Craniofacial microsomia (CFM) encompasses a broad spectrum of phenotypes. It is thought to result from defective development of the first and second pharyngeal arch structures, and generally presents with anomalies of the mandible and other facial bones, ears, and overlying soft tissues. The cause of CFM is thought to involve both extrinsic and genetic risk factors. Several classification systems have been developed to help stratify patients based on the severity of their defects. Treatment of patients includes repair of bony asymmetry as well as soft tissue defects and auricular anomalies. Surgical intervention is individualized based on each patient’s deficits.
Key points
- •
There are several classification systems for craniofacial microsomia that group patients based on their degree of asymmetry. The most recent and comprehensive of these is the OMENS PLUS (Orbit, Mandible, Ear, Nerve, Soft tissue) system.
- •
Treatment of craniofacial microsomia is based on the severity of the deformity.
- •
Timing of surgical repair remains controversial.
- •
Mandibular distraction osteogenesis is a well-accepted method of correction of mandibular asymmetry but there is evidence of relapse if patients undergo distraction before completion of growth.
- •
Treatment includes not only correction of skeletal deformities but also soft tissue deficits (by means of free tissue flaps, fat grafting, and implants).
Introduction
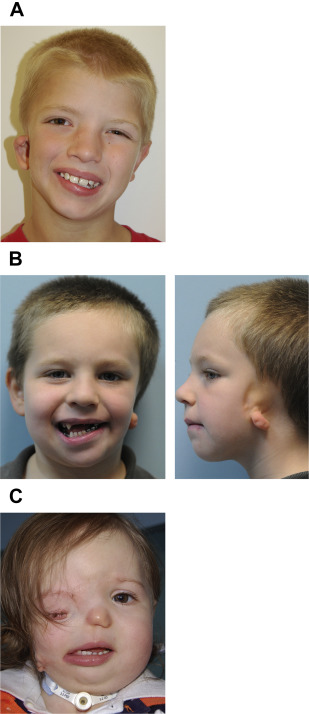
Craniofacial microsomia (CFM) is a term used to describe a spectrum of craniofacial abnormalities caused by abnormal development of the first and second pharyngeal arch derivatives. The term CFM is often used interchangeably with several other terms, including otomandibular dysostosis, lateral facial dysplasia, malformation syndrome of the first and second arches, temporal oculoauricular dysplasia, and hemifacial microsomia (HFM). In addition, Goldenhar syndrome is considered a variant of CFM, which also includes epibulbar dermoids and vertebral anomalies. It is thought that the entities mentioned earlier represent several different phenotypical presentations that exist within a continuum, and thus the term oculoauriculovertebral spectrum (OAVS) was proposed by Cohen and colleagues in 1989 to encompass all of these variants. Each of the variants includes some degree of developmental abnormality of the facial skeleton (mandible, maxilla, zygoma, and/or temporal bone), ear, and soft tissues.
Introduction
Craniofacial microsomia (CFM) is a term used to describe a spectrum of craniofacial abnormalities caused by abnormal development of the first and second pharyngeal arch derivatives. The term CFM is often used interchangeably with several other terms, including otomandibular dysostosis, lateral facial dysplasia, malformation syndrome of the first and second arches, temporal oculoauricular dysplasia, and hemifacial microsomia (HFM). In addition, Goldenhar syndrome is considered a variant of CFM, which also includes epibulbar dermoids and vertebral anomalies. It is thought that the entities mentioned earlier represent several different phenotypical presentations that exist within a continuum, and thus the term oculoauriculovertebral spectrum (OAVS) was proposed by Cohen and colleagues in 1989 to encompass all of these variants. Each of the variants includes some degree of developmental abnormality of the facial skeleton (mandible, maxilla, zygoma, and/or temporal bone), ear, and soft tissues.
Epidemiology
CFM is the second most common craniofacial birth defect after cleft lip and palate. It affects an estimated 1 in 3600 to 5600 live births in the United States each year. Literature reviews suggest that it is 50% more prevalent in boys (3:2 ratio). Ten percent of cases are bilateral, and most unilateral cases occur on the right.
Cause/pathogenesis
The mechanism behind CFM is thought to be related to the development of the pharyngeal arch structures. The pharyngeal arches start to form around the fourth week of embryologic development and are composed of mesenchymal cells that give rise to various facial structures (including skeletal, muscular, and neural elements). The morphogenesis of these structures depends on continuous and reciprocal tissue-tissue interactions, and any disruption of these interactions can lead to developmental abnormalities. There are 2 leading theories to explain the pathogenesis of CFM:
- 1.
Vascular disruption of the stapedial artery during development of the first and second pharyngeal arch derivatives leads to hematoma formation and subsequent abnormal growth and malformation of the mandible.
- 2.
Death, failure of development, or failure of migration of cells from the neural crest to the pharyngeal arches, causing dysmorphology of the arches.
Genetics
The causes of CFM include both extrinsic and genetic risk factors. Most documented cases are sporadic with no relevant family history. However, there is growing evidence for a genetic predisposition. Previously, a positive family history was documented in about 2% of patients who were within the OAVS spectrum. However, recent studies have shown significantly larger numbers of familial cases. It is also hypothesized that the reported percentage of familial involvement is underestimated given the broad phenotypic spectrum, with some family members having mild presentations that go undetected. In a study by Kaye and colleagues, 44% of cases of CFM had a positive family history of facial malformation, with an overall recurrence rate of 2% to 3% in first-degree relatives. Their data favored an autosomal dominant mode of inheritance with incomplete penetrance rather than a recessive or polygenetic mode of transmission.
Several chromosomal abnormalities have been identified in patients with CFM ( Table 1 ). Studies reveal that the 22q11 locus may harbor genes important for regulation of craniofacial symmetry and first and second pharyngeal arch development, because craniofacial skeletal and soft tissue asymmetries have been observed in patients with genomic imbalances on the 22q11 locus. The Crkl gene (in the 22q11 region) regulates signaling events in developing pharyngeal arches, again supporting its potential contribution to craniofacial dysmorphism. The OTX2 gene was also identified as a very likely causal gene in CFM. This gene encodes a transcription factor that plays a critical role in craniofacial development and anterior brain morphogenesis. Zielinski and colleagues investigated the largest CFM pedigree to date and found that a duplication in chromosome 14q22.3 (coding for OTX2) was present in all affected individuals.
| Abnormality | Gene | Type | Reference |
|---|---|---|---|
| 22q11.2 | Crkl | Deletion | Xu et al, 2008; Digilio et al, 2009; Tan et al, 2011 |
| 14q22.3 | OTX2 | Zielinki et al, 2014 | |
| 3q29 | Deletion | Guida et al, 2015 | |
| 14q32 | GCS | Kelberman et al, 2001 | |
| 15q26.2–3 | Huang et al, 2010 | ||
| 1p22.2-p31.1 | Deletion | Callier et al, 2008 | |
| 12p13.33 | Deletion | Rooryck et al, 2010; Adbelmoity et al, 2011 | |
| Trisomy 22 | Kobrynski et al, 1993 | ||
| 14q23.1 | Duplication | Ballesta-Martinez et al, 2013; Ou et al, 2008 | |
| 15q24 | Deletion | Brun et al, 2012 | |
| 5q13.2 | Deletion | Huang et al, 2010 | |
| 5p15.33-pter | Deletion | Descartes et al, 2006; Josifova et al, 2004; Ladekarl et al, 1968; Ala-Mello et al, 2008 | |
| 10p14-p15 | Duplication | Dabir et al, 2006 | |
| 14q31.1–3 | Deletion | Gimelli et al, 2013 | |
| 15q24.1 | Deletion | Brun et al, 2012 | |
| Trisomy 18 | Verloes et al, 1991 | ||
| Deletion 22qter | Deletion | Herman et al, 1988 | |
| 22q11.1–.21 | Duplication | Quintero-Rivera, 2013; Torti et al, 2013 | |
| X chromosome aneuploidies | Garavelli et al, 1999; Poonawalla et al, 1980 | ||
| t(9;18) (p23;q12.2) | Translocations | Rooryck et al, 2010 | |
| inv9(p11;q13) | Inversion | Stanojevic et al, 2000 | |
| inv14(p11.2;q22.3) | Inversion | Northup et al, 2010 | |
| Mosaicism trisomy 7 | Mosaic | Hodes et al, 1981 | |
| Mosaicism trisomy 9 | Mosaic | de Ravel et al, 2001; Wilson et al, 1983 | |
| Mosaicism trisomy 22 | Mosaic | de Ravel et al, 2001 | |
| 8q13 | Cousley et al, 1997 |
Environmental factors are also thought to play a causative role in CFM. It is hypothesized that gestational diabetes, exposure to teratogens such as thalidomide, vasoactive drug use, smoking, and multiple gestation pregnancies cause disruption of embryonic blood flow during fetal development, leading to several structural congenital anomalies.
Presentation
There are no established criteria for diagnosis of CFM. However, several studies have indicated that either mandibular or auricular defects are mandatory for diagnosis. Cousley proposed in his 1993 article the following minimum diagnostic criteria:
- 1.
Ipsilateral mandibular and ear defects (external/middle)
- 2.
Asymmetrical mandibular or ear defects (external/middle) in association with:
- a.
Two or more indirectly associated anomalies, or
- b.
A positive family history of HFM
- a.
There are varying degrees of severity within the spectrum of CFM. Mandibular deficiency can range from missing the condylar cartilage and disc to complete developmental failure of the ramus. The maxilla, temporal bone, and orbit can also be affected as a result of primary malformation. However, CFM is not characterized by bony dysmorphism alone, because there is soft tissue, neural, and muscular involvement as well. Table 2 outlines the anomalies that are seen and their incidence.
| Site | Percentage of Patients (%) |
|---|---|
| Mandibular deficiency | 89–100 |
| Other Bony Anomalies | |
| Maxillary hypoplasia | — |
| Temporal bone deformity | — |
| Orbit | 15–43 |
| Ear anomalies | 65–99 |
| Microtia/anotia | 66–99 |
| Preauricular skin tags | 34–67 |
| Conductive hearing loss | 50–66 |
| Ossicular chain defects | — |
| Pinna abnormalities | — |
| External auditory canal atresia | — |
| Soft tissue defects | 17–95 |
| Masticatory/facial muscle hypoplasia | 85–95 |
| Parotid gland hypoplasia | — |
| Deficiency of subcutaneous tissue | — |
| Transverse oral cleft | 18–61 |
| Cranial nerve involvement | 10–45 |
| Anomalies Outside Head and Neck | |
| Vertebral/rib defects | 16–60 |
| Cardiac defects | 4–33 |
| Renal/genitourinary defects | 4–15 |
| Central nervous system anomalies | 5–18 |
Classification systems
The heterogeneity of phenotypic presentations in CFM has led to difficulty developing a reproducible classification system to distinguish between varying degrees of deformity and to help aid in surgical planning. The first accepted classification was proposed by Pruzansky in 1969, and focused on the size and shape of the mandible and glenoid fossa. Kaban and colleagues modified this classification system in 1988, proposing further stratification of the type II mandible based on the relationship of the mandibular condyle and glenoid fossa ( Fig. 1 ). Another classification system described in the literature is the SAT (skeletal malformations, auricular involvement, and soft tissue defects) system, proposed by David and colleagues in 1987. Vento and colleagues took this one step further, defining the OMENS (Orbit, Mandible, Ear, Nerve, Soft tissue) classification system, which expanded the SAT system to include other affected structures: orbital distortion, mandibular hypoplasia, ear deformities, nerve defects, and soft tissue deficiencies. A modified version has since been published (OMENS PLUS), which is used when noncraniofacial structures are also involved. The hope with these classification systems (outlined in Table 3 ) is that better differentiation of key phenotypical elements will lead to improved diagnosis, treatment planning, prognostic predictions, data evaluation, and case correlation.
| Pruzansky Classification of CFM (1969) | ||
| Grade I | Mandible with mild hypoplasia | |
| Grade II | Mandible with more severe hypoplasia in addition to malformation of common bony landmarks | |
| Grade III | Mandible with complete effacement of common mandibular landmarks (absent ramus, condyle, TMJ) | |
| Pruzansky-Kaban Classification (1988) | ||
| Grade I | Mandible with mild hypoplasia | |
| Grade II | ||
| IIa | Mandibular ramus, condyle, and TMJ are present, normal in shape, but hypoplastic | |
| IIb | Mandibular ramus is hypoplastic and markedly abnormal in form and location (medial and anterior) without articulation with temporal bone | |
| Grade III | Mandible with complete effacement of common mandibular landmarks (absent ramus, condyle, TMJ) | |
| SAT Classification System (1987) | ||
| Skeletal malformations | S1 | Small mandible of normal shape |
| S2 | Mandible very different in size and shape than normal. Condyle, ramus, and sigmoid notch identifiable but distorted | |
| S3 | Mandible severely malformed: ranges from poorly identifiable ramal component to complete agenesis of ramus | |
| S4 | S3 mandible with orbital involvement: posterior recession of lateral and posterior orbital rims | |
| S5 | S4 defect with orbital dystopia, hypoplasia and asymmetric neurocranium, flat temporal fossa | |
| Auricular involvement | A0 | Normal |
| A1 | Small malformed auricle but all features are retained | |
| A2 | Rudimentary auricle with hook at cranial end corresponding with helix | |
| A3 | Malformed lobule and absent remainder of pinna | |
| Soft tissue defects | T1 | Minimal contour defect without cranial nerve involvement |
| T2 | Moderate defect | |
| T3 | Major defect, obvious facial scoliosis, severe hypoplasia of cranial nerves, parotid, muscles of mastication, eye involvement; facial clefts | |
| OMENS Classification (1991) | ||
| Orbit (orbital distortion) | O 0 | Normal orbital size and position |
| O 1 | Abnormal orbital size | |
| O 2 | Abnormal orbital position | |
| O 3 | Abnormal orbital size and position | |
| Mandible (mandibular hypoplasia) | M 0 | Normal mandible |
| M 1 | Small mandible and glenoid fossa | |
| M 2a | Short mandibular ramus but good position of glenoid fossa | |
| M 2b | Short mandibular ramus; TMJ is inferiorly, medially and anteriorly displaced; condyle is hypoplastic | |
| M 3 | Complete absence of mandibular ramus, glenoid fossa and TMJ | |
| Ear (ear anomaly) | E 0 | Normal ear |
| E 1 | Mild hypoplasia and cupping but all structures present | |
| E 2 | Absence of external auditory canal with hypoplasia of concha | |
| E 3 | Malpositioned lobule with absent auricle; lobular remnant inferiorly and anteriorly displaced | |
| Nerve (nerve involvement) | N 0 | No facial nerve involvement |
| N 1 | Upper facial nerve involvement (temporal, zygomatic branches) | |
| N 2 | Lower facial nerve involvement (buccal, mandibular, and cervical branches) | |
| N 3 | All branches of facial nerve involved | |
| Soft tissue (soft tissue deficiency) | S 0 | No obvious soft tissue or muscle deficiency |
| S 1 | Minimal subcutaneous/muscle deficiency | |
| S 2 | Moderate subcutaneous/muscle deficiency | |
| S 3 | Severe soft tissue deficiency caused by subcutaneous and muscular hypoplasia | |
Treatment overview
Treatment of CFM poses a challenging issue because there are both soft tissue and skeletal deficiencies that need to be addressed. Before surgical intervention, computed tomography (CT) with three-dimensional (3D) reconstruction is becoming an increasingly popular imaging modality to better delineate asymmetries. However, the posteroanterior (PA) cephalogram is still the gold standard method for assessing facial asymmetry. With these images, clinicians can measure maxillary and mandibular deviations from midline, differences in ramus height, and occlusal cant. These measures are important in objectively assessing improvements in asymmetry caused by surgical intervention.
The major goals in treating CFM include improvements in facial symmetry, functional jaw movement, occlusion, and patient satisfaction. Kaban and colleagues outlined 4 main treatment objectives:
- 1.
Increase size of mandible and associated soft tissue
- 2.
Create temporomandibular joint (TMJ) if one is lacking
- 3.
Foster vertical maxillary growth
- 4.
Obtain stable occlusion
Surgical timing
Defining the timing of surgical intervention is challenging, because of the controversy as to whether facial asymmetry in these patients progresses over time or remains fixed. In reviewing the literature, there are 2 separate fields of thought:
- 1.
Clinicians who think that the asymmetry is progressive favor early surgical intervention.
- 2.
Clinicians who think that the asymmetry is fixed propose delayed intervention once the children reach skeletal maturity.
Note that both fields of thought agree on early surgical intervention in children at risk for airway compromise because of their mandibular deformity.
Those surgeons who support early correction of asymmetry (before skeletal maturity) believe that mandibular skeletal asymmetry worsens with time, because the affected side has little or no growth. They argue that early intervention allows improved growth potential and functionality of structures by minimizing secondary skeletal deformities caused by limited growth of adjacent structures. In addition, they think that early intervention improves masticatory muscle hypoplasia, optimizes dental development, and affords improved patient aesthetic appearance and body image development.
Those investigators in favor of waiting to correct mandibular asymmetry think that the most favorable aesthetic results come from reconstruction at an age closer to skeletal maturity (age 13–15 years in girls, 15–16 years in boys). They argue that relapse of asymmetry occurs during growth phases, leading to a need for multiple additional procedures. They highlight technical reasons for delaying surgical reconstruction until the permanent dentition phase, noting that procedures performed later have decreased blood loss and other surgical risk factors. Patient compliance also improves in these cases compared with early distraction osteogenesis.
Studies of the outcomes following early and late skeletal correction of CFM vary greatly in terms of results, and most of these studies are small and retrospective, consisting of level IV evidence. Several larger systematic reviews have been conducted to address this issue, and these studies concluded that there was a lack of evidence supporting early skeletal correction in these children. However, some institutions still support early distraction. This article discusses the evolution of surgical treatment of CFM chronologically.
History of treatment
In the days before mandibular distraction osteogenesis (MDO), early mandibular reconstruction was achieved by mandibular osteotomy and autogenous grafting, most frequently using costochondral cartilaginous rib grafting. Dating back to the 1970s, the degree of the deformity in CFM was used to guide treatment. Those children with more severe defects (Pruzansky-Kaban types IIb and III) underwent surgery prepubertally to reconstruct the mandible, whereas treatment of children with milder deformities tended to be more variable. Many were not treated until adolescence or received functional orthodontic appliances, whereas others underwent early mandibular osteotomies to keep up with vertical midfacial growth. Soft tissue deficiencies were usually not addressed until after restoration of bony symmetry.
Modern approach to treatment
Regardless of timing of skeletal repair, the choice of procedure is based on the severity of the defect and degree of deficit of mandibular bone stock. In the meta-analysis by Pluijmers and colleagues, patients with type I deformities were most often treated with MDO. However, elongation and rotation with osteotomy was also used to treat type I and IIa patients. Those with type IIa deformities most commonly underwent MDO and those with IIb deformities most commonly underwent reconstruction with grafts. Type III deformities were most often treated with iliac or costochondral grafting to recreate the TMJ, sometimes followed by MDO.
Grafts
Gillies first described the use of cartilage and bone from the rib cage to address the hypoplastic mandible in the 1920s. Along with providing adequate bony length, the cartilaginous portion of the graft serves as a neocondyle. The most popular graft material used is the costochondral cartilaginous rib graft, followed by iliac crest, interposed temporal bone, and fibula. Its popularity stems from the potential for growth along with its adaptability and workability. However, studies have suggested unpredictable growth patterns and the potential for overgrowth on the treated side. Grafting also has risks, including infection, donor site morbidity, reankylosis, fracture, and resorption.
Follow-up studies of mandibular grafting showed high rates of resorption of graft material and recurrence of asymmetry. Thus, with the advent of MDO, grafts became used mainly in conjunction with distraction or in patients with Pruzansky type IIb and III deformities requiring construction or reconstruction of the TMJ and ramus. Occasionally, grafts were used in type IIa patients as interposed bone to lengthen the affected mandible. However, the normal side outgrew the affected side after elongation in 50% of patients. In addition, patients with costochondral grafting before MDO tended to have higher rates of postoperative complications (44%–68%).
Distraction osteogenesis
Several cases of mandibular corpus distraction were reported in the literature during the first half of the twentieth century, but the technique of MDO did not gain popularity until the early 1990s when McCarthy’s group at New York University began to perform the procedure. The technique was slowly adopted over the following years but became widely accepted with the advent of bidirectional distraction (described by Klein and Howaldt in 1995). The principal aims of MDO are to provide stable expansion of the mandible with concurrent lengthening and expansion of surrounding muscle and soft tissue. Initially, mandibular distraction devices were only external. These devices offered excellent mechanical strength but had some complications, including unsightly pin site scars, pin site infections, and dislodgement of the device. These complications led surgeons to design internal mandibular devices. These devices are inserted through either an oral or external approach and provide excellent mechanical strength. The downsides include the need for removal at the end of the distraction and bony overgrowth on the device, making removal difficult.
Initial studies of MDO revealed some significant advantages compared with costochondral grafting. MDO increased the vertical length of the mandible, produced greater bone stock, improved soft tissue asymmetry by encouraging hypertrophy of the muscles lying parallel to the distraction vector, and had less relapse than costochondral cartilage grafting. In addition, operative times were generally shorter; the complications were fewer; the postoperative course was simpler; and there was less blood loss, greater vector control of advancement, no donor site morbidity, and an ability to lengthen the mandible at a younger age.
Stability of distraction
In the decade following the advent of MDO, studies began to note the need for repeated distraction to maintain symmetry during growth. Molina and colleagues published one of the first of these studies in 1995, of 65 patients with CFM who were treated with early MDO and followed for an average of 19 months postoperatively. Facial development on the unaffected side proceeded normally, whereas the distracted side showed delayed growth, leading to some return of asymmetry. Thus the investigators proposed overcorrection and second-stage distraction.
The concept of overcorrection has since been suggested in multiple additional studies as a method to combat the need for repeated distraction. However, overcorrection has its downsides as well, including creating a dental crossbite on the contralateral side, leading to so-called occlusal disasters. Overcorrection also increases the abnormal form and position of bone and soft tissues, creating a secondary chin malformation, making future genioplasty more difficult. In addition, overcorrection did not reduce the number of surgeries these children underwent.
Increasing support for delayed surgical intervention
Several systematic reviews have been conducted over the past decade of long-term stability of the distracted mandible in patients with CFM. The investigators all commented on the lack of evidence-based data supporting early versus delayed surgical intervention. All of the studies consist of level IV evidence, and many of the studies are flawed in their design, making their data questionable in terms of validity. Table 4 outlines these studies. Conclusions were similar for all 3 systematic reviews:
- •
MDO performed before skeletal maturation leads to relapse of asymmetry, despite overcorrection.
- •
The earlier the correction, the more likely the procedure will need to be repeated.
- •
In addition, there was evidence suggesting adverse effects of MDO on growth of the affected mandible.
| Publication Author | Study Design | Therapy | Follow-up Period | Long-term Outcomes | Conclusions | Level of Evidence |
|---|---|---|---|---|---|---|
| Stability Following Surgery | ||||||
| Kaban et al, 1988 | Retrospective case series (n = 17) | Elongation and rotation by osteotomy vs grafting | 4 y | Stable occlusion with E&R, 50% of grafted mandibles outgrown by normal side | IV | |
| Kearns et al, 2000 | Retrospective case series (n = 67) | Untreated | >13 y | Statistically significant progression of asymmetry from the deciduous to mixed dentition phase in all measurements in group II patients (mandible type IIB or III) | Hemifacial microsomia is progressive; early surgical intervention is warranted | IV |
| Padwa et al, 1998 | Retrospective case series (n = 33) | Grafting | 5.5 y | 16% of patients had significant return of asymmetry as determined by occlusal cant | Proposed overcorrection | IV |
| Molina et al, 1995 | Retrospective case series (n = 65) | Early MDO | 19 mo | Younger patients had faster growth on the unaffected side compared with the treated mandible | Proposed overcorrection and second-stage distraction | IV |
| Molina et al, 2004 | Prospective case series (n = 4) | Early MDO | 12 y | Stable symmetry. In patients <5 y old, secondary occlusal disaster and need for reoperations seen | Stable symmetry | IV |
| Hollier et al, 1999 | Prospective case series (n = 8) | Early MDO | 32.6 mo | Growth of affected vertical ramus slower than the unaffected side in all patients | Proposed overcorrection | IV |
| Grayson et al, 1997 | Retrospective case series (n = 5) | Early MDO | 1–6 y | Increase in height over 5 y of growth is greater on the side that is not distracted | Proposed overcorrection | IV |
| Baek et al, 2005 | Retrospective case series (n = 19) | Early MDO | 2.7 y | Type I and IIa mandibles stable, type IIb and III mandibles with relapse | IV | |
| Cavaliere et al, 2002 | Prospective case series (n = 2) | Early MDO | 1–2 y | Type III mandibles: improvement in contour of affected side, full range of jaw motion. No mention of relapse at end of follow-up | IV | |
| Altug-Atac et al, 2008 | Retrospective case series (n = 11) | Early MDO | 6 mo | Significant improvement in hard and soft tissue asymmetry, no mention of relapse | IV | |
| Kulewicz et al, 2004 | Prospective case series (n = 28) | Early MDO | 3 mo to 1 y | Stable results in lengthening and occlusion after 1 y. Coordinated growth of maxillomandibular complex | Proponent of early correction | IV |
| Shetye et al, 2006 | Retrospective case series (n = 12) | Early MDO | 5–10 y | No alteration in growth pattern. 1 y after MDO, 26.6% relapse in ramus height, 40% relapse in occlusal and bigonial plane canting | Small amount of relapse but, by 1 y, asymmetry stabilized | IV |
| Jansma et al, 2004 | Retrospective case series (n = 2) | Early MDO | 2.5 y | Stable results until end of follow-up | No evidence of relapse following MDO | IV |
| Ortiz Monasterio et al, 1982 | Retrospective case series (n = 6) | Iliac and costochondral grafts | 3.5–5 y | Overcorrection used and, by end of follow-up, slight decrease in overcorrection but no relapse or increase in asymmetry | Proposed overcorrection | IV |
| Trahar et al, 2003 | Prospective case series (n = 6) | Early MDO | 1–2 y | Stable mandibular length without relapse | Proponent of early correction | IV |
| Gui et al, 2011 | Retrospective case series (n = 21) | MDO + graft | 3 y | Greatly improved 3D facial symmetry with minimal relapse. 18 of 21 patients very satisfied with results | IV | |
| Scolozzi et al, 2006 | Retrospective case series (n = 5) | MDO | 2.2 y | Horizontal improvement in symmetry, stable | IV | |
| Satoh et al, 2002 | Prospective case series (n = 10) | MDO | 1.3–3.3 y | Stable results with 2 of 10 patients showing slight occlusal change | IV | |
| Huang et al, 1999 | Prospective case series (n = 5) | MDO | 1 y | Stable symmetry. More downward movement of chin than forward movement | IV | |
| Munro et al, 1989 | Retrospective case series (n = 22) | Grafting | 1–9 y | 16 of 18 with facial growth, 2 of 18 with overgrowth (and relapse of asymmetry) | IV | |
| Vargervik et al, 1986 | Prospective case series (n = 14) | Grafting | 5.2 y | 11 of 14 stable with minimal relapse/return of asymmetry | IV | |
| Ousterhout et al, 1987 | Prospective case series (n = 14) | Grafting | 5.2 y | 11 of 14 stable with minimal relapse/return of asymmetry | IV | |
| Converse et al, 1973 | Retrospective case series (n = 12) | Grafting | 3–12 y | Residual asymmetry present but stable (no relapse) | IV | |
| Relapse of Asymmetry | ||||||
| Mommaerts et al, 2002 | Meta-analysis (8 studies included) | Early MDO | NA | Results revealed high percentage of overcorrection, repeated osteodistraction procedures and soft tissue complications | Despite initial correction, there is relapse of facial asymmetry. The earlier the correction, the more likely that the procedure will have to be repeated. MDO may have possible adverse effect on growth of affected mandible. MDO does not lead to lateral augmentation of soft tissue | I |
| Nagy et al, 2009 | Meta-analysis (13 studies included) | Early MDO | 3 m to 10 y | 7 studies with stable results at end of follow-up (short-term or nonobjective evaluation), 6 studies with unstable results. Type IIb, type III deformities showed relapse with need for reoperation | No convincing evidence supporting effectiveness of early mandibular osteodistraction | I |
| Pluijmers et al, 2014 | Meta-analysis (19 studies included) | Early MDO, graft + MDO, graft alone, E&R | Most common intervention was bone grafting (CCG, rib, iliac). Good results in short term but increased asymmetry over time with MDO and graft patients (type II, III mandible). Most stable results in milder deformities | Single-stage correction should be postponed until permanent dentition phase or skeletal maturity. Treatment of severely hypoplastic mandible should include multistage treatment protocol | I | |
| Kusnoto et al, 1999 | Retrospective case series (n = 6) | Early MDO | 1.5 y | Unoperated patients have fairly stable asymmetry over time. Most favorable results found in body rather than ramus of mandible. Slight decrease in mandible length noted (∼5%) | Mild relapse noted. Recommend 3D evaluation for improved surgical planning | IV |
| Marquez et al, 2000 | Case report (n = 1) | Early MDO | 2 y | Relapse of 87% of vertical distraction length, AP gain was stable. Soft tissue matrix decreased with MDO | Distraction osteogenesis does not accelerate growth and does not predictably increase length of mandible | IV |
| Meazinni et al, 2012, 2008, 2005 | Prospective case series (n = 14, 17, 8) | Early MDO | 11 y, 5 y, 5.8 y | Excellent postoperative results but symmetry obtained was lost at completion of growth (nearly 100% loss of vertical correction) | MDO is not stable over time | IV |
| Batra et al, 2006 | Retrospective case series (n = 3) | Early MDO | 7 y | 30%–60% relapse in ramus height | IV | |
| Gursoy et al, 2008 | Retrospective case series (n = 2) | Early MDO | 5 y | No relapse in vertical or horizontal mandibular length. Relapse of mandibular/skeletal profile and form to predistraction state | IV | |
| Polley et al, 1997 | Retrospective case series (n = 26) | Unoperated patients | 13 y | No significant change in asymmetry over the 13 y of growth. This finding was not influenced by grade and side of mandibular deformity | Skeletal mandibular asymmetry in HFM is not progressive in nature. Growth on affected side parallels that of the nonaffected side | IV |
| Rachmiel et al, 1995 | Retrospective case series (n = 11) | MDO | 1 y | Some relapse in vertical mandibular height noted based on PA cephalograms | IV | |
| Huisinga-Fischer et al, 2003 | Prospective case series (n = 8) | Early MDO | 1–3 y | After 1 y, relapse in 50% of patients. Relapse is progressive 3 y after MDO and all patients showed relapse | IV | |
| Ko et al, 2004 | Retrospective case series (n = 10) | Early MDO | 13 mo | 30% relapse in ramus height, 16% relapse in chin position. Occlusal plane stable | IV | |
| Wan et al, 2011 | Retrospective case series (n = 47) | MDO, graft alone, graft + MDO | 13 y | MDO patients with minimal relapse, 4 of 27 with increased asymmetry), 9 of 27 graft patients with increased asymmetry (and 2 of 27 with overgrowth), 3 of 16 graft + MDO patients with bone resorption and relapse | Relapse seen more frequently with graft-only patients, most stable results in graft + MDO patients | IV |
| Santamaria et al, 2008 | Retrospective case series (n = 8) | Graft alone (fibular free flap), graft + MDO | 3.8 y | 6 of 8 graft patients with partial improvement in occlusion, 2 of 8 with total improvement; 3 of 8 patients with increased asymmetry long term; 2 of 2 graft + MDO patients with partial improvement, no mention of relapse | IV | |
| Chow et al, 2008 | Retrospective case series (n = 4) | MDO | 7 y | Outgrowth of normal side after 2 y. Relapse of asymmetry noted | IV | |
| Cerajewska et al, 2002 | Prospective case series (n = 14) | Grafting | 4 y | Bilateral growth of ramus, minimal relapse of mandibular body length | IV | |
| Hay et al, 2000, 2000 | Prospective case series (n = 15) | Grafting | 3.5 y | Bilateral growth of ramus, minimal relapse of mandibular body length | IV | |
| Singh et al, 1999 | Prospective case series (n = 14) | Grafting | 3 y | Bilateral growth of ramus, minimal relapse of mandibular body length | IV | |
| Padwa et al, 1998 | Retrospective case series (n = 33) | Grafting | 5 y | 42% successful (<5° occlusal cant), 42% acceptable (5°–8°), 16% unsuccessful (>8°); 50% of grafted mandibles outgrown by normal side | IV | |
| Mulliken et al, 1989 | Retrospective case series (n = 8) | Grafting | 4.5 y | 42% successful (<5° occlusal cant), 42% acceptable (5°–8°), 16% unsuccessful (>8°); 50% of grafted mandibles outgrown by normal side | IV | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







