Introduction370
INTRODUCTION
CALCIUM, BONE, AND CARTILAGE
CALCINOSIS CUTIS
Subepidermal calcified nodule
Idiopathic scrotal calcinosis
Tumoral calcinosis
Auricular calcinosis
Infantile calcinosis of the heel
Milia-like calcinosis
Dystrophic calcification
Metastatic calcification
Calciphylaxis
Calcification of blood vessels
Calcification of cysts and neoplasms
Histopathology
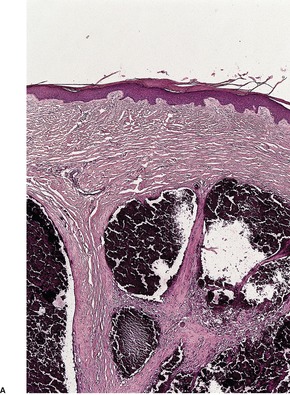
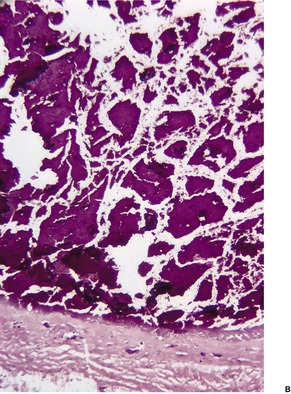
Fig. 14.1
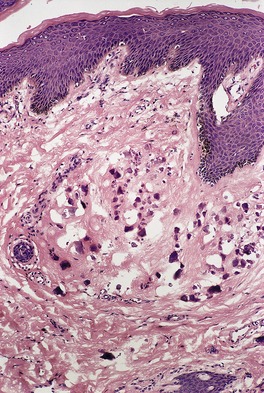
Fig. 14.2
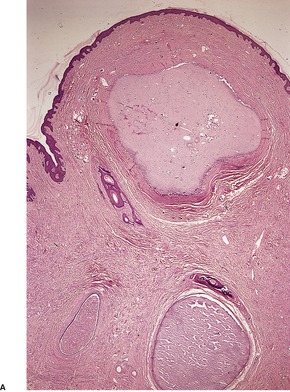
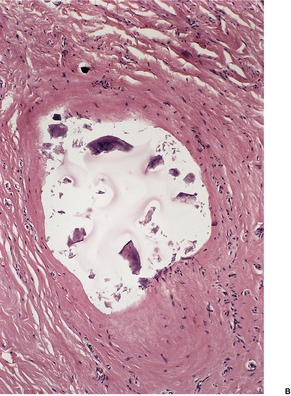
Fig. 14.3
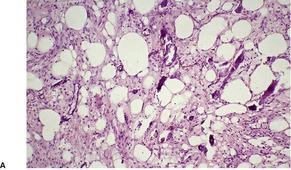
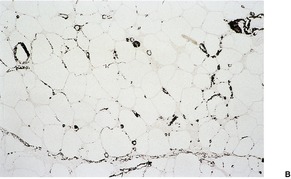
Fig. 14.4
CUTANEOUS OSSIFICATION
Multiple osteomas
Multiple miliary osteomas of the face
Auricular ossificans
Osteomas of the distal extremities
Albright’s hereditary osteodystrophy
Progressive osseous heteroplasia
Congenital plaque (plate)-like osteomatosis
Fibrodysplasia ossificans progressiva
Secondary ossification
Histopathology
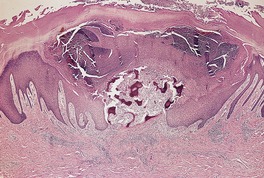
Fig. 14.5
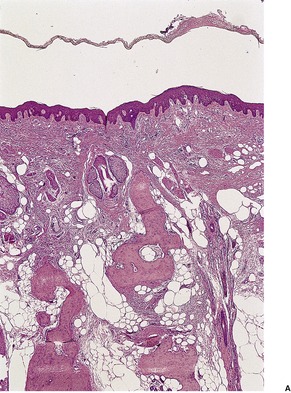
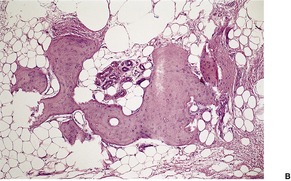
Fig. 14.6
CARTILAGINOUS LESIONS OF THE SKIN
Chondromas
Hamartomas containing cartilage
Soft tissue tumors with cartilaginous differentiation
Skeletal tumors with cartilaginous differentiation
Miscellaneous lesions
HYALINE DEPOSITS
GOUT
Histopathology
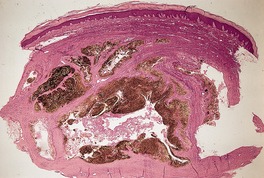
Fig. 14.7
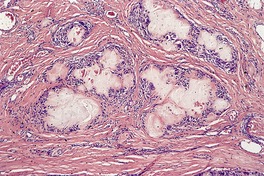
Fig. 14.8
AMYLOIDOSIS
Histochemical properties
Immunofluorescence
Ultrastructure283
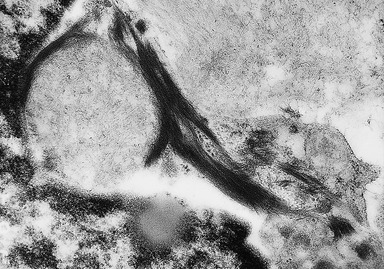
Fig. 14.9
Primary systemic amyloidosis
Histopathology
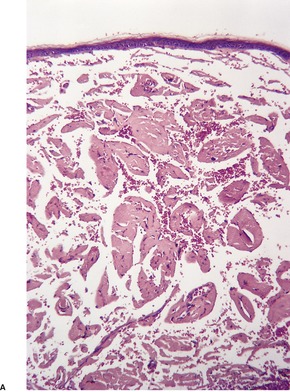
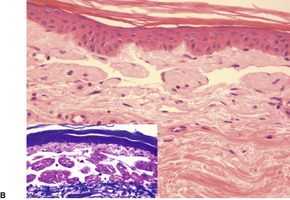
Fig. 14.10
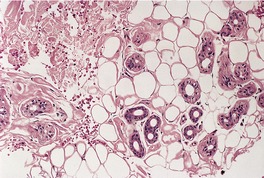
Fig. 14.11
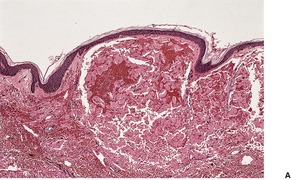
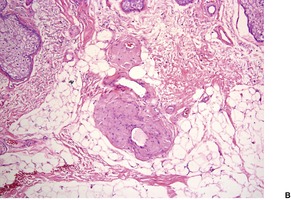
Fig. 14.12
Secondary systemic amyloidosis
Heredofamilial amyloidosis
Amyloid elastosis
Lichen, macular, and biphasic amyloidoses
Histopathology
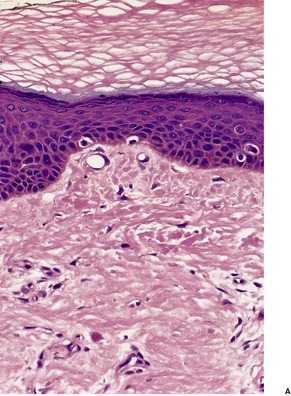
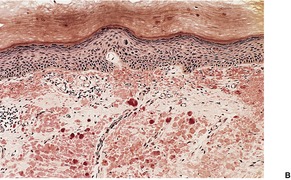
Fig. 14.13
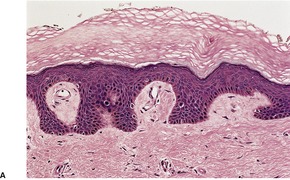
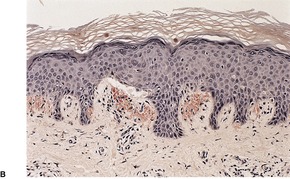
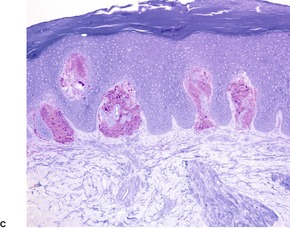
Fig. 14.14
Auricular amyloidosis

Fig. 14.15
Nodular amyloidosis
Histopathology
Poikilodermatous amyloidosis
Histopathology
Anosacral amyloidosis
Histopathology
Familial primary cutaneous amyloidosis
Secondary localized cutaneous amyloidosis
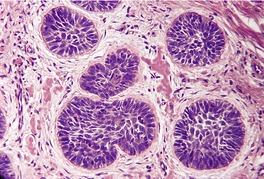
Fig. 14.16
PORPHYRIA
LIPOID PROTEINOSIS
Histopathology517. and 518.
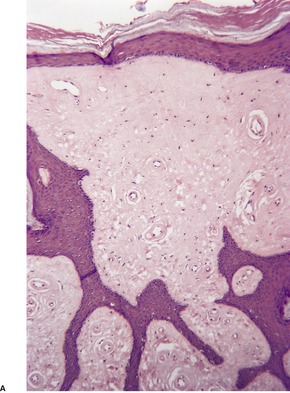
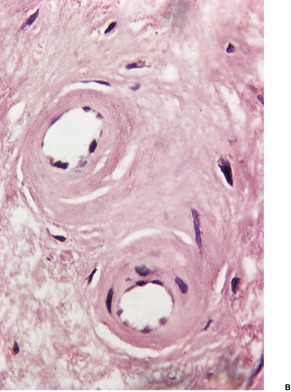
Fig. 14.17
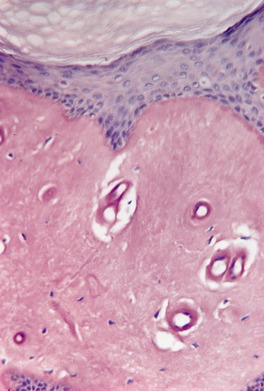
Fig. 14.18
Electron microscopy
WALDENSTRÖM’S MACROGLOBULINEMIA
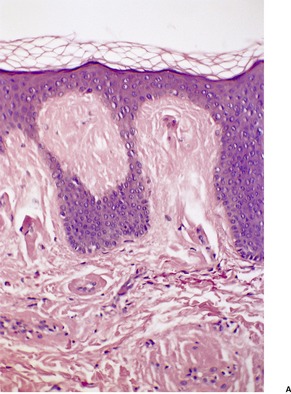
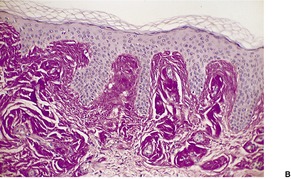
Fig. 14.19
COLLOID MILIUM AND COLLOID DEGENERATION
Histopathology
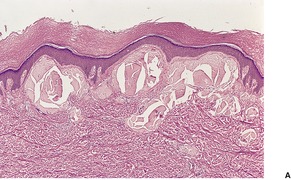
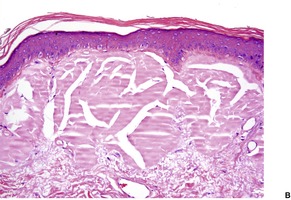
Fig. 14.20
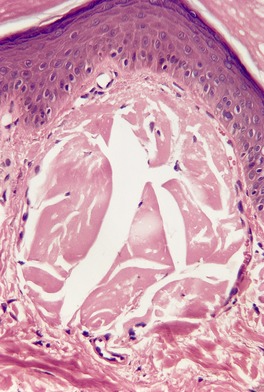
Fig. 14.21
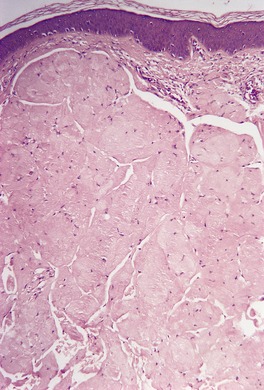
Fig. 14.22
Electron microscopy
MASSIVE CUTANEOUS HYALINOSIS
CORTICOSTEROID INJECTION SITES
Histopathology
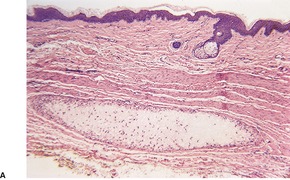
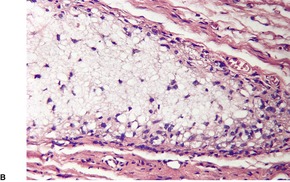
Fig. 14.23
HYALIN ANGIOPATHY (PULSE GRANULOMA)
INFANTILE SYSTEMIC HYALINOSIS AND JUVENILE HYALINE FIBROMATOSIS
Histopathology
CYTOID BODIES
Histopathology604. and 607.
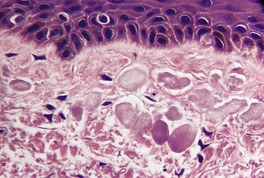
Fig. 14.24
Electron microscopy
PIGMENT AND RELATED DEPOSITS
OCHRONOSIS
Histopathology625. and 638.
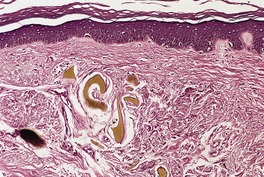
Fig. 14.25
Electron microscopy
TATTOOS
Histopathology699
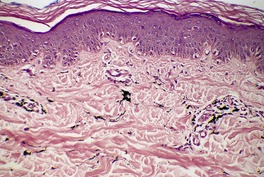
Fig. 14.26
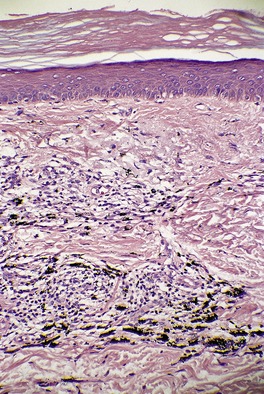
Fig. 14.27
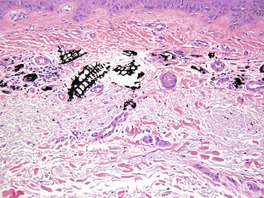
Fig. 14.28
HEMOCHROMATOSIS
Histopathology717. and 721.
HEMOSIDERIN FROM OTHER SOURCES
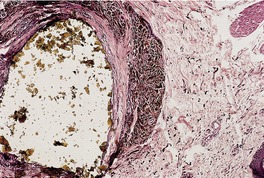
Fig. 14.29
‘BRONZE BABY’ SYNDROME
SILVER DEPOSITION (ARGYRIA)
Histopathology734
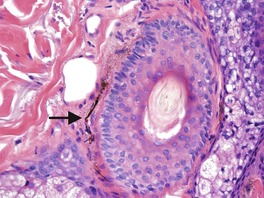
Fig. 14.30
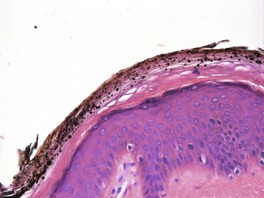
Fig. 14.31
GOLD DEPOSITION (CHRYSIASIS)
Histopathology734.765. and 771.
MERCURY
Histopathology776.786. and 788.
Electron microscopy
ARSENIC
LEAD
ALUMINUM
Histopathology796. and 803.
ZINC
BERYLLIUM
BISMUTH
TITANIUM
DRUG DEPOSITS AND PIGMENTATION
Antimalarial drugs
Phenothiazines
Tetracycline
Methacycline
Minocycline
Type I
bluish-black pigmentation of scars832. and 833. and old inflammatory foci, including sites of immunobullous diseases, 834 related to hemosiderin or an iron chelate of minocycline; a variant of this (proposed type IV), with blue-gray pigmentation of acne scars on the back was characterized by calcium-containing melanin deposits within dendritic cells and in an extracellular location. 835
Type II
blue-gray circumscribed pigmentation of the lower legs and arms due to a pigment which is probably a drug metabolite–protein complex chelated with iron and calcium. The recently reported cases with deposits of minocycline pigment localized to the subcutaneous fat of the lower extremity appear to be a different type (proposed type V).836. and 837.
Type III
a generalized muddy brown pigmentation due to increased melanin in the basal layer, and accentuated in sun-exposed areas835. and 838.
Histopathology734. and 831.
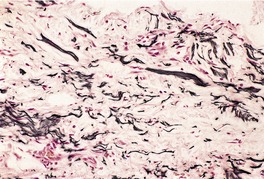
Fig. 14.32
Amiodarone
Clofazimine
Omeprazole
Chemotherapeutic agents
CUTANEOUS IMPLANTS
SILICONE IMPLANTS
Histopathology913
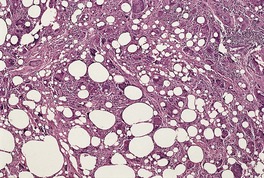
Fig. 14.33
COLLAGEN IMPLANTS
Histopathology883.925.926.927. and 928.
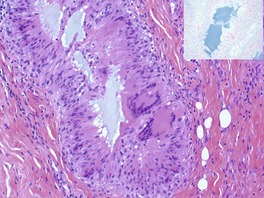
Fig. 14.34
MISCELLANEOUS DEPOSITS
OXALATE CRYSTALS
Histopathology929.930. and 933.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Cutaneous deposits
Calcium, bone, and cartilage370
Calcinosis cutis370
Subepidermal calcified nodule370
Idiopathic scrotal calcinosis370
Tumoral calcinosis370
Auricular calcinosis370
Infantile calcinosis of the heel370
Milia-like calcinosis370
Dystrophic calcification371
Metastatic calcification371
Calciphylaxis371
Calcification of blood vessels371
Calcification of cysts and neoplasms371
Cutaneous ossification372
Multiple osteomas372
Multiple miliary osteomas of the face372
Auricular ossificans372
Osteomas of the distal extremities372
Albright’s hereditary osteodystrophy372
Progressive osseous heteroplasia373
Congenital plaque (plate)-like osteomatosis373
Fibrodysplasia ossificans progressiva373
Secondary ossification373
Hyaline deposits376
Gout376
Amyloidosis376
Primary systemic amyloidosis377
Secondary systemic amyloidosis378
Heredofamilial amyloidosis378
Amyloid elastosis378
Lichen, macular, and biphasic amyloidoses380
Auricular amyloidosis381
Nodular amyloidosis381
Poikilodermatous amyloidosis382
Anosacral amyloidosis382
Familial primary cutaneous amyloidosis382
Secondary localized cutaneous amyloidosis382
Porphyria382
Lipoid proteinosis382
Waldenström’s macroglobulinemia384
Colloid milium and colloid degeneration384
Massive cutaneous hyalinosis386
Corticosteroid injection sites386
Hyalin angiopathy (pulse granuloma)386
Infantile systemic hyalinosis and juvenile hyaline fibromatosis387
Cytoid bodies387
Cutaneous deposits are a heterogeneous group of substances which are not normal constituents of the skin. They are laid down, usually in the dermis, in a variety of different circumstances. There are five broad categories of deposits (Table 14.1). The first group includes calcium salts, bone, and cartilage. 1 The second category includes the hyaline deposits. These have an eosinophilic, somewhat glassy appearance in hematoxylin and eosin preparations. The third category includes various pigments, heavy metals (many of which are deposited in the form of a pigmented salt), and complex drug pigments. The fourth category, cutaneous implants, includes substances such as collagen and silicone which are inserted into the skin for cosmetic purposes. The fifth category includes miscellaneous substances such as oxalate crystals and fiberglass.
• Calcium salts, bone, and cartilage
• Hyaline deposits
• Pigments, heavy metals, drug pigments
• Cutaneous implants
• Miscellaneous deposits
Some deposits evoke an inflammatory or foreign body reaction, although many of the hyaline and pigment deposits produce no significant response, except for some macrophages in the case of pigments. Hyaline deposits may blend imperceptibly with the surrounding collagen and require special histochemical staining for their positive identification.
The cutaneous deposition of calcium salts – calcinosis cutis – has historically been divided into a dystrophic variety, when the calcium is deposited in damaged or degenerate tissue, and a less common metastatic form associated with elevated serum levels of calcium or phosphate or both.2. and 3. In many cases, the pathogenetic mechanism is unknown and these have been assigned to a third idiopathic group. Sometimes, several mechanisms are involved in the formation of the calcium deposits.4. and 5. Rarely, no satisfactory explanation can be advanced for the calcium deposition. 6 A recent study of idiopathic cases of calcification and ossification of the skin found that bone morphogenetic protein 4, β-catenin, osteopontin, osteonectin, and osteocalcin were involved in the process; 7 it is a highly regulated one. The following classification is a modification of the historic one. 1
Subepidermal calcified nodule usually occurs as a solitary nodule on the head, particularly the ear, or the extremities of infants and young children, but it may develop in an older group of patients in whom it has a predilection for the upper extremities.8.9.10.11.12.13.14. and 15. Multiple lesions have been reported on the eyelids. 16 Mucosal lesions are rare. 17 Subepidermal calcified nodule is one of the idiopathic calcinoses, although it has been suggested that the calcification occurs in a pre-existing nevus or hamartoma. 18 There is little evidence to support this view. It has been suggested that congenital lesions occurring on the ear should be categorized as a variant of traumatic calcinosis cutis, because of presumptive in-utero microtrauma; the term congenital calcinosis cutis of the ear has also been suggested for these cases.19. and 20.
Single or multiple lesions, up to 3 cm or more in diameter, develop in the scrotal skin in children or young adults.21.22.23.24.25.26. and 27. They may break down and discharge chalky material. It has been suggested that the lesions represent dystrophic calcification of eccrine duct milia28 or of epidermal cysts,24.29. and 30. although this has been disputed.31.32. and 33. A recent study of 20 cases concluded that scrotal calcinosis results from calcification of hair follicular or epidermal cysts, but this epithelium eventually disappears and may not be seen. 34 Calcification of degenerate dartoic muscle has also been suggested as a cause. 35
Tumoral calcinosis is characterized by the presence of large, often multiple deposits of calcium hydroxyapatite that preferentially involve periarticular soft tissue on the extensor aspect of large joints.40.41.42.43.44. and 45. There is a predilection for black races. Cases involving the small joints of the hand have been described.44. and 46. In the large series of 43 cases of the distal extremities, mainly from the Armed Forces Institute of Pathology (AFIP), various predisposing conditions were identified including hyperphosphatemia, scleroderma, osteoarthritis, renal failure, and congenital deformities. 44 The etiology was indeterminate in many cases. 44
Familial cases also occur. 47 Familial tumoral calcinosis (OMIM 211900) is an autosomal recessive disorder caused by hyperphosphatemia secondary to the increased renal reabsorption of phosphate. Mutations in the GalNac-transferase-3 gene (GALNT3) on chromosome 2q24–q31 have been described.48.49. and 50. The gene product is considered important in the structure and function of the phosphaturic hormone fibroblast growth factor-23 protein (FGF23), deficiencies of which have also been associated with familial tumoral calcinosis. 50 The FGF23 gene maps to 12p13.3. Recently, a normophosphatemic variant of familial tumoral calcinosis (OMIM 610455) has been described. It is due to a mutation in SAMD9, encoding a TNF-α responsive protein. 51
Auricular calcinosis is a rare lesion of one or both ears that may be secondary to local factors such as inflammation, frost bite, or trauma or be associated with systemic diseases such as Addison’s disease, ochronosis, or hypopituitarism.54. and 55. It involves calcification of the auricular cartilage. The term ‘petrified ear’ is sometimes used.56.57.58. and 59. Ossification rarely develops in auricular calcinosis. 60 This lesion is different from the calcified nodule that is present at birth and called congenital calcinosis cutis of the ear (see above), which does not involve the cartilage.
Calcinosis of the heel has been reported in infants who received multiple heel pricks for blood tests.61. and 62. It has also been reported after a solitary episode. 63 The deposits have been recognized at 10–12 months of age and they disappear about a year later. This group should probably be regarded as a clinical variant of dystrophic calcification; the nature of the underlying damage to the dermis which leads to the deposition of the calcium salts has not been elucidated.
In dystrophic calcification there may be widespread large deposits (calcinosis universalis), such as occur in dermatomyositis73.74. and 75. and rarely in lupus erythematosus,76.77.78.79.80.81. and 82. and porphyria cutanea tarda, 83 or a few small deposits (calcinosis circumscripta), as seen in scleroderma84.85. and 86. (see p. 304). Calcinosis cutis universalis has also been reported as an idiopathic phenomenon in the absence of any underlying disease or altered calcium/phosphate levels. 87 Also included in the dystrophic group1 are the calcium deposits that are found, rarely, in burns scars, keloids, acne scars, trauma sites,88. and 89. venous ulcers, 90 radiation sites, 91 injection sites,92.93.94.95. and 96. a violin pressure point, 97 and following calcium chloride or gluconate burns or infusions98.99.100.101.102.103.104. and 105. and the use of calcium chloride-containing electrode pastes for electroencephalograms.106.107. and 108. The injection of calcium-containing heparins in patients with chronic renal failure may also result in calcinosis cutis at the injection sites.109. and 110. Cutaneous calcification of dystrophic type may follow the percutaneous penetration of calcium salts in those exposed to industrial drilling fluids containing calcium salts. 106 It has also been reported following neonatal herpes simplex infection111 and in patients with the Ehlers–Danlos syndrome (see p. 327). Widespread cutaneous calcification has been reported in pseudoxanthoma elasticum. 112 The disseminated linear lesions of calcinosis cutis that developed in an infant with congenital acute monocytic leukemia were regarded as dystrophic lesions that occurred secondary to koebnerization from scratching. 113 The dystrophic calcification of the CREST syndrome (see above) has responded to treatment with intravenous immunoglobulin. 114
Cutaneous involvement is a rare manifestation of the metastatic calcification that may accompany the hypercalcemia associated with primary or secondary hyperparathyroidism, destructive lesions of bone, 115 hypervitaminosis D, and other rare causes.5.116. and 117. It is usually a late complication of chronic renal failure. 118 The deposits are found in the deep dermis or subcutaneous tissue, particularly in the axillae, abdomen, medial aspect of the thighs, the vulva, and the flexural areas.119.120. and 121. The cutaneous calcification seen in some patients after liver transplantation is probably of metastatic type due to the large amounts of intravenous calcium needed to correct hypocalcemia following the use of blood products.122. and 123. A similar etiology may have resulted in the calcinosis cutis that developed in a patient with cystic fibrosis after double lung transplants. 124
Calciphylaxis (calcific uremic arteriolopathy) is an uncommon and often lethal variant of metastatic calcification in which calcification of the walls of small- to medium-sized vessels in the dermis and subcutis induces ischemic necrosis of the skin.125.126.127.128.129.130.131.132.133. and 134. The incidence is 4.5 per 1 million persons. 135 Its prevalence in patients on hemodialysis is 4.1%. Most cases occur in the elderly; childhood cases are uncommon. 136
It presents as painful livedo reticularis and tender erythematous plaques or nodules on the buttocks, abdomen, breasts, and the upper and lower extremities.137. and 138. The lesions may become necrotic and ulcerate.131. and 139. The penis is a rare site of involvement. 140
Most cases of calciphylaxis are associated with end-stage renal failure with secondary hyperparathyroidism,141. and 142. but it has also been associated with primary hyperparathyroidism,143. and 144. metastatic breast carcinoma,145. and 146. presumptive functional protein C and protein S deficiency induced by chemotherapy, 147 alcoholic cirrhosis,133. and 148. warfarin therapy in a diabetic patient, 149 and vitamin K therapy. 150 An idiopathic case has also been reported. 151 Obesity and systemic corticosteroids are risk factors for the development of calciphylaxis. 152
The pathogenesis of calciphylaxis is now being elucidated. 153 Recent work suggests that activation of the NFκB pathway plays an important role. Accordingly, inhibitors of the RANKL–RANK–NFκB pathway such as bisphosphonates, recombinant osteoprotegerin, and anti-RANKL antibodies may theoretically assist in the treatment of calciphylaxis. 153
The mortality rate is 60–80% and this is related to wound infection, sepsis, and organ failure. 138 Surgical debridement is associated with improved survival. 152 Other treatments that have been used include cinacalcet, 154 sodium thiosulfate,155.156. and 157. pamidronate, 158 other bisphosphonates, 159 and low-dose tissue plasminogen activator. 160
Calcification may occur in tricholemmal cysts, pilomatrixomas, trichoepitheliomas, syringomas, 165 basal cell carcinomas, and hemangiomas. 1 It is dystrophic in type. Although nanobacteria species have been implicated in the pathogenesis of urinary calculi and calcific atherosclerosis, they could not be detected in the calcification seen in tumors or tumoral calcinosis. 166
Calcium salts are easily recognized in hematoxylin and eosin sections by their intense, uniform basophilia; if necessary, their nature may be confirmed by von Kossa’s silver stain which blackens the deposits. The subcutaneous deposits found in tumoral calcinosis (Fig. 14.1) and foci of metastatic and dystrophic calcification tend to be large and dense while those found in the dermis, as in subepidermal calcified nodule, are multiple, small and globular in type (Fig. 14.2). Scrotal deposits are more or less amorphous masses (Fig. 14.3). In subepidermal calcified nodule and in milia-like calcinosis there is often overlying pseudoepitheliomatous hyperplasia, associated with transepidermal elimination of some granules. Transepidermal elimination of calcium deposits is uncommon in the other forms. 117 Foreign body giant cells and peripheral condensation of connective tissue are other features often associated with the deposition of calcium salts. Chronic inflammation is mild or absent.
(A) Tumoral calcinosis. (B) The calcium deposits are large and irregular in shape. (H & E)
Subepidermal calcified nodule. The calcium deposits are small and globular. (H & E)
(A) Idiopathic scrotal calcinosis. (B) The deposits are surrounded by hyaline fibrous tissue. (H & E)
In familial tumoral calcinosis, the initial phase is characterized by edema, collagen degeneration, mucin deposits, and hyalinization with necrosis and cyst formation. The cystic cavities are lined by osteoclast-like giant cells and mononuclear cells. Calcification then occurs, suggesting that it is a delayed response to tissue injury. 53 Furthermore, adjacent normal skin does not show any calcium deposits, which might be expected if calcification is the primary event.53. and 167. Similar stages of evolution have been reported recently in 43 cases of tumoral calcinosis-like lesions of the distal extremities in which the deposits were smaller and the etiology was varied, but not familial. 44
Epidermal and follicular calcification has been reported in the necrotic epithelium associated with toxic epidermal necrolysis in a patient who also had secondary hyperparathyroidism. 168 There were no dermal deposits of calcium present.
In calciphylaxis, there is usually epidermal ulceration, focal dermal necrosis, and vascular calcification. 169 The calcification involves small to medium-sized vessels particularly in the subcutis. Fibrin thrombi may be present in capillaries. 146 Osteopontin levels are increased at sites of calcium deposition. 170 An acute and chronic calcifying panniculitis is a common finding (Fig. 14.4). 171 Fat necrosis is often present. Calciphylaxis is often overdiagnosed on the basis of a small amount of calcification in small vessels in the subcutis. This is often just a manifestation of Monckeberg’s sclerosis in elderly patients.
(A) Calciphylaxis involving the subcutaneous fat. (H & E) (B) The small calcium deposits can be seen in vessels and thin collagenous septa. (von Kossa)
Cutaneous ossification has traditionally been classified into a primary form (osteoma cutis), where there is an absence of a pre-existing or associated lesion, and a secondary type (metaplastic ossification), where ossification develops in association with or secondary to a wide range of inflammatory, traumatic, and neoplastic processes.3. and 172. There are several distinct clinical variants within the traditional primary group and several syndromes associated with cutaneous ossification. For this reason, the following classification is suggested to cover all circumstances in which bone is found in the skin.
In this variant, multiple foci of cutaneous ossification are present at birth or develop in childhood.173.174.175.176. and 177. A family history is sometimes present.173. and 176. Albright’s hereditary osteodystrophy should be excluded. An acquired, late-onset variant is mentioned in the literature.178. and 179.
Although there is usually a history of previous acne and/or dermabrasion of the face,180.181.182.183.184.185. and 186. it appears that multiple miliary osteomas of the face may be found as a true primary condition.187.188. and 189. Multiple, hard, flesh-colored papules, a few millimeters in diameter, develop on the face.
Auricular ossificans (ectopic ossification of the auricle) is a rare condition that may be unilateral or bilateral. It can be associated with local trauma, inflammation, or systemic diseases. It is usually distinguished from secondary ossification of auricular calcinosis (see above). Although the bone may involve the cartilage solely, 190 it may also be confined to the soft tissue of the ear. 191 Cold injury is a frequent predisposing factor to the ossification.190. and 191. It has also been associated with pseudopseudohypoparathyroidism. 192
Included in the osteomas of the distal extremities are the subungual exostoses, which are basically cartilage derived, and a rare group of bony tumors of the digits in which no cartilage or bony connection can be demonstrated.
Cutaneous ossification at an early age may be a presenting feature of Albright’s hereditary osteodystrophy (OMIM 103580), which includes the clinical designations of pseudohypoparathyroidism and pseudopseudohypoparathyroidism.193.194.195.196.197. and 198. The basic abnormality is a defect in tissue responsiveness to parathormone. Hypocalcemia may be present in some cases (pseudohypoparathyroidism type 1a). 199 Mutations in the GNAS1 gene on chromosome 20q13 have been implicated. The gene is one of a small number responsible for differences in gene expression between the maternal and paternal alleles, a phenomenon known as imprinting. 200 Maternal transmission of the mutated gene leads to pseudohypoparathyroidism type 1a, whereas paternal transmission results in Albright’s hereditary osteodystrophy.200. and 201. Defects in the same gene (also paternal transmission) are responsible for progressive osseous heteroplasia (see below). In addition to the ossification of dermal, subcutaneous or fascial tissues, there may also be a characteristic round facies, defective dentition, mental retardation, calcification of basal ganglia, calcinosis circumscripta-like lesions, 201 cataracts, and characteristic short, thick-set fingers with stubby hands and feet attributable to early closure of the metacarpal and metatarsal epiphyses.195. and 196.
A case reported as progressive extensive osteoma cutis associated with dysmorphic features may be a new syndrome. 202
Progressive osseous heteroplasia (OMIM 166350) is an exceedingly rare autosomal dominant condition first described by Kaplan in 1994.203. and 204. It presents as dermal ossification in infancy, followed by progressive ossification of skin, subcutaneous fat, and deep connective tissue.204.205. and 206. Complications include skin ulceration and discharge of bony material, recurrent infections, joint ankylosis, and growth retardation.
Recently, paternally inherited inactivating mutations of the GNAS1 gene on chromosome 20q13 have been implicated in the pathogenesis. Various other mutations in the gene have since been described. 204 Phenotypic expression of the same gene mutation is variable.
Congenital plaque (plate)-like osteomatosis consists of the slow development of a large mass of bone in the lower dermis or subcutaneous tissues.178.207. and 208. It is present at birth or soon afterwards. It appears to be a variant of progressive osseous heteroplasia (see above) with the same defect in the GNAS1 gene. It has been reported to involve the thigh, 209 scalp,210.211. and 212. back, 213 and calf. 214 Two cases reported as ‘limited dermal ossification’, although much more extensive in distribution than the typical plaque-like lesion just described, are best included in this category.215. and 216.
The extremely rare, autosomal-dominant condition of fibrodysplasia ossificans progressiva (OMIM 135100) is manifested by hallux valgus, shortening of the great toes and thumbs, and ossification in muscles and connective tissue. 217 Dermal ossification may precede or accompany these changes. Chondral elements may also be present. The muscles of the shoulder and axial skeleton are commonly involved.
It is caused by a mutation in the ACVR1 gene on chromosome 2q23. 218 As a consequence of this defect, there is overexpression of bone morphogenetic protein-4 (BMP-4) which may be responsible for the deposition of bone. The noggin (NOG) gene may be responsible in rare cases, although some published reports implicating this gene were not able to be confirmed in other laboratories.
This group accounts for the great majority of cases of cutaneous ossification.172.178. and 207. Bone may be found in nevi, particularly on the face (osteonevus of Nanta), in basal cell carcinomas, in up to 20% of pilomatrixomas and less commonly in trichoepitheliomas, hemangiomas, pyogenic granulomas, 219 schwannomas, lipomas, chondroid syringomas, ossifying plexiform tumor, 220 organoid nevi, 221 epidermal and dermoid cysts, dermatofibromas, desmoplastic melanomas, 222 and some cutaneous metastases. 223 This subcategory of secondary ossification (ossification in tumors) accounted for 56 of the 74 cases of cutaneous ossification in one large series. 172 Ossification may also develop in sites of infection, trauma and scarring, such as acne scars,224. and 225. injection sites, hematomas, and surgical scars. Myositis ossificans and the related fibro-osseous pseudotumor of the digits226 can also be included. Abdominal wounds are particularly involved and it seems that injury to the xiphoid process or pubis may liberate bone-forming cells into the wound with subsequent ossification which appears within the first 6 months after surgery. 227 Other circumstances include chronic venous insufficiency of the legs, 228 scrotal calcinosis, 178 auricular calcinosis, 60 scleroderma, morphea,229.230. and 231. dermatomyositis and, rarely, gouty tophi. Secondary ossification has also been reported in neurological diseases associated with paralysis232 and in a plaque of alopecia in a patient with polyostotic fibrous dysplasia. 233 Bone formation occurs in hypertrophic osteoarthropathy, which may be secondary to pulmonary disease (finger clubbing) or occur as a primary disease resulting from mutations in the HPGD gene which encodes 15-hydroxyprostaglandin dehydrogenase. 234
Cutaneous bone usually develops by membranous (mesenchymal) ossification without the presence of a cartilage precursor. There are small spicules or large masses of bone in the deep dermis and/or subcutaneous tissue (Fig. 14.5). Haversian systems and cement lines are usually present. Occasionally there is active osteoblastic activity, particularly in Albright’s hereditary osteodystrophy, but this is unusual in the primary solitary lesion and secondary forms associated with acne scars. Osteoclasts are also uncommon. There is often a stromal component of fat, but occasionally hemopoietic cells are also present. In the congenital plaque-like osteomatosis, bone may extend around the dermal appendages (Fig. 14.6). 207 Pigmentation of the bone has been reported in acne patients receiving tetracycline or minocycline: clinically these nodules may have a bluish color.235.236. and 237. The crystalline component of the bone is hydroxyapatite, as in skeletal bone.
Osteoma cutis. The spicules of bone are undergoing transepidermal elimination. Surface crusting is present. (H & E)
(A) Plaque-like osteoma cutis of the scalp. (B) Bone extends around the eccrine glands. (H & E)
The term ‘cartilaginous lesions of the skin’ encompasses several different entities, which have in common the presence of cartilage of variable maturity. Some of these entities have been discussed in other sections. The following classification has been suggested by Hsueh and Santa Cruz. 238
The hamartomas containing cartilage include accessory tragi, the closely related Meckel’s cartilage (cartilaginous rests in the neck, ‘wattles’241.242.243. and 244.), bronchogenic cysts, and dermoid cysts. The lesions reported as elastic cartilage choristomas of the neck245 were midline and suprasternal and therefore different from the usual laterally placed branchially derived remnants.
These extraskeletal tumors arise most frequently in the soft tissues of the extremities, especially the fingers. 246 They may have varying degrees of cytological atypia in the chondrocytes, but despite this they invariably pursue a benign course.
This group includes osteochondromas, synovial chondromatosis, and subungual exostoses (see p. 864).
The eccrine tumor, chondroid syringoma, may have prominent cartilaginous differentiation which may at first glance obscure its sweat gland origin. Cartilage may develop in degenerated nuchal ligaments producing the nuchal fibrocartilaginous pseudotumor.247. and 248.
The case described as ‘cartilaginous papule of the ear’ defies classification. 249 It may represent a reactive hyperplasia of auricular cartilage.
Hyaline deposits may be seen in the dermis in several ‘metabolic’ disorders, including amyloidosis, erythropoietic protoporphyria and lipoid proteinosis, and Waldenström’s macroglobulinemia. In gouty tophi the deposits are of a crystalline nature, but when these are dissolved in an aqueous fixative the residual stromal tissue appears hyaline. Other causes of hyaline deposits are colloid milium and massive cutaneous hyalinosis; they may also occur following certain corticosteroid injections. Cytoid bodies are a heterogeneous group of hyaline deposits that are commonly overlooked in routine sections.
An unclassifiable deposit, of hyaline type, has been reported in a patient with IgG paraproteinemia and lesions resembling cutis laxa. 250 Eosinophilic homogeneous material was present in the dermis. The material had a tubular pattern on electron microscopy. 250 Eosinophilic deposits have been reported in the base of a cutaneous ulcer and forming follicular plugs in two patients with multiple myeloma. 251 The deposits were monoclonal and identical to those found in the serum. 251
Although the prevalence of gout in the community is relatively constant, the proportion of gouty patients with cutaneous manifestations – tophi – shows a continuing decline.3. and 252. This undoubtedly results from improved clinical management of these patients, particularly the use of allopurinol, a xanthine oxidase inhibitor that blocks uric acid production. Tophi, which are end-stage manifestations of primary gout, are deposits of monosodium urate crystals within and around joints, overlying the olecranon and prepatellar bursae and in the helix of the ears.253. and 254. Sometimes chalky white material is extruded from tophi. Smaller nodular deposits have been described on the fingers and toes and there are reports of leg ulcers or a panniculitis with urate deposition, as the presenting manifestations of gout.255.256. and 257. Tophi have been reported in a patient following the use of acitretin, an oral retinoid, in the treatment of erythrodermic psoriasis. 258
Tophi are dermal and subcutaneous deposits of urate crystals. 259 If material is fixed in alcohol, they appear as well-demarcated deposits of closely arranged, brown, needle-shaped crystals (Fig. 14.7). The crystals are doubly refractile under polarized light. In formalin-fixed material, the crystals will usually have dissolved and there are characteristic, amorphous pink areas corresponding to the sites of crystal deposition (Fig. 14.8). Surrounding the deposits is a granulomatous reaction with macrophages and many foreign body giant cells. 260 There is usually only a sparse chronic inflammatory cell infiltrate. Often there is some fibrosis as well, and in old lesions calcification and even ossification may occasionally develop. Transepidermal elimination of crystals is rarely seen. 261
Gouty tophus. There are brown, needle-shaped crystals forming large deposits in the dermis and subcutis. The biopsy was fixed in alcohol. (H & E)
Gouty tophus. The urate crystals have been dissolved in this formalin-fixed biopsy, leaving a pale hyaline area surrounded by macrophages and foreign body giant cells. (H & E)
It has been suggested that the primary event in the formation of a tophus is the accumulation of macrophages in an acinar arrangement followed by the centripetal transport of urate by the macrophages from the interstitial fluid to the central zone. 260 This expands progressively as more urate crystals are deposited. The corona of macrophages commonly disappears and adjacent deposits may fuse. 260
Amyloidosis refers to the extracellular deposition of eosinophilic hyaline material of autologous origin which has characteristic staining properties and a fibrillar ultrastructure.262.263.264.265. and 266.
The origin of amyloid is diverse: 16 different fibril proteins have been described so far. 267 Many of these are rare or have no relevance to the skin. Six amyloid proteins are of interest in cutaneous pathology: AA, ATTR, Aλ, Aκ, Aβ2M, and AK.267.268. and 269. Mixed amyloid deposits, containing two or more of these proteins are uncommon.270. and 271.
• AA (amyloid A protein) is associated with chronic inflammatory diseases, corresponding to secondary systemic amyloidosis of the traditional classification.
• ATTR (amyloid transthyretin protein) is found in cases of familial amyloidosis. 272 It appears to be the same as FAP (familial amyloid polyneuropathy, type 1).
• Aλ and Aκ are usually grouped together as AL (amyloid light chain protein). These proteins are found in relation to myeloproliferative diseases, particularly multiple myeloma, or in cases with no known associated disease (idiopathic). Aλ is found much more commonly than Aκ. It is the type of amyloid usually found in nodular cutaneous amyloidosis. This type of amyloid (AL) is the most difficult type to confirm immunohistochemically as staining for the two light chains λ or κ may be spotty and uneven. 273
• Aβ2M (amyloid β2-microglobulin protein) is found in amyloid deposits associated with long-term hemodialysis.267. and 274. It deposits mainly in the osteo-articular system, 275 but subcutaneous deposits have been reported. 274 Improvements in hemodialysis have led to the disappearance of this type of amyloid. 273
• AK (amyloid keratin protein) is found in localized cutaneous amyloidosis, both lichen amyloidosus and macular amyloidosis. This protein will be discussed further below.
In addition to the specific fibrillar component, amyloid deposits have been shown to contain several associated and contaminating proteins such as amyloid P, apolipoprotein E, and glycosaminoglycans.267. and 276. Immunoglobulins may be non-specifically trapped within the fibrillar meshwork. Amyloid P, which for a long time was used as a marker for amyloid, is a non-fibrillar glycoprotein which binds to all types of amyloid fibrils.
In primary cutaneous amyloidosis the amyloid is of keratinocyte origin, but how the keratin intermediate filaments transform into amyloid (AK) is speculative. Apoptosis of keratinocytes has been described, but this may simply be the method of cell death in basal keratinocytes that have accumulated an abnormal protein. 277 Another theory is that macrophages in the dermis ‘process’ the filament-rich colloid bodies, converting them into mature amyloid and in the process adopt a beta-pleated sheet pattern (as opposed to the usual alpha pattern of keratin). Active secretion of amyloid by basal keratinocytes is a less favored theory.278. and 279. AK stains with general keratin antibodies, such as EKH4 and AE1. 277 Several subclasses of keratin are found, in particular CK5, which is a constituent of normal basal keratinocytes. 269 However, the presence of CK7, CK17, and CK19, not found in the interfollicular epidermis, suggests an appendageal contribution to the amyloid deposits. 269 Suggested etiological factors in the formation of this type of amyloid include prolonged friction, pruritus, genetic predisposition, Epstein–Barr virus, and environmental factors.
The skin may be involved in the course of systemic (generalized) amyloidosis, but more commonly it is the only organ in the body to be involved – localized cutaneous (skin-limited) amyloidosis. Within each of these two major categories, several distinct clinical variants are found, as outlined in the traditional classification that follows.
• Systemic amyloidosis
Primary and myeloma associated
Secondary
Heredofamilial
Amyloid elastosis
• Localized cutaneous amyloidosis
Lichen, macular and biphasic
Nodular
Poikilodermatous
Anosacral
Familial cutaneous
Secondary localized.
The histochemical, immunofluorescence, and ultrastructural properties of the various cutaneous amyloidoses will be discussed before the description of the individual clinical variants.
Amyloid stains pink with hematoxylin and eosin and metachromatically with crystal violet and methyl violet. 280 It stains selectively with Congo red; in addition, amyloid stained by Congo red gives an apple-green birefringence when viewed in polarized light. Amyloid gives a bright yellow-green fluorescence with thioflavine T. 281 We have found crystal violet to be more reliable than Congo red in sun-damaged skin, which sometimes gives false-positive staining with Congo red; false negatives also occur. The cotton dye pagoda red No. 9 (Dylon), used as a variant of the Congo red method, is said to be more specific for amyloid than Congo red, because it does not stain the material in paraffin sections of lipoid proteinosis, colloid milium, or solar elastosis.282.283. and 284. Congo red staining of the deposits in secondary systemic amyloidosis can be prevented by prior treatment of the sections with potassium permanganate.285. and 286. In some cases of primary systemic amyloidosis the amyloid has relatively little affinity for Congo red. 287 Early cases of localized cutaneous amyloidosis can also be negative using the Congo red method. The author has seen several cases of lichen amyloidosus missed because only a Congo red stain was performed.
Immunoperoxidase methods using monoclonal antisera can also be used to demonstrate amyloid P component (a non-fibrillar protein derived from a glycoprotein found in the blood of all normal persons) in all cutaneous deposits.288.289.290. and 291. As already mentioned, the amyloid in lichen amyloidosus and macular amyloidosis, as well as in secondary localized cutaneous amyloidosis, stains with the monoclonal antibody EKH4 which recognizes 50 kDa neutral and acidic keratin. 282 It also stains with the keratin antibody AE1. The antikeratin antibody EAB-903, which recognizes 57 kDa and 66 kDa keratin peptides, reacts with the amyloid deposits in both lichen amyloidosus and macular amyloidosis, but not with the amyloid in systemic amyloidosis. 292 Other keratin monoclonals have given mixed results.292.293.294. and 295. Antisera are also available commercially against amyloid A (AA), amyloid L (AL), both anti-κ and anti-λ, islet amyloid polypeptide (IAPP), and amyloid β2-microglobulin (Aβ2M). Amyloid deposits can be misclassified if the antibody panel is incomplete. 296
Immunoglobulins, particularly IgM, and C3 complement are found in cutaneous amyloid deposits.297. and 298. Most of the studies have been confined to the localized cutaneous forms. Amyloid is thought to act like a filamentous sponge with non-specific trapping of the immunoglobulins and complement. 299
Amyloid is composed of straight, non-branching filaments, 6–10 nm in diameter, of indefinite length and in random array (Fig. 14.9). A close association with elastic fibers is sometimes observed.300.301. and 302. Intracellular amyloid has been noted in dermal fibroblasts303. and 304. and in keratinocytes in lichen amyloidosus. 303
Lichen amyloidosus. There are intracellular deposits and some dense tonofilament bundles in basal keratinocytes. The deposits appear to represent the earliest stages of amyloid formation. (× 45 000)
The ultrastructural studies of Hashimoto and colleagues305. and 306. and other groups307.308. and 309. have shown that the basal epidermal cells are involved in the histogenesis of the amyloid in lichen amyloidosus and macular amyloidosis. Basal keratinocytes overlying dermal amyloid show degenerative changes with the accumulation of modified tonofilaments (thicker, but less electron-dense than normal) in the cytoplasm. 310
Primary systemic amyloidosis (AL) is a rare disorder with an incidence of approximately 8 per 1 million persons per year. 311 However, cutaneous involvement is common in this form of amyloidosis and in the closely related myeloma-associated amyloidosis, with lesions in approximately one-third of patients.262.312. and 313. There are non-pruritic, waxy papules on the scalp, face, and neck and sometimes the genitalia.286.314.315. and 316. There is a predilection for the periorbital areas. Plaque-like lesions may develop on the hands and flexural areas. 317 Hemorrhage into the lesions is quite common.315.318.319. and 320. Rare presentations include alopecia,321. and 322. occlusion of the external auditory canals,323. and 324. chronic paronychia, 317 nail dystrophy,325. and 326. digital nodules, 327 bullous lesions,312.328.329.330.331. and 332. indurated cord-like lesions resulting from thick vascular deposits, 333 condyloma-like lesions in the perianal region, 334 muscle pseudohypertrophy, 335 and elastolytic lesions (acquired cutis laxa).336.337. and 338. As mentioned above, the fibrillar protein is derived from light chains of immunoglobulin (AL), either λ or κ. The coexistence of β2-microglobulin has been reported. 271
Lenalidomide, an analogue of thalidomide, has been used in the treatment of amyloidosis associated with multiple myeloma. 339 There is a high incidence of cutaneous adverse reactions to this therapy. The median survival of patients with systemic amyloidosis is about 13 months from diagnosis. 311
Papular lesions result from deposits of amyloid in the papillary dermis; in plaques there is a more diffuse dermal infiltration, sometimes with extension into the subcutis (Fig. 14.10). 340 In this latter site, amyloid deposits around individual fat cells to form ‘amyloid rings’ (Fig. 14.11). Dermal blood vessels are usually involved in hemorrhagic lesions (Fig. 14.12) and pilosebaceous units are involved in areas of alopecia.315. and 340. The rare bullous lesions are caused by intradermal cleavage within the amyloid deposits.312. and 341. There is often clefting about and within the amyloid in the larger papular lesions. If the deposits are large, there is often attenuation of the overlying epidermis. 340 There are no pigmented cells, and inflammatory cells are scarce. 341
Primary amyloidosis. (A) The hyaline deposits in the dermis show some artifactual separation. (H & E) (B) Another case with deposition accentuated in the upper dermis. (H & E, with crystal violet inset)
Amyloid rings. There are fine deposits of amyloid surrounding individual fat cells. (H & E) (Photomicrograph kindly supplied by Dr G Strutton)
Primary amyloidosis. (A) There is considerable hemorrhage between the hyaline deposits. (B) A small artery in the subcutis has thickening of its wall due to amyloid deposition. (H & E)
Clinically normal skin will show deposits of amyloid in the dermis, usually in the walls of blood vessels, in more than 50% of biopsies in cases of primary systemic amyloidosis. 342 A recent study found cutaneous amyloid deposits in 97% of cases of systemic amyloidosis, making skin biopsy a preferred method of diagnosis of systemic amyloidosis. 268 Abdominal fat aspiration is another procedure, 343 but a large series from the Mayo Clinic found a low yield by this technique. 344
Clinical involvement of the skin is rare in cases of secondary systemic amyloidosis.262. and 340. Uncommonly, this form of amyloidosis is the result of an underlying chronic skin disease such as lepromatous leprosy, mycosis fungoides, hidradenitis suppurativa, arthropathic psoriasis,285.345. and 346. Schnitzler’s syndrome, 347 or dystrophic epidermolysis bullosa. 348 Although no cutaneous involvement was recorded, renal amyloidosis has been reported in a patient with concurrent familial Mediterranean fever and pseudoxanthoma elasticum. 349 Both diseases involve gene mutations in the 16p13 region. Secondary amyloidosis may occur following hemodialysis; in these circumstances the protein fibril deposited is β2-microglobulin.275.350. and 351. In other circumstances the fibrillar component is amyloid A protein (AA). It has been suggested that the presence of AL amyloidosis may enhance the development of amyloid A (AA) amyloidosis. 352
There are skin manifestations in certain of the heredofamilial amyloidoses. 353 These include trophic changes and amyloid deposits in the arrector pili muscles in (heredo)familial amyloid polyneuropathy263.283. and 354. and urticaria in other forms such as the Muckle–Wells syndrome (urticaria, amyloidosis, and deafness).355. and 356. The major pathological hallmark of familial amyloidotic polyneuropathies (FAP) is the formation of transthyretin-derived amyloid deposits in several organs. 272 The disease (OMIM 176300) has an autosomal dominant manner of inheritance. The gene map locus is 18q11.2–q12.1. It is endemic in the northern area of Portugal, but it has also been reported in patients of non-Portuguese descent. 357 The Finnish type of amyloidosis is mentioned below.
Amyloid elastosis is an exceedingly rare form of amyloidosis with cutaneous lesions and progressive systemic disease.358. and 359. The elastic fibers in the skin and serosae are coated with the amyloid material; 358 the amyloid is localized to the microfibrils of the elastic fibers. 360 Why amyloid is preferentially deposited on elastic fibers, resulting in clinically evident lesions, is unknown. It is a variant of systemic AL amyloidosis. 361
Lichen amyloidosus and macular amyloidosis are clinical variants of the same process.283.364. and 365. Patients with features of both variants, or transformation from one to the other (biphasic form), are well documented.366.367.368. and 369. There is no visceral involvement in lichen amyloidosus or macular amyloidosis. 370 An association with multiple endocrine neoplasia syndrome 2A (MEN 2A – OMIM 171400) has been reported.371. and 372. A Brazilian family with localized cutaneous amyloidosis (OMIM 105250) due to a mutation in the oncostatin M receptor-β (OSMR) gene has been reported. 373 Other reported associations are possibly coincidental, although chronic pruritus could be implicated in two such associations.374.375.376. and 377. The fibrillar component is derived from keratinocytes and designated AK (amyloid keratin). All of the cytokeratins detected in the deposits are of basic type (type II). CK5 is strongly expressed. 378
Lichen amyloidosus presents as small, discrete, often pruritic, waxy papules with a predilection for the extensor surfaces of the lower extremities.370. and 379. Rare clinical presentations have included similar distribution in identical twins, 380 a thermosensitive distribution with sparing of areas with a higher temperature, 381 and involvement of the glans penis.382. and 383. Lichen amyloidosus is not uncommon in Southeast Asia and some South American countries.370. and 384. It has been associated with chronic Epstein–Barr virus (EBV) infection,385. and 386. with Kimura’s disease, 387 and angiolymphoid hyperplasia with eosinophilia. 388 Others believe it is a consequence of chronic scratching.389. and 390. This may be the explanation for its rare occurrence in HIV-associated papular pruritus391 and in refractory atopic dermatitis. 392 Nerve fibers are reduced at the dermoepidermal junction but not in the papillary dermis, leading to the suggestion that the pruritus may result from hypersensitivity of the nerve fibers that remain following the unexplained loss of nerves at the dermoepidermal junction. 393
Dermabrasion, combined bath PUVA photochemotherapy and oral acitretin, acitretin alone, hydrocolloid dressings, and the pulsed dye laser have been used in the treatment of lichen amyloidosus.394.395.396.397. and 398.
Macular amyloidosis is relatively common in Asia and the Middle East. 399 It occurs as poorly defined hyperpigmented and rippled patches on the trunk.309. and 400. Rarely, there is widespread pigmentation.401.402. and 403. Pigmentation resembling incontinentia pigmenti has been reported. It was associated with subepidermal blister formation. 404 There is a predilection for the interscapular region of adult females. 405 Lesions are often pruritic. Macular amyloidosis has been reported in Japanese following prolonged rubbing of the skin with nylon brushes and towels.282.406. and 407. Other types of friction have sometimes been implicated.408. and 409. Unusual presentations include involvement of the thighs, 410 knees, 411 or elbows. 412 The Q-switched Nd:YAG laser has been used to reduce the pigmentation in patches of macular amyloidosis. 413
Both lichen amyloidosus and macular amyloidosis are characterized by small globular deposits of amyloid in the papillary dermis (Fig. 14.13). 298 Sometimes a thin band of compressed collagen separates these deposits from the overlying epidermis; 370 at other times the deposits are in contact with the basal cells and sometimes interspersed between them. More extensive deposits are sometimes seen (Fig. 14.13). Transepidermal elimination of the amyloid sometimes occurs. 414 Subepidermal clefting above the deposits rarely occurs. 415 Pigmented cells are often seen within the dermal deposits. The presence of these cells is an important clue to the diagnosis of primary cutaneous amyloidosis on H & E-stained sections.
Macular amyloidosis. (A) Hyaline material, barely distinguishable from collagen, is present in the papillary dermis. The diagnosis can be easily missed. (H & E) (B) The deposits are more extensive than usual. (Pagoda red)
In lichen amyloidosus (Fig. 14.14) the overlying epidermis shows hyperkeratosis and acanthosis, the changes sometimes resembling those of lichen simplex chronicus (see p. 86). 416
Lichen amyloidosus. (A) Small, hyaline deposits of amyloid are situated in the papillary dermis. There is overlying epidermal hyperplasia. (H & E) (B) The size of the deposits can be better appreciated on the special stain for amyloid. (Congo red) (C) The preferable stain for amyloid keratin is the crystal violet stain, shown here. (Crystal violet)
In both types of amyloidosis occasional apoptotic bodies are present within the epidermis. 417 Basal vacuolar change also occurs.
As already mentioned, the author routinely uses the crystal violet stain to confirm the amyloid deposits. It is superior to both the alkaline and Highman’s Congo red stains. The detection of cytokeratins (using an LP34 clone which detects CK5, 6, and 18) is the new gold standard. 418
Auricular amyloidosis (amyloidosis of the auricular concha) has also been reported in the past as ‘collagenous papules of the ear’.419.420. and 421. It presents with papules or plaques localized to the ear.422. and 423. It may be a variant of lichen amyloidosus (Fig. 14.15). The deposits are localized to widened dermal papillae. 422 It is not as rare as the paucity of reports would suggest.
Auricular amyloidosis. This condition was formerly known as ‘collagenous papules of the ear’. (H & E)
Nodular amyloidosis is an uncommon form of cutaneous amyloidosis which is manifested by solitary424 or multiple waxy nodules, 0.5–7 cm in diameter, on the lower extremities, 425 face,426.427.428.429.430. and 431. neck, 432 scalp, or genital region.433.434.435.436.437. and 438. In at least 15% of cases, the patient will subsequently develop systemic amyloidosis.416.435. and 439. None of the 16 patients with nodular amyloidosis reported from the Mayo Clinic had progressed to systemic amyloidosis at the time of the study. 440 In another study, the rate of progression was 7%. 441 A light-chain origin of the amyloid (AL) has been proved in many cases.433.437.442. and 443. Trauma was implicated in one case. 444
Nodular deposits of amyloid, derived mostly from β2-microglobulin, are a rare finding in the skin of patients with chronic renal failure on long-term hemodialysis.274. and 275. ‘Amyloidoma’ refers to a rare tumor mass of amyloid that may be found in the subcutis.445.446.447. and 448. It may be composed of AA, AL, or IAPP (islet amyloid polypeptide) amyloid. 445
There are large masses of amyloid in the dermis and subcutis, with accentuated deposition around deep vascular channels and adnexal structures. 315 Plasma cells, some with large Russell bodies, are usually quite prominent at the margins and within the amyloid islands.341.435. and 449. Monoclonality of these cells has been confirmed.440.450. and 451. The deposits do not stain with antikeratin antibodies. 269 They may stain for Aλ, Aκ, or Aβ2M (see above). Foreign body giant cells and focal calcification are sometimes present.435. and 452. The amyloid may be deposited in relation to the elastica.300. and 453.
Poikilodermatous lesions are rare. 454 A distinct subset of patients have short stature, early onset, light sensitivity, and sometimes palmoplantar keratoderma – the poikilodermatous cutaneous amyloidosis syndrome. 454
Included in this category are the cases reported as amyloidosis cutis dyschromica.455. and 456. It is characterized by reticulate hyperpigmentation with hypopigmented spots over much of the body. It is assumed to be a familial disorder. 457
There is amyloid in the dermal papillae and around dermal blood vessels, resembling the pattern of primary systemic amyloidosis.
Anosacral amyloidosis is a rare form of primary cutaneous amyloidosis that has been reported in Chinese persons. 458 It presents as a light brown lichenified plaque of the perianal region extending onto the lower sacrum. The amyloid is of keratinous origin (AK).
The amyloid deposits are situated in the papillary dermis. There is some overlying epidermal hyperkeratosis, acanthosis and melanin incontinence. 458
Familial primary cutaneous amyloidosis is an extremely rare, autosomal dominant genodermatosis with keratotic papules and/or swirled hyper- and hypopigmentation459 on the extremities and sometimes the trunk.315.460. and 461. The clinical features may resemble lichen amyloidosus. 462 A susceptibility locus may exist on chromosome 1q23 but the gene encoding serum amyloid P component (APCS), also found at this site, may not be involved. 463 The same group has subsequently suggested that the gene is linked to chromosome 5p13.1–q11.2. 464 Transepidermal elimination of the papillary dermal deposits has been a characteristic feature. 461
Secondary localized cutaneous amyloidosis refers to the finding of amyloid in the stroma of various cutaneous tumors such as basal cell carcinoma (Fig. 14.16)465.466. and 467. and, less commonly, squamous cell carcinomas, 468 nevocellular nevi, 469 trichoblastomas, cylindromas, pilomatrixomas, and syringocystadenoma papilliferum. 470 Amyloid may underlie the epithelium in seborrheic and actinic keratoses, 471 Bowen’s disease, 472 porokeratosis, skin treated with ultraviolet A radiation after the ingestion of psoralens (PUVA), 473 and mycosis fungoides.283.474. and 475. Amyloid has also been reported localized to areas of severe solar elastosis: 476 amyloid A protein was identified in this latter case. In all other circumstances, the amyloid appears to be of keratinocyte origin (AK). Apolipoprotein E (apoE) is also a constituent of the amyloid deposits in both secondary localized, and primary cutaneous amyloidosis. 477
Secondary amyloidosis. Hyaline deposits are present in the stroma of a basal cell carcinoma. (H & E)
Porphyria is a metabolic disorder with varied cutaneous manifestations. It is considered in detail in Chapter 18, page 495.
The characteristic histological feature of the cutaneous porphyrias is the deposition of lightly eosinophilic, hyaline material in and around small blood vessels in the upper dermis. In erythropoietic protoporphyria the hyaline material also forms an irregular cuff around these vessels but it does not encroach upon the adjacent dermis as much as the hyaline material does in lipoid proteinosis (see below). Furthermore, there is no involvement of the sweat glands in cutaneous porphyria. The hyaline material has similar staining characteristics in both diseases, although the hyaline material in porphyria tends to stain less intensely with Hale’s colloidal iron method than it does in lipoid proteinosis.
Lipoid proteinosis, also known as Urbach–Wiethe disease (OMIM 247100), is a rare, autosomal recessive, multisystem genodermatosis which primarily affects the skin, oral cavity, and larynx, with the deposition of an amorphous hyaline material.478.479.480.481.482.483.484. and 485. The disease occurs worldwide but it is more common in some geographical areas, such as parts of South Africa and Turkey.486. and 487. A gene founder effect has been proposed to explain the high number of cases in South Africa. 488 The early clinical features are hoarseness and the development of recurrent skin infections, sometimes with vesiculobullous lesions which heal leaving atrophic pock-like scars.489.490. and 491. Waxy papules and plaques develop progressively over several years on the face, scalp, neck, and extremities. 492 Other features include beaded papules on the eyelid margins (blepharosis),493. and 494. oral ulceration, 495 and verrucous lesions on the elbows, knees, and hands. 496 A possible localized form, limited to hyperkeratotic lesions on both hands and wrists, has been reported. 497 Although deposits have been found in many organs of the body, resulting dysfunction is rare.498. and 499. Insulin resistance has been reported in two adolescent siblings. 500 Epilepsy may be associated with calcification of the hippocampus. 488
Lipoid proteinosis results from mutations in the gene (ECM1) encoding extracellular matrix protein 1 on chromosome 1q21. More than 20 different mutations have been described,501. and 502. and it has been suggested that individuals with mutations in exon 7 have a milder phenotype than those with exon 6 mutations. 486 Consanguinity is present in up to 20% of cases.487. and 503. The mechanism by which the mutations lead to excessive basement membrane deposition in skin and mucosae are poorly understood, but it has recently been suggested that a failure of mucocutaneous lymphangiogenesis may be the cause. 504 Earlier work suggested it was a lysosomal storage disease.505. and 506. ECM1 binds to the major heparin sulfate proteoglycan, percelan, and functions as a ‘biological glue’ in the dermis, helping to regulate basement membrane and interstitial collagen fibril assembly. 507 In the epidermis ECM1 plays a role in keratinocyte differentiation which may be the cause of the warty hyperkeratosis found in this condition, 488 although one study has shown that the absence of ECM1 does not lead to alterations in epidermal maturation. 508 Nevertheless, the finding of free-floating desmosomes in infants with vesicular lesions suggests a defect in the attachment of desmosomes to keratin filaments, probably a consequence of ECM1 deficiency. 509
The deposited material has increased laminin and collagen of types IV and V and a relative decrease in collagen type I.510.511.512.513.514. and 515. There is also a selective increase in pro-α1(IV)mRNA in lipoid proteinosis. 512
Limited success has been achieved by treating the disease with steroids, chloroquine, and etretinate. D-penicillamine has also been used with some benefit. 516
There is a progressive deposition of pale, eosinophilic, hyaline material in the superficial dermis, but this is initially localized around small blood vessels and at the periphery of eccrine sweat glands. 479 Small capillaries are sometimes increased in number. In advanced lesions, the deposits around blood vessels may have an ‘onion-skin’ appearance (Fig. 14.17). There is also progressive atrophy of secretory sweat glands associated with increasing hyaline deposition. This material is also deposited in arrector pili muscles and around pilosebaceous units. Calcification of the deposits is extremely rare. 504 The epidermis may show hyperkeratosis and some acanthosis in the verrucous lesions.
(A) Lipoid proteinosis. (B) Hyaline material is arranged around blood vessels in the papillary dermis in an onion-skin pattern. (H & E)
The histology of the vesicular lesions has been described infrequently.519. and 520. There is extensive non-dyskeratotic acantholysis of the epidermis as well as a subepidermal cleft. 519 The superficial epidermis was absent in the erosive, vesicular lesions reported in one study. 520
The hyaline deposits are PAS positive and diastase resistant (Fig. 14.18). They stain positively with colloidal iron and Alcian blue at pH 2.5 and also with Sudan black and oil red O on frozen sections.521. and 522. The accumulation of lipid is usually a late and presumably secondary phenomenon.521. and 523. Types IV and V collagen are increased at the dermoepidermal junction and around blood vessels.524. and 525.
Lipoid proteinosis. The hyaline material involving the papillary dermis and wall of blood vessels is PAS positive. (Periodic acid–Schiff)
Although histologically and histochemically similar material is found in erythropoietic protoporphyria, the deposits in the latter condition are more limited in distribution, being perivascular only. 526 Sweat glands are not involved in porphyria.
In lipoid proteinosis there are fine collagen fibrils embedded in an amorphous, granular matrix.492.527.528. and 529. There is prominent reduplication of the basal lamina at the dermoepidermal junction and concentrically around vessels.510.513.529. and 530. Calcium deposits may be seen. Myofibroblasts have thick basal laminae in continuity with the hyaline masses. 531 Cytoplasmic inclusions have been noted in the fibroblasts; their exact significance is unknown.505. and 513. In blistering lesions there is a dissociation of relatively intact desmosomes from keratinocytes, with desmosomes that are ‘free-floating’ in the intercellular spaces or attached by thin strands to the cell membrane. 509
Translucent papules, formed by deposits of monoclonal IgM, are an uncommon manifestation of Waldenström’s macroglobulinemia (see p. 945). The hyaline deposits that fill the papillary and upper reticular dermis are strongly PAS positive (Fig. 14.19). The deposits encase blood vessels and hair follicles. 532 Artifactual clefts may form. Ultrastructurally, the deposits are composed of fibrillar and granular material. 533
(A) Waldenström’s macroglobulinemia. Hyaline deposits fill the papillary dermis. (H & E) (B) They appear to be more extensive on special stains. (Periodic acid–Schiff) (Slides kindly provided by Dr Richard Williamson)
There are at least five distinct clinicopathological conditions that can be included under the umbrella term of ‘colloid milium and colloid degeneration’. 534 Regrettably, our knowledge of these conditions is limited by the paucity of reports in the literature. The five variants are:
The adult type develops in early to mid-adult life with numerous yellow-brown, semitranslucent, dome-shaped papules, 1–4 mm or more in diameter. They may be discrete or clustered to form plaques. Verrucous lesions are rare. 544 The cheeks, ears, neck, and dorsum of the hands are sites of predilection. 545 Often there is a history of exposure to petroleum products and/or excessive sunlight,538. and 546. but obviously there is some underlying predisposition as well. 547 It has developed in a patient with β thalassemia major. 548 Unilateral involvement of the sun-exposed arm of taxi and truck drivers has been reported.549. and 550. The case reported on non-sun-exposed skin seems to be a different entity. 539 The material in the dermis is thought to represent a degeneration product of elastic fibers induced by solar radiation (actinic elastoid).551. and 552. Fractional photodermolysis produced clearance of facial lesions in one case of adult colloid milium. 553
Juvenile colloid milium is exceedingly rare.540.554.555.556. and 557. Papules or plaques develop, usually on the face and neck, prior to puberty. Conjunctival and gingival involvement have been reported.558. and 559. It has been suggested recently that juvenile colloid milium and ligneous conjunctivitis are different clinical phenotypes of severe type 1 plasminogen deficiency. 560 Some purported cases probably represent examples of erythropoietic protoporphyria.
Pigmented colloid milium541 is found as gray to black clustered or confluent papules on the face, following the excessive use of hydroquinone bleaching creams (see ochronosis, p. 388).
Colloid degeneration (paracolloid) presents as nodular, plaque-like areas, usually in chronically sun-exposed skin, particularly the face.542. and 561. This is probably a heterogeneous group as illustrated by the case occurring on penile skin. 562
Acral keratosis with eosinophilic dermal deposits is the term used by Saeed, Sagatys, and Morgan for six cases that presented with agminated or solitary papules of the distal finger found on histological examination to contain amorphous eosinophilic deposits. 543 The lesions were slowly progressive and had been present for 1–5 years. Only one patient had a history of chronic sun and hydrocarbon exposure. Their age ranged from 59 to 81 years. 543
In the adult form, there are nodular masses of homogeneous, eosinophilic material expanding the papillary dermis and extending into the mid dermis (Fig. 14.20). 536 Fissures and clefts divide this material into smaller islands and fibroblasts are commonly aligned along the lines of fissuring (Fig. 14.21). A thin grenz zone of uninvolved collagen usually separates the colloid material from the overlying epidermis, which is thinned. 563 Some clumped elastotic fibers are often present in this grenz zone and also between and below the colloid masses, but the colloid material itself stains only lightly or not at all with elastic stains. 552 This material has been reported to stain positively with crystal violet and Congo red and to give fluorescence with thioflavine T; such reactions are more likely to be positive on frozen than paraffin sections.536. and 563. Our own material (including a few cases using frozen sections) has not shown these reactions. In contrast to lipoid proteinosis and primary cutaneous amyloidosis, colloid milium does not contain laminin or type IV collagen. 554
Colloid milium. (A) The clefted, hyaline material in the papillary dermis forms a papular lesion. (B) A plaque-like lesion is present. (H & E)
Colloid milium. The clefted, hyaline material is hypocellular. (H & E)
In the juvenile form, hypocellular material is present in the broadened dermal papillae; this shows some clefting with intervening spindle or stellate fibroblasts. 540 In most areas there is no grenz zone and the basal layer may show hyaline transformation with a transition towards the dermal material. The colloid is PAS positive and sometimes methyl violet positive, but it is usually Congo red negative. 555 The material shows positivity with a polyclonal antibody to cytokeratin (MNF116). 558
In the pigmented form, 541 there are lightly pigmented colloid islands in the upper dermis (see p. 388).
In the plaque type of colloid degeneration, 542 there is amorphous, homogenized, dermal collagen with small fissures and clefts extending deeply into the dermis (Fig. 14.22). It is relatively acellular. The material is basophilic in contrast to the eosinophilic fissured material found in the case occurring on penile skin (see above). It is weakly PAS positive, but negative with Congo red and crystal violet. There is patchy staining with elastic tissue stains, but other areas are negative.
Colloid degeneration (paracolloid). The deposits extend more deeply than in colloid milium and clefting is often less conspicuous. (H & E)
In acral keratosis with eosinophilic dermal deposits there were variable degrees of hyperkeratosis and papillomatosis. An epidermal collarette was present in four of the six cases. The central epithelium was effaced by a sharply circumscribed deposit of amorphous eosinophilic material confined to the papillary dermis. 543 The material was fissured in only one case. It had some resemblance to colloid degeneration, particularly the case reported from the penis which was also eosinophilic (see above). The material was trichrome positive and PAS positive with diastase resistance. Stains for amyloid, protein P, collagen type IV, and pan-keratin were negative. There was a conspicuous absence of elastic fibers in the deposits, similar to the findings in the case of colloid degeneration from the penis (see above).
The ultrastructural features are different in the various types. In the adult form, there are large amounts of amorphous and granular material with some wavy, ill-defined, short, and branching filaments.563. and 564. Some components of actinic elastoid are present at the margins of the islands. 283 There are active fibroblasts. In the juvenile form, there are fibrillary masses with some whorling, rare nuclear remnants, and some melanosomes and desmosomes. 540 Fibrillary transformation of keratinocytes has been observed, leading to the concept that the dermal tonofilament-like material is of epidermal origin.540. and 555. This has been confirmed by positive staining using a polyclonal antikeratin antibody. 554 Colloid degeneration has shown microfilaments admixed with collagen, but more studies are needed before definite conclusions are reached.
The term ‘massive cutaneous hyalinosis’ has been used to describe the condition of a patient with massive amorphous deposits of hyaline material in the deep dermis and subcutis of the face and upper trunk. 565 The material was PAS positive, Congo red negative, and ultrastructurally non-fibrillary. 565 Subsequent investigations have shown that there are three major components of this hyaline material: kappa light chains, a mannose-rich glycoprotein, and type I collagen. 566
The local injection of corticosteroids into keloids or various soft tissue lesions results in a characteristic histological appearance should this site subsequently be biopsied.567.568.569. and 570.
There are usually well-defined, irregularly contoured lakes of lightly staining material in the dermis or deeper tissues. 568 The material is finely granular or amorphous and is surrounded by a variable histiocytic response, sometimes with a few admixed foreign body giant cells and lymphocytes (Fig. 14.23). 570 On low power, the material resembles to some extent that seen in gouty tophi after the crystals have been dissolved by formalin fixation. Crystal-shaped empty spaces may be seen within the material and occasionally birefringent crystals have been present. 570 Sometimes there is no discernible reaction, while at other times a few neutrophils may be present. There is some controversy whether these differing appearances are time related. 570
(A) Triamcinolone injection site. (B) There is pale, foamy material surrounded by a palisade of macrophages. (H & E)
The material may be weakly PAS positive but, although superficially resembling mucin, it does not stain for it. 569
Hyalin angiopathy is one term used for an entity that is also known as giant cell hyalin(e) angiopathy and pulse granuloma.571. and 572. It is an unusual histological change that has been reported in the oral cavity and skin. 573 All cutaneous cases have occurred in skin close to openings of the gastrointestinal tract.571. and 574. They are thought to represent an unusual foreign body reaction to implanted material. It is characterized by amorphous, eosinophilic material within and around blood vessels associated with acute or chronic inflammation. It does not stain for amyloid. As the presence of giant cells is not always a conspicuous feature in the surrounding inflammatory reaction, it seems best not to refer to this condition as ‘giant cell hyalin angiopathy’. 573 Proponents of the term pulse granuloma point out that the material is not always confined to the vascular surrounds.
Infantile systemic hyalinosis (OMIM 236490) and juvenile hyaline fibromatosis (OMIM 228600) are rare, autosomal recessive conditions characterized by multiple subcutaneous nodules, gingival hypertrophy, joint contractures, and hyaline deposits.575.576.577. and 578. They are allelic and characterized by pathogenic mutations in the capillary morphogenesis protein 2 (CMG2) gene on chromosome 4q21.575.579. and 580. The protein encoded by this gene is an integrin-like cell surface receptor for laminin and type IV collagen which may play a key role in cell–matrix or cell–cell interactions. 579
In infantile systemic hyalinosis the skin lesions are present at birth or appear in the first few months with hyperpigmented plaques over bony prominences.581. and 582. Pearly papules on the head and neck, and fleshy nodules, particularly in the perianal region, then develop.575. and 579. There is failure to thrive; death occurs in early childhood.583. and 584.
Juvenile hyaline fibromatosis is characterized by papules, nodules, and large tumors on the hands, scalp, and ears that develop over the first few years of life.585.586.587. and 588. There is also hypertrophy of the gingiva, flexural contractures, and often focal bone erosion.589.590.591.592.593.594.595.596. and 597. A localized form, with slow progression and no visceral involvement, has been reported. 598 Spontaneous regression of tumors sometimes occurs. Recurrent infections may lead to death.
Both lesions are characterized by the deposition of an amorphous hyaline, eosinophilic substance in which spindle-shaped cells are embedded. It may be vaguely chondroid. 599 Basophilic calcospherules may form in the deposits. 600 The material is PAS positive and diastase resistant. 601 The matrix is more abundant in older lesions, whereas recent lesions tend to be more cellular. 576 The material does not stain with Alcian blue. 594 It lacks elastic fibers. A case with minimal hyaline change has been reported. 602
Cytoid bodies are ovoid, round or polygonal, discrete deposits which vary in size from 5 to 20 µm or more in diameter. The term has been applied to a heterogeneous group of deposits which include amyloid, colloid bodies, Russell bodies, and elastic globes. 604 With the exception of Russell bodies, which are derived from plasma cells, cytoid bodies are usually found in the papillary dermis.
Colloid bodies are derived from degenerate keratinocytes, usually associated with the lichenoid reaction pattern. They represent tonofilament-rich bodies extruded into the dermis, but they are sometimes trapped in the epidermis and are carried upwards with normal epidermal maturation. They are considered with the lichenoid tissue reaction in Chapter 3, page 36.
Elastic globes were first described in the 19th century and were for a time regarded as a diagnostic sign in cutaneous lupus erythematosus or scleroderma. 604 In 1965, Pinkus and colleagues described them in normal skin and suggested that they are a structural variant of elastic fibers. 605 They can be found regularly in clinically normal skin from the face and extremities, particularly the calf. It has been suggested that elastic globes in some circumstances may represent the end stage of degenerated colloid bodies; this has not been confirmed by immunohistochemistry, which shows that elastic globes have an immunological profile close to elastic fiber microfibrils. 606
Elastic globes are usually amphophilic, PAS-positive structures found in the papillary dermis (see p. 339). They may have a slight basophilic tint in sun-damaged skin. They are usually larger than cell size (Fig. 14.24), stain strongly with elastic tissue stains and are weakly autofluorescent.
Elastic globes in the papillary dermis. (H & E)
Electron microscopy shows electron-dense, granular, amorphous, and filamentous material.
A heterogeneous group of exogenous and endogenous pigments may be found in the skin. For convenience, the various heavy metals and drugs that produce deposits and/or pigmentary changes are discussed here as well.
For completeness, it should be mentioned that the shaving heads and foils used in electric shavers may be a daily source of iron-chromium-nickel contamination of the skin, leading theoretically to allergic reactions. 608 Deposits of iron, nickel, and chromium have been reported in the skin following total elbow arthroplasty. 609 The metallosis produced blue-gray pigmentation of the forearm. 609 Unidentified pigment deposits have also been reported in the skin following a high-pressure paint-gun injury of a finger; the reaction simulated a giant cell tumor of tendon sheath. 610 Traumatic osmium tetroxide inoculation can result in gray-brown staining to elastic tissue and amorphous gray-brown deposits. 611
Yellow-orange macular discoloration of the skin (xanthoderma) may be produced by jaundice, carotenoderma, ‘tanning pills’ and sprays, and several drugs. This topic was reviewed in 2007. 612
Ochronosis refers to the yellow-brown or ocher pigment (homogentisic acid) deposited in collagen-containing tissues in alkaptonuria.613. and 614. Alkaptonuria (OMIM 203500) is an autosomal recessive disorder in which the hepatic and renal enzyme homogentisic acid oxidase is absent.615.616.617.618.619. and 620. The gene responsible (HGD) maps to chromosome 3q21–q23. The term ochronosis is also used for the deposition of similar hydroquinone derivatives in certain exogenously induced conditions which sometimes followed the topical use of phenol in the treatment of leg ulcers and of picric acid in the treatment of burns (both procedures have now been abandoned) and which are still seen as a complication of the oral administration621. and 622. or intramuscular injection623 of antimalarial drugs and the topical use of hydroquinone bleaching creams in black races.624.625.626.627.628.629.630.631.632.633.634. and 635. The author has also seen it in a patient who consumed large quantities of quinine-containing tonic water.
There is some clinical variability in the presentation of the various types. In alkaptonuria, there is bluish and bluish-black pigmentation of the face, neck, dorsum of the hands and palmoplantar region636. and 637. and bluish discoloration of the sclerae and of the cartilage of the ears and sometimes of the nose. 638 Acrokeratoelastoidosis-like lesions were present in one case. 639 In the pigmentation associated with antimalarial therapy, the pretibial, palatal, facial, and subungual areas have been involved. 640 In hydroquinone-induced lesions, the face (particularly the malar areas), neck and sometimes the ears, corresponding to sites of application of the cream, are involved. 641 The dorsal aspect of the interphalangeal joints is frequently affected. 642 There is hyperpigmentation, with variable development of finely papular and even colloid milium-like areas.624.625. and 626. Skin atrophy, striae, and acne also develop.642.643.644. and 645. Of interest is the complete absence of hydroquinone-induced ochronosis in areas of vitiligo. 646 This suggests that melanocytes are necessary for the deposition of the pigment, which is presumably derived from a melanin-hydroquinone precursor. 646
There is a marked similarity between the ochronotic deposits in alkaptonuria and hydroquinone-induced ochronosis. 626 In the earliest stages, there is some basophilia of the collagen fibers in the upper dermis, followed by the appearance of stout, sharply defined, ocher-colored fibers which may be crescentic, vermiform, or banana-shaped (Fig. 14.25). 625 Fragmented fibers and small pigmented deposits may also be present, the latter lying free in the dermis or in macrophages. Pigment granules are also found in the endothelial cells of blood vessels and the basement membrane of sweat glands. 616 Colloid milium-like foci often develop in the hydroquinone-induced lesions, and these foci may show no visible ochronotic material or only partial staining of the fibers. 625 Transepidermal elimination of ochronotic fibers has been observed.541. and 647. There are a variable number of macrophages present, but they are usually infrequent in alkaptonuria. Rarely, foreign body giant cells surround the fibers, but this occurs more often in extracutaneous sites. 617 Actinic granuloma-like changes have also been reported (see p. 188). 648
Ochronosis. An irregularly shaped deposit is present in the mid dermis. (H & E)
In hydroquinone-induced pigmentation there is usually diminution in basal melanin, but prominent melanin in macrophages in the papillary dermis. In lesions induced by antimalarial drugs, the changes are usually different, with small pigment granules which are predominantly in macrophages in a perivascular position and around appendages.621. and 640. Small ocher-colored fibers can be present throughout the dermis, but large fibers in the upper dermis are not a feature. The pigment in the antimalarial-induced cases usually stains positively for melanin and hemosiderin, 621 while in the other forms the fibers and smaller deposits are usually negative with these stains and also with elastic tissue stains. 625 They do, however, stain darkly with methylene blue. 626
Tattoos are produced by the mechanical introduction of insoluble pigments into the dermis. In one telephone study reported recently from the United States, 24% of respondents had tattoos,649. and 650. while an almost identical incidence was obtained in a survey of university undergraduates. 651 Most tattoos are decorative in type, but occasionally carbon or some other pigment is traumatically implanted in an industrial or firearm accident.652. and 653. The incidence of complications is becoming quite rare with the declining use of mercury salts (although other red tattoo pigments may cause reactions)654. and 655. and a greater emphasis on hygiene in tattoo parlors.
The complications have been well reviewed.656.657. and 658. They may be grouped into several broad categories: infections introduced at the time of tattooing; cutaneous diseases that localize in tattoos, often in a Koebner-type phenomenon; allergic reactions to the tattoo pigments; 659 photosensitivity reactions;658. and 660. tumors; and miscellaneous reactions. The infections reported have included pyogenic infections, syphilis, leprosy, tuberculosis, 661 tetanus, chancroid, verruca vulgaris,657.662.663.664. and 665. vaccinia, herpes simplex and zoster, molluscum contagiosum, 666 viral hepatitis, and a dermatophyte infection. 667 Cutaneous diseases that may localize in tattoos include psoriasis, lichen planus, 668 Darier’s disease, and discoid lupus erythematosus, the latter in the red areas. 658 Allergic reactions can occur to mercury, 669 chromium,670. and 671. manganese, 672 aluminum, 673 cobalt, and cadmium salts.658.674. and 675. Photosensitivity reactions may be photoallergic or phototoxic, the latter reaction being quite common with cadmium sulfide, a yellow pigment. 674 The development of tumors such as basal cell676. and 677. and squamous cell carcinomas, melanoma, keratoacanthoma, lymphoma, 678 and reticulohistiocytoma may well be coincidental. 656 Miscellaneous lesions include keloids, 657 regional lymphadenopathy, and a sarcoidal reaction which may be localized or systemic.679.680. and 681.
Temporary henna tattoos are becoming more popular, especially among teenagers. 682 Allergic and irritant reactions have been reported but most reactions occur when henna is used in combination with other coloring agents.682.683.684.685.686. and 687. Another recent fad has been the use of cosmetic tattooing (permanent makeup) applied to the lips, eyelids, and eyebrows. Complications have been reported. 688
Recent experimental work with guinea pigs suggests that the lightening of tattoos after laser therapy results more from widespread necrosis and subsequent tissue sloughing and dermal fibrosis than from any specific changes in the pigment or its handling by macrophages. 689 Other mechanisms appear to be involved with some of the newer lasers.690.691. and 692. Some tattoo inks can be difficult to remove.693. and 694. The presence of titanium dioxide in the inks is associated with a poor response to laser therapy. 695 Topical tacrolimus has been used successfully to treat a lichenoid tattoo reaction, 696 and etanercept to treat a granulomatous reaction. 697 Tattoo removal using traditional therapy may result in adverse reactions. 698
Tattoo pigments are easily visualized in tissue sections. After several weeks they localize around vessels in the upper and mid dermis in macrophages and fibroblasts (Fig. 14.26). Extracellular deposits of pigment are also found between collagen bundles. The pigment is generally refractile, but not doubly refractile. A foreign body granulomatous reaction has not been recorded except in the presence of other severe reactions.
Tattoo. Black pigment is seen in macrophages and lying free in a predominantly perivascular location. (H & E)
Hypersensitivity reactions in tattoos vary from a diffuse lymphohistiocytic infiltrate in the dermis (Fig. 14.27), with an admixture of some plasma cells and eosinophils, to a lichenoid reaction,700.701. and 702. sometimes with associated epithelial hyperplasia.675.703. and 704. Red tattoo pigment is often implicated in producing lichenoid reactions.691. and 705. A lichenoid reaction has also been reported following a temporary tattoo containing henna and p-phenylenediamine. 686 Other reactions include the development of sarcoidal granulomas, a granuloma annulare-like reaction, a vasculitis,706. and 707. and a pseudolymphomatous pattern.703.708.709.710. and 711. Scarring may be present. A morphea-like reaction developed in one case. 712 Epidermal spongiosis and pseudoepitheliomatous hyperplasia have been reported.699. and 713. The occurrence of a compound melanocytic nevus along the ink lines of a tattoo were hypothesized as being due to multiple autografts of nevus cells from a pre-existing benign nevus, during the creation of the tattoo. 714
Tattoo pigment with an associated inflammatory reaction, the result of an allergic reaction to one of the pigments. (H & E)
The pigment deposits that are traumatically implanted in the skin during an industrial or other accident are usually more variable in size, and often larger than the deposits introduced in decorative tattoos (Fig. 14.28). Sometimes, the pigment in accidental tattoos is found in the mid dermis.
Non-decorative tattoo. The coarse deposits were impregnated into the skin in a work injury. They are more variable in size than the pigment in a decorative tattoo. (H & E)
Recently, attempts have been made to correlate the ultrastructural features with the pigment used, as determined by X-ray microanalysis techniques. 715 The pigment present in macrophages may be granular or crystalline. 715 It is sometimes membrane bound. Tattoo pigment has also been found in dermal fibroblasts. 716
Hemochromatosis is a multisystem disorder of iron metabolism in which cutaneous pigmentation is a manifestation in up to 90% of patients (‘bronzed diabetes’).717. and 718. Although generalized, the pigmentation is most obvious on the face, especially the forehead and malar areas. 718 Some patients have been reported to have a slate-gray color, rather than the typical bronze pigmentation. 718 Cutaneous pigmentation fades slowly with venesection of the patient.
The bronze color results from increased melanin in the basal layers of the epidermis and, to a lesser extent, some coexisting thinning of the epidermis. 717 Patients with a slate-gray color have been reported to show hemosiderin deposits in the epidermis as well as the dermis, and it is assumed that the epidermal hemosiderin contributes to the skin color in these patients. 718 The absence of pigmentation in the vitiliginous areas of patients with both vitiligo and hemochromatosis indicates that hemosiderin in the usual dermal sites does not contribute significantly to the bronze color in patients with hemochromatosis. 719 Pigment changes are not as apparent in dark-skinned races, although the darkening of pre-existing epidermal cysts, due to increased melanin in their walls, or of keloids may be a useful marker. 720
The increased melanin production is thought to result from the deposition of hemosiderin in the skin, as other heavy metals will produce a similar response. The mechanism by which the heavy metals stimulate melanin production is uncertain.
There may be some thinning of the epidermis and increased melanin pigment in the basal layer. Golden brown granules of hemosiderin are present in the basement membrane region of the sweat glands and in macrophages in the loose connective tissue stroma of these glands. A small amount can often be seen associated with sebaceous glands and their stroma. In some cases, small specks of hemosiderin can be seen in the epidermis with Perls’ stain.718. and 722.
Hemosiderin has also been noted in the skin following the application of Monsel’s solution (20% aqueous ferric subsulfate) for hemostasis in minor surgical procedures,723.724. and 725. and the use of iron sesquioxide on a skin ulcer. 726 In both circumstances there has been ferrugination of collagen fibers with numerous siderophages724. and 725. and sometimes multinucleate giant cells726 in the interstitial tissues of the dermis. Perls’ stain has been strongly positive in these areas.
Hemosiderin is conspicuous in venous stasis of the lower legs. 727 It is found in the pigmented purpuric dermatoses, Zoon’s balanitis and Zoon’s vulvitis, granuloma faciale, and the pigmented pretibial patches of diabetes mellitus. Impregnation of iron from earrings and metallic foreign bodies has been reported.728.729. and 730. Ferruginous foreign bodies may be clinically mistaken for melanomas. 729 Hemosiderin is also present around glass fragments in the dermis (Fig. 14.29), and in dermatofibromas and various tumors of blood vessels.
Hemosiderin deposits around fragments of glass in the dermis. (H & E)
‘Bronze baby’ syndrome refers to the transient bronze discoloration of the skin, serum, and urine which is a relatively uncommon complication of phototherapy for neonatal hyperbilirubinemia.731. and 732. The pigment is thought to be either a photo-oxidation product of bilirubin or a copper-bound porphyrin; it may even be biliverdin. 732 No histological studies have been undertaken.
Localized green discoloration of the palms and soles has been reported in an adult with hyperbilirubinemia. 733
Argyria, which refers to the systemic deposition of silver salts, is an iatrogenic disease resulting from the indiscriminate ingestion of silver-containing compounds or their application to mucous membranes or burnt skin.734.735.736. and 737. Now that the availability of these preparations is restricted, argyria should be rare and seen only in relation to industrial exposure. 738 However, bizarre dietary fads and the availability of colloidal silver preparations on the internet as part of alternative health treatments has led to a resurgence in the incidence of this disease.739.740.741.742.743.744.745. and 746.
Cutaneous changes of argyria consist of permanent blue-gray pigmentation, resembling cyanosis, which is most marked in sun-exposed areas. 747 The nail lunulae may be azure blue.747. and 748. The pigmentation is thought to result from the photoactivated reduction of the absorbed silver salts to metallic silver.739. and 749. There is probably some contribution from increased melanin production as well.
Localized argyria has been reported after prolonged topical exposure,750. and 751. at the site of implanted acupuncture needles,752.753. and 754. and from the wearing of silver earrings in pierced ears. 755
There are multiple, minute, brown-black granules deposited in a band-like fashion in relation to the basement membranes of sweat glands. They are also found in elastic fibers in the papillary dermis and to a lesser extent in the connective tissue sheaths around the pilosebaceous follicles (Fig. 14.30), in the arrector pili muscles and in arteriolar walls. On dark-field examination, the deposits are more easily detected, giving a ‘stars in heaven’ pattern. 756 In one case of localized argyria the deposits were in the papillary dermis adjacent to the intraepidermal sweat duct. 750 Localized argyria may also present with ocher-colored, swollen and homogenized collagen bundles resembling those seen in ochronosis. 757 There is usually an increase in melanin pigment in the basal layer of the epidermis, and melanophages are present in the papillary dermis.
Argyria. There are fine silver particles along the connective tissue sheath of the hair follicle. The patient worked in a silver mine. (H & E)
Scanning electron microscopy has shown that the granules are larger and more abundant in exposed than non-exposed skin. 739 Transmission electron microscopy shows electron-dense bodies 13–1000 µm in diameter in relation to sweat glands and the microfibrils of elastic fibers.740.756.758. and 759. The granules are found in macrophages in membrane-bound aggregates.739. and 740. Histochemical studies suggested that the deposits were in the form of silver sulfide; 760 the recent use of X-ray probe microanalysis has confirmed the presence of silver and sulfur, with the addition of selenium and other metals in trace amounts.734. and 740.
Rarely, silver nitrate staining of the skin may be mistaken for a melanocytic lesion and removed. The author has seen such a case involving a colleague (Fig. 14.31).
Silver nitrate pigmentation of the stratum corneum. This lesion was removed because of clinical suspicion of a melanoma. (H & E)
Chrysiasis refers to the permanent blue-gray pigmentation of the skin, most pronounced in sun-exposed areas, which results from the deposition of gold salts in the dermis, following gold injections for the treatment of rheumatoid arthritis and pemphigus.734.761.762.763. and 764. Its development is, in part, dose related, but light exposure and even laser therapy appear to favor its deposition.765.766.767. and 768.
Besides chrysiasis, gold injections may produce a non-specific eczematous or urticarial reaction, eruptions resembling lichen planus and pityriasis rosea and, rarely, erythema nodosum or erythroderma.769. and 770.
Small round or oval black granules, irregular in size, are present in dermal macrophages which tend to localize around blood vessels in the upper and mid dermis. Similar pigment may be in elongated, fibroblast-like cells in the upper dermis. 762 The gold is well visualized on dark-field examination. A striking orange-red birefringence can be demonstrated under polarized light. 772 The granules are larger than silver granules and, unlike argyria, there is no deposition of gold on membranes.
Now that mercury-containing ointments are no longer commonly used, the slate gray pigmentation of the skin related to the topical application of mercury salts is rarely seen.761.775.776.777. and 778. Another manifestation of mercury intoxication which is rarely seen is acrodynia (pink disease), a condition of early childhood attributed to chronic mercury ingestion in teething powders.779. and 780. Acral parts assume a dusky pink color. Serious systemic symptoms and even death sometimes ensue. Cutaneous nodules containing globules of mercury have been reported in one patient, as a reaction to oral mercury. 781 With the increasing consumption of mercury-polluted seafood, papular and papulovesicular eruptions are being seen. 782
A widespread allergic reaction (mercury exanthem) may follow exposure to high concentrations of mercury vapor783 or the topical application of mercury-containing ointments. 784 Local sclerosing granulomatous lesions may follow the implantation of mercury associated with skin trauma from a broken thermometer, 785 self-injection, 786 or temporary henna tattoos. 787
The pigmentation from topical applications of mercurial preparations results from the deposition of brown-black mercury granules in aggregates of up to 300 µm in macrophages around blood vessels in the upper dermis and in linear bands following the course of elastic fibers. 734 The particles are refractile. There may be a contribution from increased melanin in the basal layer. 789
The mercury exanthem shows subcorneal neutrophilic microabscesses with a variable perivascular neutrophilic and lymphocytic infiltrate around vessels in the upper dermis.
The accidental or deliberate implantation of mercury into the skin results in a granulomatous foreign body giant cell reaction.786. and 790. A zone of degenerate collagen often surrounds the black spherules of mercury in the tissues.785.786. and 791. In older lesions there may be fibrosis around the deposits. 785 Ulceration or pseudoepitheliomatous hyperplasia may overlie dermal deposits of mercury.
Particles averaging 14 nm in diameter, but forming larger aggregates, are present in the dermis.
Prolonged ingestion of arsenic may result in a diffuse, macular, bronze pigmentation, most pronounced on the trunk with ‘raindrop’ areas of normal or depigmented skin. 734 The color is said to arise partly from increased melanin in the basal layer and partly from the metal itself. Other manifestations of chronic arsenical poisoning include keratoses, hyperkeratosis of the palms and soles, and carcinomas of the skin. Periungual pigmentation developed in some of the survivors of an incident involving the ingestion of arsenic-laced curry at a community festival. 792 In the acute stage, facial edema, flushing, and conjunctival hemorrhages were common. 792
Persistent subcutaneous nodules are a rare complication of the use of aluminum-adsorbed vaccines in immunization procedures.794.795. and 796. The nodules may be painful or pruritic.794. and 795. Aluminum salts used in tattooing rarely cause a granulomatous reaction in the skin. 673 An aluminum ‘tattoo’ can also result from the use of topical aluminum chloride in the cauterization of biopsy sites and from the insertion of a dental prosthesis.797. and 798. Drysol (aluminum chloride) is now being used as a hemostatic agent for minor surgical procedures. 799 Contact sensitivity, and a pseudolymphomatous reaction at vaccination sites due to aluminum-containing vaccines, have also been reported.800. and 801. Speckled pigmentation of the lower legs has been reported following the implantation of metallic particles in the skin associated with welding. 802 Aluminum was one of several different metals present.
The nodular lesions show a heavy lymphoid infiltrate in the lower dermis and subcutis with well-formed lymphoid follicles, complete with germinal centers. The infiltrate around the follicles includes lymphocytes, plasma cells, and sometimes eosinophils. Macrophages with slightly granular cytoplasm which stains purple-gray with hematoxylin and eosin are usually present. 795 Giant cells and small areas of necrosis are sometimes seen. The aluminum can be confirmed by X-ray microanalysis795 or by the solochrome-azurine stain in which crystals of aluminum salts stain a deep gray-blue color.
Aluminum ‘tattoos’, following the topical application of aluminum chloride, contain variable numbers of macrophages with ample stippled cytoplasm, resembling the parasitized macrophages of certain infectious diseases. The particles are, however, larger and more variable in size than parasites. 797 An underlying scar is usually present. Following the use of Drysol, there are individual and clusters of macrophages with abundant cytoplasm. They contain aluminum. 799
Zinc deposition has been reported on the lip, following the use of a zinc oxide-containing sunblock for a period of several days. 804 It presented as a well-demarcated dark black macule with an uneven edge. Histological examination showed the submucosal deposition of fine golden yellow granules, predominantly in a superficial location and in a linear fashion upon the extracellular matrix, especially on elastic fibers. 804 Some concentration of the zinc granules was also seen around blood vessels.
Beryllium is one of the lightest metals and it is used as an alloy with other metals. Pulmonary granulomas are a serious complication of prolonged industrial exposure. Although it does not produce cutaneous deposits, it is included here because it produces irritant contact dermatitis, allergic contact dermatitis, chemical ulcers, ulcerating granulomas, and allergic granulomas. 805 The granulomas are usually confluent and sarcoidal in type with some central fibrinoid necrosis. 805
Generalized pigmentation resembling argyria may follow systemic use of bismuth. Metallic granules are present in the dermis. 734 Crops of small black carbon-like particles have been reported on the skin after prolonged ingestion of a bismuth subsalicylate preparation. 806 It has been suggested that prurigo pigmentosa, a condition seen mostly in Japan, is a persistent lichenoid reaction to bismuth with postinflammatory melanin incontinence and pigmentation of the skin. 807
Exposure to titanium dioxide may produce cutaneous lesions.808. and 809. There is one report of a patient developing small papules on the penis following the application of an ointment containing titanium dioxide for the treatment of herpetic lesions. 808 Another report of occupational exposure documents involvement of the lungs, skin, and synovium. 809 In the case involving the topical application, numerous brown granules, confirmed as titanium by electron probe microanalysis, were present in the upper dermis, both free and in macrophages. 808 In another case, a necrotizing lesion involving the subcutis, with extension into muscle, was present. 809 Granulomatous reactions to a titanium alloy used in ear piercing and to titanium screws in a hip replacement have also been reported.810. and 811.
A number of mechanisms are involved in the cutaneous pigmentation induced by certain drugs. These include an increased formation of melanin, the deposition of the drug or complexes derived therefrom in the dermis, and postinflammatory pigmentation, with melanin incontinence, usually following a lichenoid reaction.761. and 812. The exact mechanism is still unknown in many cases. Drugs, therefore, share many features with the heavy metals already considered. This subject has been well reviewed. 734
The long-term use of antimalarial drugs, either for malarial prophylaxis or in the treatment of various collagen diseases and dermatoses, can result in cutaneous pigmentation. 813 Several patterns are seen.734. and 814. Yellow pigmentation is sometimes seen with quinacrine (mepacrine), although the histopathology has not been described. Small ochronosis-like deposits are a rare finding. Pretibial pigmentation is more common and this is slate gray to blue-black in color. Pigment granules – some staining for hemosiderin, some for melanin and some for both – can be seen in macrophages and extracellularly. 640
Prolonged use of phenothiazines produces a progressive gray-blue pigmentation in sun-exposed areas. 815 Slow fading occurs with cessation of the drug. 816 Similar cutaneous pigmentation has been reported in patients taking imipramine817.818.819.820. and 821. and in one taking desipramine. 822 Refractile, golden-brown pigment with the staining properties of melanin is found in the dermis along collagen bundles and in macrophages, especially around vessels in the superficial vascular plexus.734. and 819. The Perls’ method for iron is negative. Electron microscopy shows melanin granules in macrophages but also other bodies of varying electron densities which may represent metabolites or complexes of the drug.823. and 824.
Bluish pigmentation of cutaneous osteomas, and bluish-green pigmentation in areas of trauma on the lower legs have resulted from the use of tetracycline.825. and 826. Rarely, pigmentation of acne scars on the face occurs. 827 The use of doxycycline in suprapharmacological doses (by a psychotic patient) resulted in cutaneous hyperpigmentation resembling that seen with minocycline. 828
The prolonged use of the antibiotic methacycline produces gray-black pigmentation of light-exposed areas and some conjunctival pigmentation in a small percentage of patients. 734 In addition to increased melanin in the basal layer of the epidermis there is extracellular pigment in the elastotic sun-damaged areas which stains positively with the Masson–Fontana method for melanin. 829 Some of this pigment is in macrophages.
Five different patterns830. and 831. of cutaneous pigmentation may follow long-term therapy with the antibiotic minocycline:
Combinations of these patterns are not uncommon. 835 Blue perspiration has also been reported. 839 In patients with atopic dermatitis diffuse cutaneous pigmentation results from relatively short-term minocycline therapy, 3–28 days. 840
A case involving the lips and one involving the tongue have been reported.841. and 842. The sclerae may be involved in severe cases. 843 Rare cases of P-ANCA positive cutaneous polyarteritis nodosa have been reported as a possible complication of minocycline therapy. 844
The pigmentation in all cases gradually fades after cessation of the drug.834. and 845. Laser therapy has been used in cases of incomplete disappearance of the pigmentation. 846
The pigment in the localized types is present in macrophages, often aggregated in perivascular areas, in dermal dendrocytes847 and in eccrine myoepithelial cells. 848 In other cases the pigment may deposit on elastic fibers or lie free in the dermis. 849 It has also been seen in a localized capillaritis of the legs. 850 This complex pigment is positive with both the Perls’ method for iron and the Masson–Fontana method for melanin (Fig. 14.32), but is negative with the PAS stain. 851 Iron was absent from the deposits in the proposed type IV pigmentation of acne scars (see above). 835 It has also been absent from cases in which minocycline pigmentation was isolated to the subcutaneous fat of the lower extremity.836. and 837. Green-gray, flocculent, non-refractile globules were present in macrophages in the subcutis in these cases. 837 It is non-birefringent and non-fluorescent.
Minocycline pigment deposited on dermal elastic fibers. (Masson–Fontana)
Amiodarone, an iodinated benzofuran derivative used in the treatment of cardiac arrhythmias, produces slate-gray discoloration of sun-exposed areas in those patients on prolonged high-dose therapy.855.856.857.858. and 859. It affects 1–2% of those taking the drug. 859 Cutaneous photosensitivity is a more common complication of the drug. The pigmentation slowly disappears after cessation of the drug. 856 Basal cell carcinoma has been reported after amiodarone therapy, but this may be a chance association. 860 Brown granules, staining positively with the Masson–Fontana stain, are present in dermal macrophages. The pigment was originally thought to be lipofuscin, although melanin-containing complexes may also be present. 859 Recently, this concept has been challenged following the finding that amiodarone itself was deposited in the skin. 861
Polyene antibiotics such as nystatin may also produce local lipofuscinosis.855. and 857. The mechanism responsible for the production and deposition of the lipofuscin is unknown for both these drugs.
Localized lipofuscinosis has also been reported as an incidental phenomenon. 862 There was no history of trauma or the application of topical agents.
The substituted phenazine dye clofazimine is used in the treatment of leprosy, discoid lupus erythematosus, and other dermatoses. A not uncommon side effect is the development of cutaneous and conjunctival pigmentation which has a reddish blue hue.761. and 864. Although light microscopy of routine hematoxylin and eosin-stained sections fails to show the pigment, birefringent red clofazimine crystals can be seen in fresh frozen sections. 864 These deposits, which are concentrated around larger vessels in the dermis, are vivid red on fluorescence microscopy. 864
Omeprazole, a potent inhibitor of gastric acid secretion, has been associated with cutaneous pigmentation, mimicking ashy dermatosis. 865 The pigmentation had cleared 12 months after cessation of the drug. A biopsy revealed a normal epidermis and numerous macrophages containing golden-brown granules, mainly located around blood vessels in the upper dermis. The granules stained positively with the Masson–Fontana stain but were negative for iron. Sulfur-containing material, representing the drug and/or drug–melanin complexes were found in the cytoplasm of the macrophages. 865
Pigmentation of the skin may follow the prolonged use of several antineoplastic chemotherapeutic agents including busulfan, bleomycin, doxorubicin, daunorubicin,866. and 867. fluorouracil, 868 cisplatin,869. and 870. cyclophosphamide, and the topical application of mechlorethamine (chlormethine, mustine) and carmustine (BCNU).734. and 871. That following the use of bleomycin takes the form of ‘flagellate streaks’.872.873.874.875.876. and 877. Localization in striae distensae, areas of pressure, and in supravenous skin following venous infusions has been reported.878.879.880.881. and 882. Cisplatin has produced periungual hyperpigmentation. 870 The pigmentation appears to result from increased melanin in the basal layer of the skin and in macrophages in the upper dermis. In the case of daunorubicin hyperpigmentation, complete disappearance has been reported 8 weeks after cessation of the therapy. 867
Over the years, various agents have been injected or surgically implanted into the dermis and subcutaneous tissue as a cosmetic procedure to correct defects and scars and to augment tissues. 883 Paraffin was one such substance, although its complication, ‘paraffinoma’ (see p. 473), is rarely seen these days.799.884.885.886.887.888. and 889. Squamous cell carcinoma is a rare complication of a paraffinoma. 890 Bovine collagen and silicone are the agents used most frequently for these purposes. Other substances, such as gelatin matrix, polymethacrylates and acrylic hydrogels such as Artecoll and Dermalive, and polyvinylpyrrolidone-silicone suspensions such as Bioplastique, polyalkylimide fillers such as Bio-Alkamid, 891 and stabilized hyaluronic acid have been introduced recently and it can be expected that others will be marketed in the future.799.883.892.893. and 894. Adverse reactions to these substances in their current form are uncommon, but granulomatous inflammation has been reported even to hyaluronic acid products.892.893.895.896. and 897. The various adverse cutaneous reactions to these soft tissue fillers was published in 2008. 898 A favorable effect of the injection of crosslinked hyaluronic acid is its stimulation of collagen synthesis, partially restoring dermal matrix components that are lost in photodamaged skin. 899 The hemostatic agent gelfoam is fully absorbed in 4–6 weeks, but if biopsies are done prior to this period, the characteristic collapsed net-like or honeycombed deposits will be seen. 799 The material is basophilic. An excellent review of dermal filler materials and botulin toxin was published in 2001. 900
Hydroxyethyl starch, a key component in many colloid volume expanders used in the treatment of hypovolemic shock and otological disease, commonly produces pruritus. 901 Histopathology reveals multiple cytoplasmic vacuoles in dermal macrophages, endothelial cells, and perineural cells. 901
Suture material, another implant, produces a fairly stereotyped reaction with macrophages, foreign body giant cells, and some lymphocytes. In the case of absorbable sutures, collections of macrophages with brown, foamy cytoplasm often remain after absorption is complete. 902 The morphological appearances of various suture materials in tissue sections were reviewed some time ago. 902 A brief account of the reactions to silicone and to bovine collagen follows.
The term ‘silicone’ is used to designate certain polymeric organosilicon compounds which may be in liquid, gel, or solid form.883. and 900. A liquid form, dimethicone (dimethylpolysiloxane), is used to augment soft tissues. Little reaction is produced if only small amounts (less than 1 ml at each treatment session) are used; 883 severe reactions with granulomas and ulceration have been reported.903. and 904. In an attempt to reduce the side effects that result from the use of large amounts of the liquid or gel forms, ‘bag-gel’ implants were introduced for augmentation of the breasts. 905 Leakage of silicone can occasionally occur following trauma to the site of implantation, producing a local reaction; uncommonly, the silicone gel can migrate to distant sites where it may result in induration or a discharging wound.905.906.907.908. and 909. A lupus miliaris-like reaction on the face has been reported in a patient with silicone breast implants. 910 Ulceration has also been recorded overlying areas of subcutaneous injection of liquid silicone. 911 Silicone has also been used to construct auricular prostheses. 912
Controversy surrounds the development of systemic manifestations, such as scleroderma, in patients who have received silicone implants (see p. 313). Some of these cases have been the subject of litigation.
Silicones can produce a range of histological reactions, depending mainly on the form of the silicone (liquid, gel, or solid elastomer type) and the amount in the tissues. 905 Liquid silicone results in round to oval vacuoles of varying size surrounded usually by histiocytes, some with foamy cytoplasm (Fig. 14.33). A few multinucleate giant cells may be present. 914 Small amounts of the gel form may remain in tissue sections after processing but the liquid forms are usually removed during paraffin processing, leading to the appearance of empty vacuoles. 905 A variable fibroblastic response ensues. 883 Artecoll and Dermalive, two new injectable esthetic microimplants, can also produce a granulomatous reaction. 892
Silicone deposits with characteristic vacuoles of varying size surrounded by macrophages and foreign body giant cells. (H & E)
The reaction to silicone elastomer (silicone rubber), as used in joint prostheses, is strikingly different from that to liquid and gel forms of silicone and takes the form of foreign body granulomas. 905 The implant is sometimes extruded. 915
Although earlier reports suggested that silicone is doubly refractile when examined with polarized light, 916 it is now thought that this property results from adulteration of the silicone with other material. 905 Talc deposition is sometimes seen with polarized light in these cases. 917 It is possibly introduced at the time of the implant surgery.
The injection of bovine collagen (Zyderm®) is a relatively safe procedure used to correct defects caused by acne scars, trauma, and aging.883. and 918. Adverse reactions in the form of erythema, urticaria, abscess formation, and induration of the injection site are relatively uncommon.918. and 919. Granulomatous reactions are rare (see below).920. and 921. There is a theoretical risk of prion transmission when materials of bovine origin are used. No such complication has yet been reported. 922
The mechanism of action of the implant appears to be to stimulate the deposition of new collagen by fibroblasts, which are increased in the vicinity of the implant.
Bovine collagen matrix, another bovine collagen product, is used to promote hemostasis in surgical wounds. It promotes the migration and attachment of stromal and epithelial cells, thereby accelerating wound healing. 923 Other implant materials are constantly being evaluated. 924
The bovine collagen commercially available as Zyderm® is composed mainly of type I collagen of relatively small fiber diameter. It can be recognized in tissues for several weeks after its injection as finely fibrillar material between the larger bundles of native collagen. In contrast to native collagen, which is birefringent under polarized light and which stains green with Masson’s trichrome stain, bovine collagen fails to refract polarized light, stains a pale gray-violet color with Masson’s trichrome stain and is only lightly eosinophilic in hematoxylin and eosin preparations. 925 Bovine collagen is apparently absorbed as it can no longer be detected by light microscopy or immunofluorescence techniques once several months have passed. 926
Following injection of the material, a mild lymphocytic and histiocytic infiltrate is found around blood vessels in the vicinity. This is followed by a slight increase in the numbers of fibroblasts and the subsequent deposition of native collagen. Calcification, which is not uncommon at the site of injection of bovine collagen into animals, has not been recorded in humans. Rare reactions include the formation of foreign body granulomas925. and 927. and abscesses919 or of necrobiotic granulomas resembling granuloma annulare. 920
Granulomatous reactions may also follow the use of hyaluronic acid fillers used for soft tissue augmentation (Fig. 14.34).
Hyaluronic acid filler producing a granulomatous reaction. (H & E with Alcian blue inset)
Oxalate crystals can be found in the skin in some cases of primary oxalosis, a genetically transmitted disorder of oxalate metabolism characterized by hyperoxaluria, nephrolithiasis, nephrocalcinosis, and renal failure at an early age.929.930. and 931. There are two main types of primary hyperoxaluria: type I (OMIM 259900), in which there is a deficiency of the hepatic enzyme alanine-glyoxylate aminotransferase encoded by a gene at 2q36–q37, and type II (OMIM 260000), which has a deficiency of D-glycerate dehydrogenase, the gene for which maps to 9cen. 932 Cutaneous deposits are unusual in secondary oxalosis, which is seen most often in patients with chronic renal failure on long-term hemodialysis. 930 Such patients usually present with miliary deposits in the fingers, particularly on the palmar surface. A patient with multiple subcutaneous nodules and one with dermal plaques on the thigh have been reported.933. and 934. Vascular deposition of oxalate crystals in either the primary or secondary form can produce livedo reticularis935.936. and 937. or cutaneous necrosis.938. and 939. These lesions may resemble calciphylaxis. 932
Oxalate crystals, which are light yellow to brown in sections stained with hematoxylin and eosin, are birefringent. They are rhomboid in shape. They are deposited in the dermis and, rarely, as large nodular deposits in the subcutis. There may be a mild inflammatory reaction with some foreign body giant cells.
As the crystals usually contain calcium salts, they can be stained by the von Kossa method. 930
In cases with livedo reticularis or cutaneous necrosis, oxalate crystals may be found in blood vessels in the subcutis.935. and 938.





