Chapter 54 Correction of burn alopecia
![]() IN THIS CHAPTER
IN THIS CHAPTER ![]() PowerPoint Presentation Online
PowerPoint Presentation Online
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
Introduction
Patients who sustain large total body surface area burns have involvement of the head and neck between 25% and 45% of the time.1,2 Since human skin does not regenerate itself, scarring is the end result of the healing process. Such scarring can not only be disfiguring but also can lead to contractures which can affect function. The ultimate effect of deep burns to the scalp is loss of hair leading to cicatricial alopecia. The management of this problem is multifactorial. It includes the analysis of the size of the defect, its location, the surface area of the remaining scalp and the condition of the remaining hair-bearing scalp. The treatment can range from excision with primary closure to the use of multiple tissue expanders.
The scalp is a popular donor site for the harvesting of split thickness skin grafts to resurface patients with large total body surface area burns. Multiple harvestings of skin grafts from the scalp may also lead to cicatricial alopecia. However, the incidence of alopecia associated with graft harvesting remains controversial. In 1990, Brou et al.3 reported a 61% incidence of alopecia in patients with existing scalp burns, in which skin grafts were harvested from the injured scalp. Yet, only a 2.2% incidence of alopecia was noted in patients without burns to the scalp who underwent harvesting of scalp grafts for closure of burn wounds.4 Reconstructive surgeons have a number of tools available to address the correction of problems associated with burn patients. However, one must keep in mind that inherent in all techniques can be problems associated with color match, texture, and donor site disfigurement. Certainly, primary closure of burn alopecia can eliminate these problems using local flap advancement. Now, tissue expansion is an example of how skin responds to mechanical stress. It offers a number of advantages when compared with other modalities of reconstruction. Such advantages as color match, sensation and minimal donor site morbidity are not to be taken lightly. However, tissue expansion is not for everyone. But, it is such a valuable technique that it has become an integral part of the armamentarium for reconstruction surgeons who are charged with the reconstruction of burn patients.
Histomorphology of tissue expansion
It is noted that tissue expansion occurs under natural conditions (i.e. pregnancy, breast development) and in abnormal circumstances (expansion of the neck, earlobes). As part of the aesthetics in various societies, tissue expansion has been noted to document positions of social hierarchy.5,6 The first clinical case of soft tissue expansion was reported by Neumann in 1957.7 In a case of partial traumatic ear loss in a 52-year-old man, Neumann inserted a rubber balloon above the ear to create an expanded flap to cover his cartilaginous framework. However, in spite of this remarkable case, the idea of soft tissue expansion to correct traumatic defects remained dormant for another 20 years. In 1975, both Austad et al. and Radovan began pioneering work on soft tissue expansion.8–10 Experimental data on the histomorphology of tissue expansion largely came from animal data. Although Austad reported the laboratory experience with tissue expansion prior to clinical use, Radovan is noted as the first surgeon to claim extensive use with tissue expanders clinically.
Epidermis
The response of the epidermis to tissue expansion is quite interesting. The examples of tissue from both guinea pigs and humans reveal epidermal thickening.8–11 Additional studies by Pasyk et al. noted that epidermal thickening can last up to two years after expansion. Pasyk also showed that the epidermal thickening occurred in the stratum spongiosum.11 However, there is no correlation between epidermal thickening with expansion time, location, volume or patient age. Interestingly, with expansion, light microscopy reveals an undulated basal lamina. The basal and prickle cells show an increase in the bundles of tonofibrils within the tonofilaments. Such findings along with a decrease in the intracellular spaces, in all of the epidermal layers, suggest increased mitosis. These findings were later supported by Austad, who documented increased mitotic activity using tritiated thymidine. The three-fold increase in epidermal mitosis occurred during expansion but returned to baseline in 2–5 days.9
Dermis
The expansile and recoil properties of the skin are related to the amount of collagen and elastin fibers in the dermis.12,13 Similarly, the epidermis, like the dermis, undergoes significant changes during the expansion process. However, the thickness of the dermis is reduced dramatically. This is not related to expander volume or anatomic location.10 Most of the dermal thinning occurs in the reticular dermis, with thinning of the papillary dermis being less dramatic. During the first few weeks of expansion, the dermis thins significantly but less so towards the end of the expansion process. After expansion, the reticular dermis is noted to have increased amounts of thick bundles of collagen fibers parallel to the skin. In addition, the elastic fibers in the expanded dermis were thicker and longer. It is believed that the presence of increased numbers of active fibroblasts in the dermis is responsible for the immature collagen fibers. Collagen bundles populate both the reticular and papillary dermis from the multiplication of fibroblasts.12,13
Skin has the ability to stretch and recoil. Elastin fibers are linked to each other by end-to-side junctions, and interspersed among collagen fibers, which are often larger and unlinked to another. Elastin fibers, unlike collagen, have the ability to stretch and retract. Collagen fibers in their relaxed state are disoriented and unparalleled. These fibers, in the presence of applied stress, align in a parallel fashion.10 This response is believed to be linearly proportional to the magnitude of the applied stress. However, too much stress during expansion of skin can cause constriction in the tiny blood vessels, inducing ischemia. The goal of reconstructive surgeons is to take advantage of this regenerative process without causing flap loss secondary to ischemia. It should be noted that sebaceous glands and sweat glands, and sensory nerves might undergo subtle changes. Hair follicles remain unchanged qualitatively but remain active. The lumens of various glands remain open even though adjacent structures have been compressed.12,13 It is believed that sensory fibers do not under go any appreciable structural changes.10
Blood vessels
Several investigators have noted a significant proliferation of blood vessels associated with tissue expansion. This proliferation occurs primarily at the junction of the capsule and host tissues. Within days of expansion, small capillaries become distended, and in addition, the number of arterioles and venules increase. Cherry et al. noted an increase in the surviving length of expanded random-patterned skin flaps when compared with delayed skin flaps.14 Sasaki and Pang confirmed previous studies by documenting increased blood flow in expanded flaps.15 Lantieri et al. later suggested that vascular endothelial growth factor (VEGF) may play a part in the development of the increased vascularity of expanded flaps as VEGF was only expressed in expanded flap.16
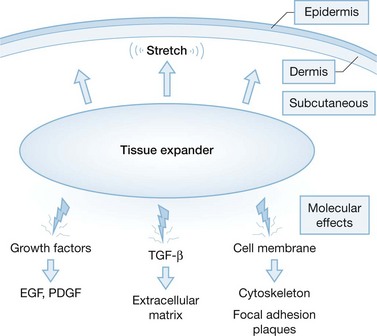
Molecular basis of tissue expansion
Clearly, several studies have documented an increased mitotic index in the epidermis with tissue expansion.9,17 Yet, Takei et al. thought the mechanism of action was through the activation of growth factors.18 This group postulated that platelet derived growth factors and other growth factors could stimulate cutaneous cellular activity. It is well known that transforming growth factor-B (TGFβ) can not only influence extracellular matrix production but can also enhance fibroblast proliferation. In addition, it is felt that membrane bound molecules can play a role in the regulation of signal transduction pathways (Fig. 54.1). Although it is clear that strain has an effect on skin biology, whether or not we can modulate its effects chemically may be a rich source for future research.
Clinical application: correction of burn alopecia
Primary closure
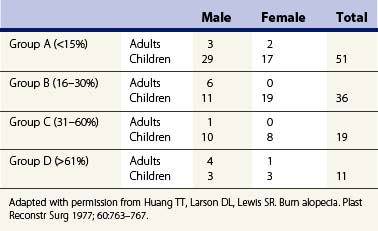
In 1978, Huang et al. categorized the extent of burn alopecia as it related to correction of this problem. At this time, the authors used primary excision and rotation flaps as a means to either eliminate or camouflage burn alopecia.19 This group discovered that alopecia greater than 15% of the hair-bearing scalp was not amenable to correction using serial excision. The next stage in the evolution of closure of scalp defects came from Orticochea. The use of three and four limb Orticochea flaps was successful in the closure of scalp defects greater than 15%.20 The Juri flap, a pedicled, laterally-based scalp flap, was described to re-establish the anterior hairline in bald patients. The use of the Juri flap along with tissue expansion has also been described.21,22 It is clear that the use of primary closure in the correction of burn alopecia without the use of tissue expansion is possible. However, the extent of closure is less than 20–25% (Table 54.1). In general, if more than two operations are required to close a scalp defect, tissue expansion should be given serious consideration.