cell carcinomas or anaplastic carcinomas which may show areas of squamous differentiation. 215
Immunohistochemistry is positive for the cytokeratin markers CK7, CK19, and CK20. Nearly half of transitional cell carcinomas are also CK14 positive. 220
In one study of 321 metastatic lesions in 176 autopsy cases of carcinoma of the prostate, 4 lesions metastatic to the skin were found. 221 Brownstein and Helwig recorded only 5 cases in their large series. 72 The metastases are usually firm violaceous nodules, although unusual clinical patterns87 such as Sister Mary Joseph nodules (see p. 928),77.222. and 223. penile deposits,87.88.224.225. and 226. metastasis to a gynecomastic breast, 227 a zosteriform pattern, 34 and a nodule simulating a sebaceous cyst33 or an angiosarcoma228. and 229. have been recorded. Most metastases are in the inguinal region230 but other sites have been reported. 231 The primary tumor is usually an adenocarcinoma,232. and 233. but one transitional cell carcinoma has been documented. 234 Immunoperoxidase staining for prostate-specific antigen is a useful technique for confirming the prostatic origin of these metastatic adenocarcinomas.235.236. and 237.
There are several reports of cutaneous metastases from testicular tumors. 238 The histopathological pattern has included seminoma, 238 teratocarcinoma, 239 and choriocarcinoma.23.240.241. and 242. There is one report of cutaneous metastases in the suprapubic region from an adenocarcinoma of the rete testis. 243 Primary cutaneous germ cell tumors of the skin and subcutis are exceedingly rare. Only two cases have been reported in adults, although a few more have been reported in young children. 244
Squamous cell carcinomas of the penis rarely give rise to cutaneous metastases. 17
Cutaneous metastases are found in approximately 2% of patients with fatal ovarian carcinoma. 18 Brownstein and Helwig recorded 10 cases, which represents 4% of the cutaneous metastatic lesions in females. 72 There are usually multiple nodules at a solitary site on the chest or abdomen. The umbilicus and thighs may be involved.245. and 246. The pattern is usually that of a well-differentiated adenocarcinoma, sometimes having a papillary configuration with psammoma bodies. 72 A carcinoma of mucinous pattern and a Brenner tumor247 have also been reported. Paraneoplastic associations such as dermatomyositis may be a presenting sign of ovarian carcinoma. These associations were reviewed in 2008. 248 Ovarian tumors are usually CK7 positive and CK20 negative, but some mucinous ovarian tumors may be CK20 positive.114. and 249.
Cutaneous metastases are unusual in carcinoma of the cervix97.250.251. and 252. and uterine body,253.254.255.256. and 257. even in the terminal phases.258. and 259. They usually involve the lower abdomen, groin, upper thighs,260. and 261. or umbilicus,77.245.254.262. and 263. but a case metastatic to the scalp producing alopecia neoplastica, and another metastatic to the face producing a cellulitis-like picture, have been reported.30. and 264. Epidermotropic metastases to the lower abdominal wall, mimicking Bowen’s disease, have been reported from a squamous cell carcinoma of the cervix/vagina. 265 Endometrial tumors are adenocarcinomas253 or, very rarely, a mixed mullerian tumor, 266 whereas those from the cervix may be squamous cell carcinomas,250. and 260. adenosquamous carcinomas21. and 23. or, rarely, neuroendocrine in type.267. and 268. In a review of the literature of genital carcinomas with metastases to the umbilicus, Galle recorded 18 of ovarian origin, 12 from the uterine body, one squamous cell carcinoma from the cervix, and 2 adenocarcinomas from the fallopian tube. 245 There is one report of cutaneous metastases from an adenocarcinoma of the vulva. 269 Squamous cell carcinoma of the vagina rarely causes a cutaneous metastatic deposit.270. and 271. Metastasis to the vulva also occurs (see above). 89
Skin metastases are an unfavorable prognostic sign in gestational trophoblastic disease. They occur only in association with widespread disease.272. and 273. Gluteal metastases, 274 and a solitary nodule in the scalp275 have been reported. There have been several cases of placental choriocarcinoma metastasizing to the skin of a neonate. 276 The histopathology is usually similar to the primary lesion, with large syncytial trophoblastic cells and much hemorrhage. 275 Chorionic gonadotrophin can be demonstrated using immunoperoxidase techniques.
Cutaneous metastasis of thyroid carcinoma is a rare event; 277 Brownstein and Helwig recorded only 4 cases. 72 In one autopsy study, cutaneous metastases were noted in 2 of 12 medullary carcinomas and 4 of 12 giant-cell carcinomas. 278 Rarely, follicular, Hürthle cell, papillary and spindle-cell patterns are encountered.15.277.279.280.281.282.283.284.285.286. and 287. In a review of 43 patients with skin metastases from thyroid carcinoma, a papillary carcinoma was the most common (41%), followed by follicular (28%), anaplastic (15%), and medullary (15%) carcinomas. 74 The scalp was the most common site of metastasis. 74
A skin nodule may be the presenting sign of the disease. 15 An unusual presentation in one case was the development of multiple pulsatile nodules on the face, suggesting Kaposi’s sarcoma. 288 Carcinoma erysipeloides is another rare clinical presentation. 289 Long survival has been reported after the development of cutaneous metastases, 15 although the average survival in one series was 19 months. 74 Immunoperoxidase methods can be used to demonstrate calcitonin in medullary carcinomas,290. and 291. and thyroglobulin in papillary, follicular and some anaplastic tumors.280.281.287. and 292.
Cutaneous carcinoid tumors may be derived from the bronchus,293.294. and 295. stomach, 296 small bowel, appendix, and large bowel.297.298. and 299. The bronchus is the most common primary site. Several cases purporting to be primary cutaneous carcinoids have now been reported;297.300.301. and 302. they appear to behave in a benign fashion. 303 A cutaneous metastasis from an occult primary lesion must be excluded before accepting a case as a primary carcinoid of the skin. 304 Metastases from non-cutaneous tumors are usually multiple, and on the trunk. 293 Solitary,294. and 298. umbilical metastases305 and precocious metastases306 have been recorded. The carcinoid syndrome may be present.307. and 308. Its cutaneous features include flushing, rosacea, and scleroderma. 309 Pellagra is a not uncommon cutaneous manifestation of the carcinoid syndrome, although it is not specifically related to the presence of cutaneous metastases.309. and 310.
Carcinoid tumors are composed of solid islands and nests of uniform cells (Fig. 39.8). 305 Thin collagenous septa extend between the tumor nests. A mucinous stroma was present in one purported case of a primary lesion. 301 In one case, the cutaneous metastasis mimicked a primary adnexal poroid neoplasm. 311 The cells may be argentaffin positive if the primary lesion is in the small or large intestine. Cutaneous metastases of bronchial carcinoids are often devoid of both argyrophil and argentaffin granules. The cells in carcinoid tumors are positive for neuron-specific enolase, and often chromogranin and synaptophysin as well. The cells are negative for CK5/6, CK7, CK20, and p63. 311 Dense-core granules can be seen in the cytoplasm on electron microscopy. 294
Metastatic carcinoid of the scalp. A primary lesion was found in the terminal ileum some months later. (H & E)
Neuroblastomas are the most common tumors of childhood.20.312.313.314.315.316. and 317. Whereas cutaneous and subcutaneous metastases are found in only 2.6% of cases of neuroblastoma of all ages, they are found in 32% of neonatal tumors. 317 Cutaneous nodules may be the presenting sign of neonatal neuroblastoma.313. and 318. They characteristically blanch on pressure.312. and 314. The pattern of cutaneous metastases may sometimes resemble that of the ‘blueberry muffin baby’, which is more usually associated with the congenital rubella syndrome. 315
The findings are typical of neuroblastoma, with small cells with hyperchromatic nuclei and rosette formation. 316 The cells stain for neuron-specific enolase by immunoperoxidase methods.
Paradoxically, stage IV-s disease in neonates, in whom there is remote spread of tumor to the liver, skin, and bone marrow, has a relatively good prognosis. 312 The tumor may remit or transform spontaneously into a benign ganglioneuroma. With more aggressive treatment protocols, the prognosis is now better than in some of the earlier series of neonatal neuroblastomas. 317
The skin and subcutaneous tissue are common sites of metastases in melanoma.6.319. and 320. Often they are the first site to become involved. 321 There is great variability in the incidence reported in the literature, which reflects in part the different criteria used for inclusion of cases. Local and in-transit (see below) cutaneous metastases are specifically excluded in some series.321. and 322. Metastases to the skin have been present at autopsy in from 10% to 75% of patients with fatal melanoma.323.324. and 325. It has been the site of the first metastasis in from 6% to 22% of cases.321. and 322. Late metastases are rare, 326 but as Carlson has pointed out, melanomas with slow tumor doubling times may give rise to late metastases. 327 It has been stated that in nearly 5% of patients a metastasis is the initial presentation of the disease, and no primary lesion can be found.328. and 329. In the author’s experience it is less than 0.5%. Usually these individuals present with a lymph node metastasis, but sometimes it is in the skin. 328 Brownstein and Helwig reported 75 cases of metastatic melanoma in the skin, making melanoma the third most common source of cutaneous metastases. 72 In a recent report (2005), five cases of completely regressed primary cutaneous melanomas with nodal and/or visceral metastases were reviewed. 330
Recently, DNA microarray technology has been used to study gene changes in melanoma cells in cutaneous metastases. There is significant up-regulation of several mitogen-activated protein kinase genes in melanoma metastases. 331
A distinct pattern of cutaneous metastasis which is almost unique to melanoma is the development of multiple small nodular deposits, often on a limb, between the site of the primary lesion and the regional lymph nodes. 332 These in-transit metastases probably originate from cells trapped in lymphatics. 333 The nodules are bluish, black, or pink in color, 332 and are small and painless. Larger lesions may ulcerate.
Rare clinical presentations have included inflammatory metastases,61. and 334. a pattern resembling Kaposi-like angiodermatitis due to lymphatic spread, 335 a hematoma-like lesion, 336 a pedunculated tumor, 337 a zosteriform distribution,38.338. and 339. a miliary pattern, 340 metastasis to the breast, 341 and diffuse melanosis.342.343.344. and 345. Vitiligo is an uncommon finding in metastatic melanoma. 346 Hypercalcemia from bone marrow involvement has also been reported. 347 Although widespread cutaneous metastases are usually a bad prognostic sign, some patients with in-transit metastases localized to a limb can survive for many years. In one study, a positron emission tomography (PET) scan had low sensitivity in detecting metastases. 348
Long-term complete remission of cutaneous melanoma metastases has been reported in a patient using a folk remedy consisting of the ingestion and application of the plant Thymus vulgaris (thyme). 349 Topical imiquimod has also been used with success in one case. 350 The use of anti-tumor necrosis factor therapies may lead to reactivation of latent melanoma metastases. 351
There is usually no difficulty in diagnosing cutaneous metastatic deposits, although the rare signet-ring cell melanoma may cause problems. 352 They differ in many instances from a primary lesion by the absence of junctional activity and an inflammatory infiltrate. 353 Occasionally lymphatic or vascular permeation is present. 354 Angiotropism may be a clue to the diagnosis of an epidermotropic metastatic melanoma. 355 Invasion between collagen bundles in the reticular dermis or into fat lobules of the subcutis, accompanied by incorporation of host stroma islands into the tumor bulk, is associated with a bad prognosis.356. and 357.
Uncommonly, cutaneous metastases are epidermotropic with nests of tumor cells in the junctional zone and within the epidermis itself.319.358.359.360. and 361. The criteria originally suggested for an epidermotropic metastasis358 are no longer regarded as diagnostic (see p. 747).
The immunophenotype of metastatic melanomas usually differs from primary tumors. The expression of Ki-67 and mutant p53 protein is usually higher in metastatic tumors than in primary lesions and CD117 is usually lost in metastatic lesions (except from an ocular primary) but present in cutaneous primary lesions. 362 If melanin pigment is absent from the deposit, the diagnosis can be confirmed by immunoperoxidase studies for S100 protein, melan-A, or HMB-45. The occasional finding of S100 protein in metastases of mammary carcinoma has already been mentioned. Loss of S100 protein staining, or all three markers, has been recorded in metastatic melanoma.363. and 364.
Rare primary lesions that have been known to metastasize to the skin include an adenoid cystic carcinoma, an acinic cell carcinoma, a myoepithelial carcinoma, and adenocarcinoma of the salivary gland,365.366.367.368.369. and 370. an adenoid cystic carcinoma of the lacrimal gland, 371 an ameloblastoma, 372 a thymoma, 373 an adrenal carcinoma,374. and 375. a pheochromocytoma, 376 and carcinomas of the hypopharynx, 377 nasopharynx,31.378. and 379. and larynx.380.381.382.383. and 384. Medulloblastomas,385. and 386. hemangiopericytoma, 387 and other tumors, particularly glioblastomas, rarely metastasize to the skin;388. and 389. when they do so it is usually to the scalp.390. and 391. The author has seen a retinoblastoma metastatic to the skin.
Squamous cell carcinomas of the skin may occasionally metastasize to other cutaneous sites.39.40.43. and 392. Rarely, it is zosteriform in type. 393 Metastasis from skin cancer in organ transplant recipients has a poor prognosis, particularly if the initial metastasis is distant rather than regional or in-transit. 394
Brownstein and Helwig reported 19 metastatic sarcomas in their 724 cases of cutaneous metastases. 72 A footnote in the article states that this figure ‘includes leiomyosarcoma, rhabdomyosarcoma, fibrosarcoma, chondrosarcoma, Ewing’s sarcoma, osteogenic sarcoma, and undifferentiated sarcomas’. 72 Leiomyosarcomas of the uterus,266. and 395. small intestine, 396 mesentery, 397 and colon metastatic to the skin have been recorded, as have rhabdomyosarcomas20.398.399. and 400. and fibrosarcoma and malignant fibrous histiocytoma of soft tissues and bone,21.401. and 402. a giant cell tumor of bone, 403 Hodgkin’s disease, 404 Ewing’s sarcoma,20. and 405. a chondroblastoma, 406 several cases of chondrosarcoma,407.408.409. and 410. a mesenchymal chondrosarcoma of soft tissue origin, 411 a metaplastic breast carcinoma with chondrosarcomatous features, 143 an osteogenic sarcoma (osteosarcoma),412.413.414.415.416. and 417. a paraganglioma, 418 and an angiosarcoma of the aorta419 and heart. 420 Mesotheliomas may rarely metastasize to the skin.421. and 422. Several cases of chordoma metastatic to the skin have been reported;423.424.425. and 426. direct extension to the skin is more common.427. and 428.
Finally, atrial myxomas may embolize to the skin, producing a varied clinical appearance.429. and 430. The tumor emboli, which have a characteristic myxomatous appearance, do not usually extend beyond the vessel wall (Fig. 39.9). 431
(A) Atrial myxoma in a deep dermal vessel of the finger. (B) Loose myxoid tissue is present in the lumen of a small artery. (H & E)
References
Introduction
1. Leonard, N, Cutaneous metastases: Where do they come from and what can they mimic, Curr Diagn Pathol 13 (2007) 320–330.
2. Rosen, T, Cutaneous metastases, Med Clin North Am 64 (1980) 885–900.
3. Brodland, DG; Zitelli, JA, Mechanisms of metastasis, J Am Acad Dermatol 27 (1992) 1–8.
4. Krumerman, MS; Garret, R, Carcinomas metastatic to skin, NY State J Med 77 (1977) 1900–1903.
5. Su, WPD; Powell, FC; Goellner, JR; Wick, MR, In: Pathology of unusual malignant cutaneous tumors (1985) Marcel Dekker, New York, pp. 357–397.
6. Lookingbill, DP; Spangler, N; Helm, KF, Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients, J Am Acad Dermatol 29 (1993) 228–236.
7. diSibio, G; French, SW, Metastatic patterns of cancers. Results from a large autopsy study, Arch Pathol Lab Med 132 (2008) 931–939.
8. Abrams, HL; Spiro, R; Goldstein, N, Metastases in carcinoma: analysis of 1,000 autopsied cases, Cancer 3 (1950) 74–85.
9. Freireich, EJ; Kurzrock, R; Estrov, Z, Metastasis – an alternative hypothesis, Cancer 103 (2005) 1537–1539.
10. Schwartz, RA, Cutaneous metastatic disease, J Am Acad Dermatol 33 (1995) 161–182.
Clinical and morphological features
11. Brownstein, MH; Helwig, EB, Patterns of cutaneous metastasis, Arch Dermatol 105 (1972) 862–868.
12. Lookingbill, DP; Spangler, N; Sexton, FM, Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients, J Am Acad Dermatol 22 (1990) 19–26.
13. Jevtic, AP, Skin metastasis from renal carcinoma presenting as an inflammatory lesion, Australas J Dermatol 28 (1987) 18–20.
14. Camiel, MR; Aron, BS; Alexander, LL; et al., Metastases to palm, sole, nailbed, nose, face and scalp from unsuspected carcinoma of the lung, Cancer 23 (1969) 214–220.
15. Pitlik, S; Kitzes, R; Ben-Bassat, M; Rosenfeld, JB, Thyroid carcinoma presenting as a solitary skin metastasis, Cutis 31 (1983) 532–536.
16. White Jr, JW, Evaluating cancer metastatic to the skin, Geriatrics 40 (1985) 67–73.
17. Brownstein, MH; Helwig, EB, Spread of tumors to the skin, Arch Dermatol 107 (1973) 80–86.
18. Brady, LW; O’Neill, EA; Farber, SH, Unusual sites of metastases, Semin Oncol 4 (1977) 59–64.
19. McKee, PH, Cutaneous metastases, J Cutan Pathol 12 (1985) 239–250.
20. Wesche, WA; Khare, VK; Chesney, TM; Jenkins, JJ, Non-hematopoietic cutaneous metastases in children and adolescents: thirty years experience at St. Jude Children’s Research Hospital, J Cutan Pathol 27 (2000) 485–492.
21. Taboada, CF; Fred, HL, Cutaneous metastases, Arch Intern Med 117 (1966) 516–519.
22. Marcoval, J; Moreno, A; Peyrí, J, Cutaneous infiltration by cancer, J Am Acad Dermatol 57 (2007) 577–580.
23. Reingold, IM, Cutaneous metastases from internal carcinoma, Cancer 19 (1966) 162–168.
24. Peris, K; Fargnoli, MC; Lunghi, F; Chimenti, S, Unusually large cutaneous metastases of renal cell carcinoma, Acta Derm Venereol 81 (2001) 77–78.
25. Resnik, KS; DiLeonardo, M; Gibbons, G, Clinically occult cutaneous metastases, J Am Acad Dermatol 55 (2006) 1044–1047.
26. Cohen, I; Levy, E; Schreiber, H, Alopecia neoplastica due to breast carcinoma, Arch Dermatol 84 (1961) 490–492.
27. Baum, EM; Omura, EF; Payne, RR; Little, WP, Alopecia neoplastica – a rare form of cutaneous metastasis, J Am Acad Dermatol 4 (1981) 688–694.






