Cosmetic Leukodermas: Therapeutic Approaches
Pearl E. Grimes
Persistent leukoderms or hypopigmentation caused by a variety of aesthetic procedures are indeed dreaded complications. Hypopigmentation can occur after ablative or nonablative resurfacing procedures, chemical peels, dermabrasion, and laser hair removal. In addition, hypopigmented and/or depigmented splayed facelift scars are particularly distressing for many patients. Of these conditions, pigmentary alterations are most often associated with laser resurfacing procedures. Such complications have been reported in all skin types. However, it is most distressing in darker racial ethnic groups. Hyperpigmentation and hypopigmentation are relatively common side effects of ablative laser resurfacing.1,2,3,4,5 The frequency of hyperpigmentation varies from 2% to 37%. It is primarily observed in darker skin types and in some instances is amendable to topical bleaching agents. In contrast, hypopigmentation is more often a late sequela, usually occurring after 6 or 7 months. Published studies report frequencies ranging from 1% to 20%. 1,2,3,4,5 Many physicians have considered cosmetic leukoderma a permanent sequela of resurfacing procedures; however, in my experience, these conditions are amenable to therapeutic intervention.
Pathogenesis of Hypopigmentation
The precise mechanism of pigment loss is unknown. It has been reported that after every resurfacing procedure, there is some loss of melanocytes.6 Hypopigmentation is a common occurrence after phenol peeling, which causes a deep dermal wound. In addition to the induction of dermal fibrosis, phenol and thymol are toxic to melanocytes7,8. Liew et al.9 described the histologic changes of hypopigmentation in nine patients treated for hair removal using the ruby laser. S-100 positive melanocytes remained constant, whereas DOPA oxidase activity appeared to decrease. These findings suggested that the ruby laser caused hypopigmentation by blocking melanin synthesis rather than destroying melanocytes. Laws et al.10 assessed the histologic features of hypopigmentation after CO2 resurfacing in a 62-year-old woman. There was no decrease in the number of melanocytes compared with a pretreatment biopsy. However, there was a decrease in the content of epidermal melanin as assessed with Fontana-Masson staining.
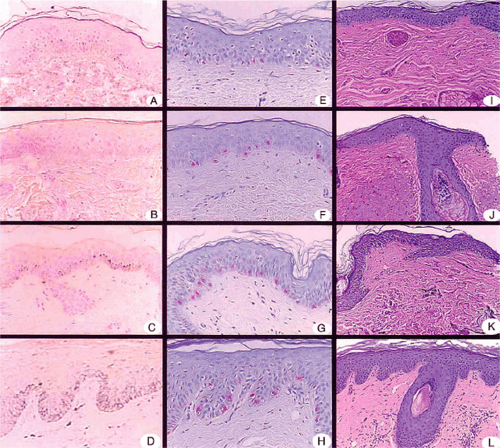
Grimes et al.11 assessed the histopathological features of hypopigmentation caused by laser resurfacing. Biopsies were taken from the affected areas of pigment loss and normal skin for comparison in four patients. All biopsy specimens demonstrated varying quantities of epidermal melanin as well as residual epidermal melanocytes. Mild perivascular inflammation was evident in two specimens (Fig. 14-1). There was superficial dermal fibrosis in all specimens. These findings suggested that laser resurfacing pigment loss was due to a suppression of melanogenesis rather than loss of melanocytes. In addition, dermal fibrosis is also a contributing factor.
Therapeutic Approaches
Albeit challenging, there are several therapeutic regimens that have proven beneficial for patients with hypopigmentation caused by aesthetic procedures.
Topical photochemotherapy
The use of psoralens as repigmenting agents for vitiligo was described as early as 1400 B.C.E.12 In the Indian sacred book Atharva Veda, there is discussion of a plant that produced even skin color. Psoralens are furocoumarin compounds: Photodynamically active drugs that are capable of absorbing radiant energy. They are also found in limes, lemons, celery, figs, and parsnips.12
Psoralens were introduced into the field of modern dermatology by El Mofty in 1947. El Mofty observed repigmentation of vitiliginous lesions after the use of powdered seeds prescribed by native herbalists in Egypt. Early clinical studies in Egypt further documented the effectiveness of the Ammi majus plant extract 8-methoxypsoralen (8-MOP) taken orally or applied topically in combination with
sunlight or ultraviolet (UV) lamps. The acronym PUVA (psoralens + UVA) was introduced in 1974 to describe the use of oral psoralen (8-MOP) with the newly invented high-intensity long-wave (320–400 nm) ultraviolet phototherapy units. More than 30 skin conditions, including vitiligo, have been successfully treated with PUVA therapy.12
sunlight or ultraviolet (UV) lamps. The acronym PUVA (psoralens + UVA) was introduced in 1974 to describe the use of oral psoralen (8-MOP) with the newly invented high-intensity long-wave (320–400 nm) ultraviolet phototherapy units. More than 30 skin conditions, including vitiligo, have been successfully treated with PUVA therapy.12
Although initially used for treatment for vitiligo, topical photochemotherapy has proven efficacious for treatment of cosmetic leukodermas. Grimes et al.11 reported the efficacy of topical photochemotherapy treatments for treatment of laser resurfacing induced hypopigmentation. Seven patients were treated twice a week using 0.001% and 0.01% methoxsalen followed by exposure to artifical UVA light sources. The treatment induced moderate to excellent repigmentation in 71% of the treated patients. Side effects were minimal.
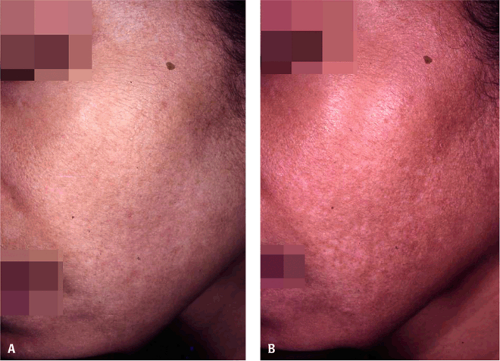 Figure 14-2 Hypopigmentation from a medium depth TCA peel. A: Baseline. B: After twice-weekly topical photochemotherapy treatments (methoxsalen 0.01%). |
The author’s standard protocol uses methoxsalen lotion 1% (Oxsoralen, Valiant Pharmaceuticals, Costa Mesa, CA). Methoxsalen stimulates melanocyte proliferation and melanogenesis. The lotion is diluted to a concentration of 0.001% and 0.01% in Aquaphor. A thin coat of 0.001% concentration is applied to hypopigmented areas 30 minutes before UVA exposure. Patients are treated with an initial UVA fluence of 0.20 J/cm2. The fluence is then increased by 0.20 to 0.50 J per treatment, according to skin type and sensitivity. Lower initial doses and increments are indicated for skin types I and II. After mild to moderate asymptomatic erythema achieved, UVA fluence is maintained at a level sufficient to retain erythema. Treated areas are then cleansed with Cetaphil and water. A broad-spectrum sunscreen is applied after treatment. Patients are treated twice weekly. After 8 to 10 treatments, the concentration of methoxsalen can be increased to 0.01% if therapeutically indicated. High-intensity UVA light sources, such as the Daavlin Spectra 311/350, are used. However, smaller high-intensity UVA units can be used for small areas. Unaffected areas are protected with sunscreen or clothing (Fig. 14-2A,B and Fig. 14-3A,B).
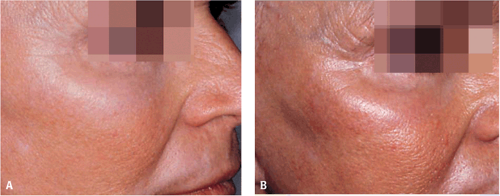 Figure 14-3 Hypopigmentation from CO2 laser resurfacing in skin type II. Before (A) and after (B) 28 topical photochemotherapy treatments. |
For some patients who find it difficult to travel to an office for twice-weekly treatments, topical photochemotherapy with daily sunlight exposure is a viable alternative regimen. A thin coat of 0.001% methoxsalen is applied to hypopigmented areas. After an interval of 20 to 30 minutes, the affected areas are exposed to sunlight for 10 to 20 minutes. For lighter skin types (I–II), initial exposure to sunlight is for 5 to 10 minutes. After 2 weeks, exposure time can be increased to 30 minutes if mild erythema has not occurred. Following sun exposure, the treated sites are washed with soap and water. A broad-spectrum sunscreen is applied after treatment.
The author has treated many patients with this regimen. It is efficacious with minimal complications.
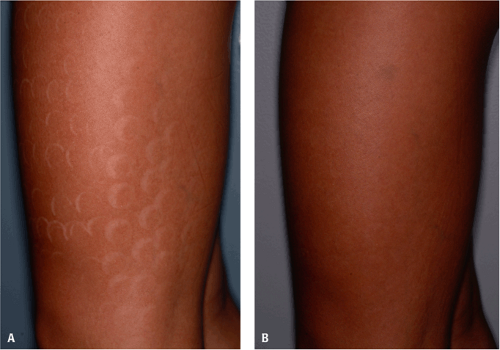 Figure 14-4 Severe hypopigmentation from laser hair removal. Before (A) and after (B)
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|