CRANIOFACIALL MICROSOMIA
Craniofacial microsomia, a variable hypoplasia of the skeleton and soft tissue, is the second most common congenital deformity of the head and neck region, with an incidence as high as 1 in 3,500 live births.
The deformity has been known by a variety of terms. In Europe, the term dysostosis otomandibularis has been used. Gorlin and Pindborg preferred hemifacial microsomia, but this term implies that the syndrome is unilateral and that the deformity is confined to the face. I prefer the term unilateral craniofacial microsomia or, when there is bilateral involvement, bilateral craniofacial microsomia.
Bilateral craniofacial microsomia can be confused with Treacher Collins syndrome (
Chapter 28), but the latter shows a well-defined pattern of inheritance and the pathology is relatively symmetrical. Treacher Collins syndrome has other distinguishing features (absence of the medial lower eyelashes, lower eyelid hypoplasia, and antegonial notching of the mandible), findings that are absent in craniofacial microsomia. Likewise, craniofacial microsomia should be distinguished from micrognathia of the development or posttraumatic type where the underdevelopment is restricted to the mandible and there is no evidence of facial paralysis, ear anomalies, or hypoplasia of the soft tissue.
ETIOLOGY
The hypoplasia is variable and can be manifested in any structure(s) derived from the first and second branchial arches (
Table 24.1), accounting for the wide spectrum of the deformity.
The genetics of the syndrome are poorly understood. In a series of 102 affected patients, only 4 had a sibling or parent with evidence of craniofacial microsomia; indeed, only a few pedigrees of the syndrome have been reported. Despite the possibility of an occasional autosomal dominant transmission, only a 2% to 3% recurrence rate was found in a study of first-degree relatives.
Several theories have been proposed in an attempt to understand the etiopathogenesis. Stark and Saunders invoked the concept of mesodermal deficiency, the current theory for cleft lip/palate formation. Tessier, in a classification system of orbitofacial clefts, invoked a clefting mechanism. He described three clefts involving the orbitozygomatic complex in patients with craniofacial microsomia (see
Chapter 26).
The most commonly accepted is one of vascular insult, with hemorrhage formation in the developing first and second branchial arches. The stapedial artery is a temporary embryonic collateral of the hyoid artery. Defects of this temporary vessel may result in hemorrhage, accounting for injury to the developing first and second branchial arches.
Laboratory phenocopies of craniofacial microsomia have been created following the administration of triazine to the developing mouse and thalidomide to the monkey. Histologic studies demonstrated hematoma formation before formation of the stapedial artery. The spectrum of the pathology varied depending on the volume of hemorrhage, ranging from involvement of only the external ear and auditory ossicles to a larger defect involving the zygomatic complex and the entire mandible on the affected side of the mouse model. Moreover, the laboratory findings were supported by the clinical documentation in Germany of approximately 1,000 severe cases and an additional 2,000 less severe cases of craniofacial microsomia following the widespread use of thalidomide as a tranquilizer in pregnant women.
EPIDEMIOLOGY
The incidence of the syndrome is not accurately known in the United States but has been reported to be as high as 1 in 3,500 live births. If all infants with preauricular skin tags and so-called
isolated microtia are included, the incidence of maldevelopment of the first and second branchial arches is much higher.
Similarly, the sex ratio is not accurately known; in a series of 102 patients, 63 were males and 39 were females. Another series reported an almost equal sex ratio (59 males and 62 females). Studies of “isolated” microtia patients, on the other hand, all report a clear male preponderance.
The incidence of bilateral involvement is said to be 10% to 15%. The true incidence is probably higher when one considers the presence of preauricular skin tags and subtle radiographic abnormalities of the mandible on the contralateral, “unaffected” side.
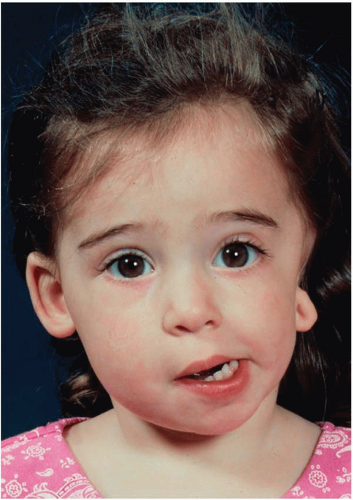
CLINICAL FINDINGS
There is a wide variety of pathologic expression of craniofacial microsomia in the following anatomic regions: jaws, other craniofacial skeletal components, muscles of mastication, ears, soft tissue, and nervous system (
Figure 24.1).
Jaws
The most obvious deformity is the mandible, especially the ascending ramus, which is reduced in the vertical dimension. The size of the condyle usually reflects the degree of hypoplasia of the ramus. Involvement of the temporomandibular joint ranges from mild hypoplasia to a pseudoarticulation at the cranial base to complete absence of the condyle. In addition to being short, the ramus is usually displaced toward the midline.
The chin is deviated toward the affected side and there is a corresponding cant of the mandibular occlusal plane, which is paralleled in the corresponding planes of the maxillary sinus floors and pyriform apertures. Similarly, the maxillary and mandibular dentoalveolar complexes are reduced in the vertical dimension on the affected side.
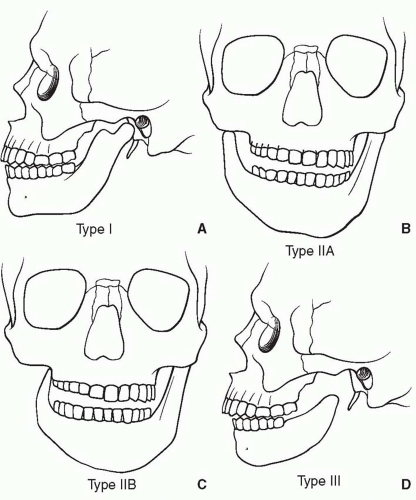
Pruzansky proposed a classification of the mandibular deficiency, which was later modified by Mulliken and Kaban (
Figure 24.2):
Mild hypoplasia of the ramus with minimally affected mandibular body.
The condyle and ramus are small; the head of the condyle is flattened; the glenoid fossa is absent; the condyle is hinged on a flat, often convex, infratemporal surface; the coronoid may be absent.
The ramus is reduced to a thin lamina of bone or is completely absent. There is no evidence of a temporomandibular joint.
The above classification was subsequently modified by subdividing type II based on the pathology of the temporomandibular joint region. In type IIA, although the ramus and condyle are abnormal in size and shape, the glenoid fossa-condyle relationship is maintained. Temporomandibular joint function is almost normal. In contrast, in type IIB, the condyle is hypoplastic and malformed and displaced toward the midline relative to the contralateral side. Patients open with restricted hinge-like functioning of the mandible on the ipsilateral side.
Other Skeletal Components
The maxilla is reduced in the vertical dimension and, depending on the degree of hypoplasia of the mandible, there is a corresponding cant of the occlusal surface of the maxillary dentition.
The zygomatic complex can be reduced in all dimensions; the zygomatic arch can be decreased in length or absent. These findings, combined with soft-tissue deficiency, result in a reduction in the distance between the oral commissure and ear vestige on the affected side.
The temporal bone can also be involved, although the petrous portion is spared. The mastoid process can be hypoplastic and there can be partial or complete lack of pneumatization of the mastoid air cells. The styloid process can be shortened or absent. The orbit is often reduced in all dimensions, and occasional patients have microphthalmos. The frontal bone can be flattened, giving the illusion of a plagiocephaly although the ipsilateral coronal suture is patent.
Malformations of the cervical vertebrae are not uncommon and include the presence of hemivertebrae, fused vertebrae, and even a basilar impression syndrome. Goldenhaar described a variant of craniofacial microsomia characterized by epibulbar dermoids/lipodermoids, associated vertebral abnormalities (usually cervical), and occasional rib anomalies.
Muscles of Mastication
The syndrome is not restricted to the skeleton; the associated muscles of mastication are hypoplastic. The deficiency, however, is not always proportional to the skeletal deficiency. A three-dimensional computed tomography (CT) scan study compared the volume of the mandibular deformity with that of the adjacent muscles of mastication and noted that there was not always a 1:1 relationship in the degree of pathologic involvement.
Muscle function is impaired, especially evident in lateral pterygoid muscle function on the affected side. The lateral pterygoid muscle is responsible for movement of the mandible and chin point to the contralateral side. Consequently, in patients with unilateral craniofacial microsomia, who attempt a protrusive chin movement, the chin deviates to the affected side during opening and during forceful protrusion. The hypoplastic lateral pterygoid muscle on the affected side is overpowered by its unaffected counterpart. Moreover, mouth opening is also adversely affected by the hypoplastic ramus and malpositioned temporomandibular joint.
Ears
Involvement of the auricle occurs in most patients (
Chapter 27). Meurmann proposed a classification of the external ear deformities: Grade I, distinctly smaller malformed auricle but all components are present; Grade II, only a vertical remnant of cartilage and skin with aural atresia (complete atresia of the external auditory canal); Grade III, almost complete absence of the auricle except for a small remnant, usually a soft-tissue lobule. Nagata’s classification (
Chapter 27) is more useful for the surgeon. The great majority of patients with microtia also have aural atresia. A small percentage do have a canal, but in many of these patients the canal is stenotic, atypical, or in abnormal position.
Soft Tissue
On the affected side, preauricular skin tags are common, and the skin and subcutaneous tissue of the cheek show varying degrees of hypoplasia. Hypoplasia or aplasia of the parotid gland has been documented. The soft-tissue deficiency occurs in all three dimensions.
Lateral facial clefts (macrostomia) are common associated findings and also contribute to the overall cheek hypoplasia.
Overt clefts of the soft palate are said to occur in 25% of patients, and the soft palate may deviate to the affected side on voluntary function.
Nervous System
Cerebral abnormalities, although rare, can occur and include hypoplasia of the cerebrum and corpus callosum, as well as hydrocephalus of the communicating and obstructive types. The brain stem can be involved secondarily because of anomalies of the cervical vertebrae, resulting in disturbances such as impression of the brain stem.
The most common cranial nerve anomaly is an incomplete facial palsy of varying degrees, attributed to the following (alone or in combination): absence of the intracranial portion of the facial nerve and nucleus in the brain stem, aberrant pathway of the nerve in the temporal bone, or agenesis of the facial muscles. Absence of facial nerve function in the distribution of the marginal mandibular branch is seen in approximately 25% of patients, with weakness of other components, such as the buccal and zygomatic branches, occurring in a smaller percentage.
CLASSIFICATION
Several classifications have been described based on the clinical findings of the patient with unilateral craniofacial microsomia. Harvold, Vargervik, and Chierici proposed the following classification:
I (A). The classic type characterized by unilateral facial underdevelopment without microphthalmos or ocular dermoids but with or without abnormalities of the vertebrae, heart, or kidneys.
I (B). Similar to type I (A) except for the presence of microphthalmos.
I (C). Bilateral asymmetric type in which one side is more severely involved.
I (D). Complex type that does not fit the above but does not display limb deficiency, frontonasal phenotype, or ocular dermoids.
II. Limb deficiency type (unilateral or bilateral) with or without ocular abnormalities.
III. Frontonasal type. Relative unilateral underdevelopment of the face in the presence of hypertelorism with or without ocular dermoids and vertebral, cardiac, or renal abnormalities.
IV. (A) Unilateral or (B) bilateral. Goldenhar type with facial underdevelopment in association with other dermoids, with or without upper lid coloboma.
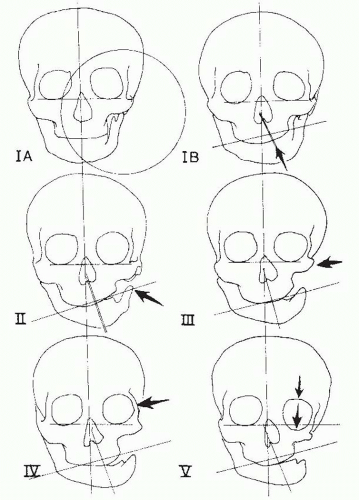
Munro and Lauritzen proposed a clinical classification system (
Figure 24.3) that was designed as an aid in planning surgical correction:
Type IA: The craniofacial skeleton is only mildly hypoplastic and the occlusal plane is horizontal.
Type IB: The skeleton is similar to IA, but the occlusal plane is canted.
Type II: The condyle and part of the affected ramus are absent.
Type III: In addition to the findings in type II, the zygomatic arch and glenoid fossa are absent.
Type IV: This is an uncommon type with hypoplasia of the zygoma and medial and posterior displacement of the lateral orbital wall.
Type V: The most extreme type has inferior displacement of the orbit with a decrease in orbital volume.
Vento and colleagues proposed the nosologic OMENS classification system in an effort to standardize reporting between treatment centers. The acronym OMENS designates each of the five major areas of involvement in craniofacial microsomia: O = orbital, M = mandibular, E = ear, N = facial nerve, and S = soft tissue. The orbital gradations were based on size and position; the mandible was scored as noted above;
the ear anomaly was categorized essentially according to the Meurmann classification; the facial nerve was according to which branches were involved, and the soft tissue was according to the degree of subcutaneous and muscular deficiency.
PREOPERATIVE ASSESSMENT
A complete clinical evaluation is mandatory, because other organ systems, such as the kidneys and heart, can be involved. The role of the pediatric otolaryngologist is critical in assessing the airway and auditory function. The patient with airway problems will require endoscopy and sleep studies. Medical photographs are obtained, including frontal, lateral, oblique, submental vertex, and occlusal views. Cephalograms (posteroanterior, lateral, and basilar) and a panoramic roentgenogram (Panorex) are likewise obtained. The optimal way to define the various skeletal deformities is with a three-dimensional CT scan (
Figure 24.4), which can be reformatted to give a dentascan and document the location of tooth follicles in the younger patient in whom cephalograms and Panorex cannot be obtained. i-CAT scans have recently been added as a tool in planning skeletal surgery.