I. OVERVIEW OF CONGENITAL UPPER EXTREMITY ANOMALIES
A. Incidence
1. Approximately 0.2% of all live births
2. Most common: Syndactyly, polydactyly, and camptodactyly
3. 95% sporadic
4. Frequently associated with cardiac, hematopoietic, and tumorous conditions due to simultaneous development.
B. Embryologic development
1. The arm bud (consisting of mesenchyme and covered by ectoderm): Appears at 30 days of gestation and *is complete by 8 weeks (ossification continues throughout gestation).
2. Development: Hox genes (A, B, C, and D) and directed by signaling proteins including sonic hedgehog, fibroblast growth factor, and Wnt-7a.
3. Development occurs in three planes: Proximal to distal axis, dorsal to palmar axis, and anteroposterior (preaxial/postaxial) axis.
a. *Apical ectodermal ridge: Thickening of ectoderm at the leading edge of the limb bud; controls proximal to distal differentiation.
b. Dorsal ectoderm: Differentiation along dorsal to palmar plane (flexor and extensor regions).
c. *Zone of polarizing activity: Anterior–posterior (radial/ulnar) differentiation and is a group of mesenchymal cells on the preaxial (radial) aspect of the upper limb. Caused by Hedgehog signaling.
4. Fourth week: Limb buds appear
5. Fifth week: Apical ectodermal ridge appears, hand plates develop
6. Sixth week: Digital separation by apoptosis
7. Seventh week: Mesenchymal differentiation and chondrogenesis
8. Eighth week and beyond: Ossification of the skeleton
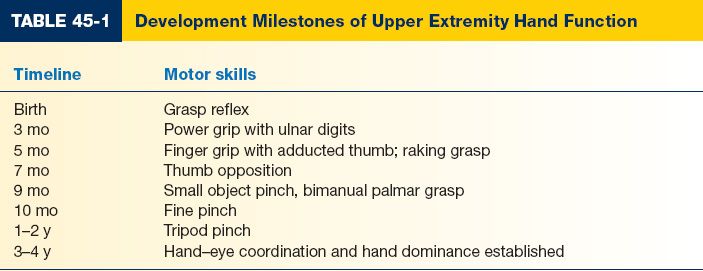
C. Developmental milestones: Ideally, reconstruction should be performed by age 4 prior to school entry for socialization and to match developmental milestones (Table 45-1)
1. At birth: Grasp reflex present
2. 3 months: Power grip with ulnar digits
3. 5 months: Finger grip with adducted thumb
4. 7 months: Thumb opposition with power grip
5. 9 months: Small object pinch
6. 10 months: Fine pinch
7. 3 to 4 years: Hand preference established
8. Ossification centers: See tips of distal phalanx by 7 weeks of gestation, metacarpals and proximal phalanx by 9 to 10 weeks; middle phalanx by 10 to 12 weeks. Wrist: First form capitate (0 to 6 months postnatal), then hamate (0 to 6 months).
______________
*Denotes common in-service examination topics
II. CLASSIFICATION
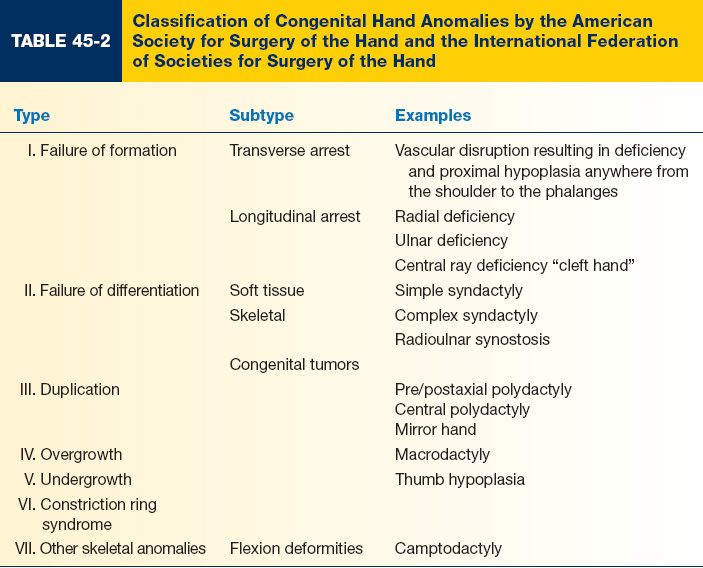
A. International Federation of Societies for Surgery of the Hand (IFSSH) classifies congenital hand anomalies into seven distinct groups (Table 45-2)
III. WRIST AND FOREARM ABNORMALITIES
A. Radial deficiency
1. General concepts
a. Most common type of longitudinal failure of formation
b. Involve radial side of the forearm, including the radius, radial carpus, and thumb.
c. Hypoplasia of some or all elements, including thumb hypoplasia, absence of the scaphoid and trapezium, camptodactyly of the radial digits, and absence of radial artery and nerve.
d. Radiographs of the hand and wrist are needed to determine the extent of malformation.
2. Epidemiology
a. 1/30,000 to 1/100,000 live births
b. More common among male infants and Caucasians
c. 50% are bilateral; unilateral: Right more affected than left
3. Associated syndromes
a. Genetic syndromes: Children should be evaluated by a geneticist and undergo a thorough workup, including spinal radiographs, echocardiogram, and a renal ultrasound.
b. *Fanconi’s anemia: Radial deficiency with polydactyly, syndactyly, clinodactyly, atrial septal defect (ASD), and pancytopenia (Autosomal recessive)
c. TAR syndrome: Thrombocytopenia, absent radius
d. Holt–Oltram syndrome: ASD with radial deficiency (Autosomal dominant)
e. VATER association (vertebral anomalies, anal atresia, tracheoesophageal fistula, renal defects)
f. Chromosomal anomalies (trisomies 13 and 18)
g. Nager syndrome: Radial deficiency/acrofacial dysostosis (Autosomal dominant)
h. Mobius syndrome: Congenital facial paralysis, limb abnormalities in 25% of cases.
i. Klippel–Feil syndrome
4. Presentation
a. Fibrotic muscle bellies result in bowing of the ulna
b. Shortened ulna and hypoplastic distal humerus result in elbow stiffness
c. Hand assumes flexed and radially deviated position
d. Extensor indicis proprius (EIP) may be deficient, flexors abnormal, thumb muscles affected.
e. Nerve: Radial nerve ends after triceps; median nerve innervates radial forearm skin
f. Vessels: Ulnar artery may be only vessel; interosseous artery may replace radial artery
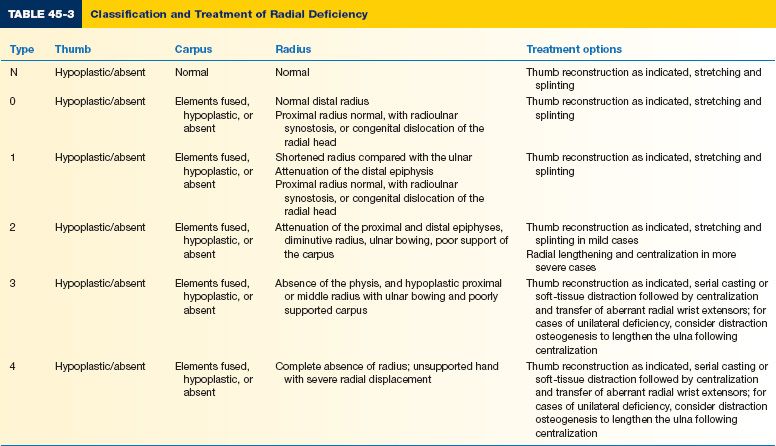
5. Treatment (Table 45-3)
a. Stretching
b. Serial casting
c. External soft tissue distraction
d. Centralization of the wrist on the ulna
i. Radially placed Z-plasty incision to release skin tightness
ii. Median nerve is usually present and can be easily injured during surgical exposure due to aberrant anatomy.
iii. Carpus released from the radial-sided wrist flexors and extensors (brachioradialis [BR], flexor carpi radialis [FCR], extensor carpi radialis longus [ECRL])
iv. Carpus is centralized on the ulna, and a Steinmann pin is used to fix the middle metacarpal, carpus and ulna
v. Tendon transfers are used to maintain a centralized wrist position: Fused mass of FCR, ECRL, extensor carpi radialis longus brevis and BR is transferred to extensor carpi ulnaris to become ulnar deviator, thus balancing the wrist.
vi. Corrective osteotomy of the ulna may also be performed
vii. Soft-tissue coverage achieved via local tissue rearrangement (e.g., bilobe flap)
6. Contraindications to reconstruction
a. Older patients who have adapted to the deformity, or in patients with poor elbow flexion
b. In these cases, radial deviation and flexion of the hand assist with activities of daily living among patients with severe elbow stiffness.
7. Long-term outcomes
a. Recurrent radial deviation, wrist stiffness
b. Centralization improves appearance, but the extent to which improves long-term function is not known.
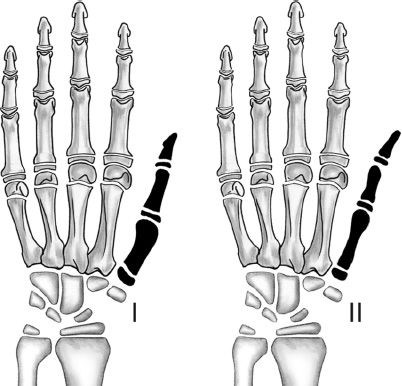
B. Ulnar deficiency
1. Epidemiology
a. Less common than radial deficiency
b. Approximately 1/100,000 births
c. Usually sporadic and unilateral, and rarely associated with other syndromes
d. About 50% of patients have another musculoskeletal anomaly (e.g., proximal femoral focal deficiency, fibular deficiency, phocomelia, and scoliosis); 90% have associated hand anomalies (e.g., syndactyly, absent digits, and thumb abnormalities).
e. Malformations range from hypoplasia to total absence with radiohumeral synostosis.
2. Anatomy
a. The ulna is absent, and a fibrocartilaginous “anlage” is present that inserts on the ulnar aspect of the carpus and distal radius rather than the ulna, and fails to grow commensurately with the child.
b. Flexor carpi ulnaris typically absent
c. Median and ulnar nerves present, but ulnar artery usually absent
d. Unlike radial deficiency, the carpus is stable; however, the elbow may be unstable due to radial head dislocation.
3. Treatment
a. Depending on the associated hand anomalies, may require syndactyly release, first web space deepening, opponensplasty, pollicization, and thumb metacarpal rotational osteotomy.
b. Serial casting and splinting to improve elbow posture
c. Excision of fibrous anlage when there is 30 degrees or more of angulation or progressive ulnar angulation. May be combined with radial osteotomy to further straighten the forearm axis.
d. Loss of elbow function may be improved with resection of the radial head and osteosynthesis of the distal radius to the proximal ulna
e. Derotational osteotomy of the humerus for children with severe internal rotation and radiohumeral synostosis.
4. Outcomes: Following treatment, long-term function is improved, but less pronounced in patients with radiohumeral synostosis and absent or stiff digits.
C. Madelung deformity
1. Definition: Excessive radial and palmar angulation of the distal radius due to a growth disturbance at the ulnar aspect of the physis.
2. Pathophysiology: Growth disturbance at the physis may be due to a bony lesion or due to abnormal ligamentous tethering of the lunate to the distal radius.
3. Epidemiology
a. More common in females
b. Usually bilateral
a. Patients typically present at school age, from 6 to 13 years
b. Deformity includes dorsal prominence of the ulna and ulnar positive variance
c. Concave, foreshortened appearance of the forearm
d. The degree of functional impairment varies. Patients asymptomatic, or complain of pain with ulnar deviation and wrist extension.
5. Treatment
a. No treatment indicated for painless deformity
b. Symptomatic deformity: Physiolysis, release of palmar–ulnar ligaments, and corrective osteotomy
D. Transverse failure of formation (congenital amputation)
1. Epidemiology
a. Usually unilateral, and most commonly at the proximal forearm
b. Sporadic
2. Pathophysiology
a. Etiology unknown, but likely due to intrauterine vascular compromise at the apical ectodermal ridge or developing limb bud.
3. Presentation
a. Most commonly presents with arrest at the proximal forearm
b. Elbow flexion and extension intact, but difficulty with pronation and supination
4. Treatment
a. Surgical intervention is rarely indicated. Children function well with active and passive prosthetic options.
E. Radioulnar synostosis
1. Definition: Failure of separation of the proximal radius and ulna
2. Epidemiology
a. 60% bilateral
b. Majority sporadic, but autosomal dominant inheritance has been described
c. May be associated with other upper extremities in 30% of affected children (e.g., thumb hypoplasia) and associated with Apert syndrome and arthrogryposis.
3. Presentation
a. Children present with lack of forearm rotation and presence of elbow flexion contractures, resulting in difficulty with hand positioning and dexterity.
b. Radial head subluxation or dislocation may also be present
c. Children may compensate through rotation at the shoulder, radiocarpal, intercarpal, and carpometacarpophalangeal (CMC) joints.
4. Treatment
a. Indications
i. Functional impairment due to lack of supination and pronation
ii. Forearm is fixed in more than 60 degrees of pronation.
iii. Bilateral deformity
b. Options
i. Derotational osteotomy at synostosis or at the diaphysis with placement of forearm in neutral or slight pronation.
ii. Resection of synostosis and interposition of autologous tissue (vascularized or nonvascularized grafts) or allograft between the radius and ulna.
c. Outcomes
i. Complications: Chronic wrist and elbow pain, compartment syndrome, and neurovascular injury.
ii. Recurrent deformity is common
F. Congenital dislocation of the radial head
1. Epidemiology
a. Most common congenital elbow deformity
b. Usually bilateral
c. Associated with congenital radioulnar synostosis
2. Presentation
a. Radial head may be dislocated anteriorly, posteriorly, or laterally, and patients present with a lack of forearm rotation.
b. Diagnosis may be confused with traumatic dislocation
c. Majority of patients are asymptomatic with minimal functional limitations
3. Treatment
a. Observation
b. Open reduction and reconstruction of the annular ligament can be considered in symptomatic patients, but often unreliable and unpredictable results.
c. Radial head excision can be considered for symptomatic patients with degenerative changes.
G. Congenital pseudoarthrosis of the ulna
1. Definition: Replacement of the distal or middle third of the ulna with fibrous tissue
2. Epidemiology: Associated with neurofibromatosis
3. Presentation
a. Forearm is foreshortened with radial bowing and radial head dislocation
b. Patients present with forearm deformity, weakness, pain, instability, and lack of motion.
4. Treatment
a. Resection of pseudoarthrosis and free vascularized fibula transfer
H. Arthrogryposis
1. Definition
a. Multiple nonprogressive joint contractures due to a lack of fetal development
b. Etiology is variable and can be related to genetic syndromes (e.g., Beals syndrome and Freeman–Sheldon syndrome) or sporadic.
2. Presentation
a. *Most commonly present with bilateral, symmetric contractures of the upper extremity, including shoulder adduction and internal rotation, elbow extension, forearm pronation, wrist flexion and ulnar deviation, and finger flexion.
b. Muscle atrophy is often present
3. Treatment
a. Nonoperative
i. Passive range of motion; stretching beginning in infancy
ii. Static progressive splinting or serial casting if needed
b. Operative
i. Shoulder: Corrective osteotomy of the humerus
ii. Elbow: Posterior capsulotomy and triceps lengthening to achieve passive elbow flexion
iii. Wrist: Proximal row carpectomy, soft-tissue distraction, and corrective osteotomy
IV. HAND DEFORMITIES
A. Syndactyly
1. Definition: Fusion of soft tissue and sometimes bony elements of the digits
2. Epidemiology
a. *Occurs in approximately 1 in 2,000 to 3,000 births
b. 50% bilateral
c. 10% to 40% present with a family history of syndactyly suggesting autosomal dominance with variable penetrance
d. Observed in patients with Poland’s syndrome, Apert syndrome
a. *Most common between the middle and ring finger, followed by the ring and small finger
b. Simple: Skin fusion only
c. Complex: Bony fusion and skin fusion. Most commonly involves the distal phalanx. Can be identified with preoperative radiographs.
d. Complete: Fusion along the entire length of the digit
e. Incomplete: Fusion along the portion of the digit not including the nail folds
f. Complicated: Fusion of multiple digits (e.g., Apert syndrome)
4. Treatment
a. Release is indicated to enhance aesthetic appearance, limit functional limitations, and prevent growth restriction and deformity.
b. Release is usually performed between age 12 and 18 months unless growth restriction and angular deformity is evident earlier.
c. Contiguous web spaces are released in a staged fashion in order to avoid vascular compromise.
d. Surgical options
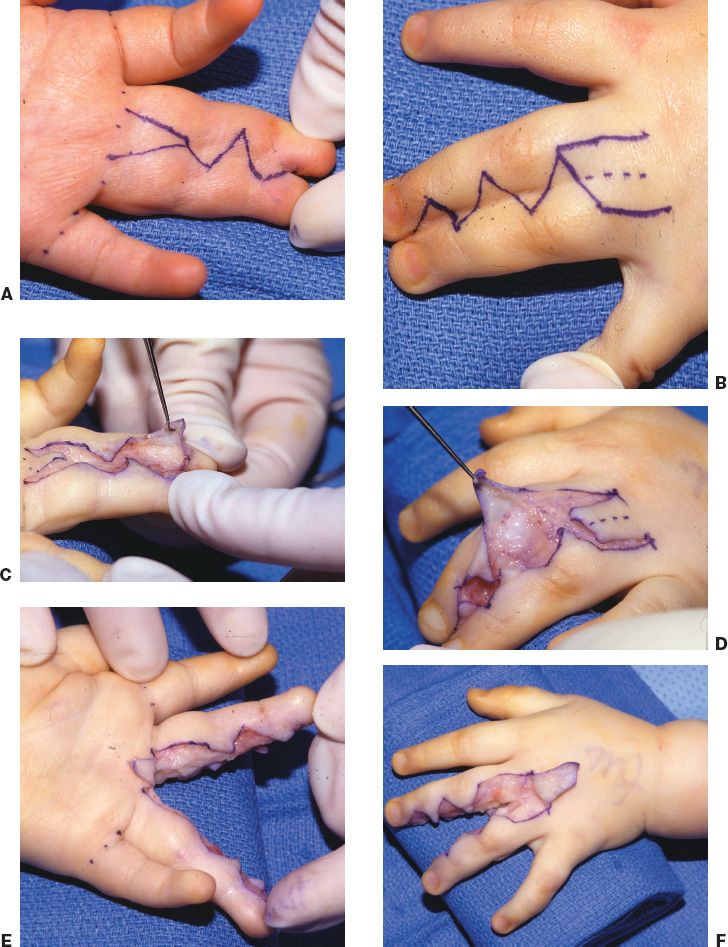
i. A proximally based, dorsal rectangular skin flap is designed between the two metacarpal heads to incorporate the perforating metacarpal artery vessel is advanced into the web space. Interdigitating triangular flaps are designed to resurface the digits, and a full-thickness skin graft is often harvested from the groin to complete coverage (one variation shown in Fig. 45-1).
e. Postoperative complications
i. Skin flap loss and delayed wound healing, scar contracture, web space creeping (most common), joint instability, skeletal deformity, keloid formation.
B. Ulnar polydactyly
1. Definition: Accessory digit is present on the postaxial aspect of the hand
2. Epidemiology
a. *Most common presentation of polydactyly
b. Autosomal dominant with variable penetrance
c. More common in African Americans (1 in 143 births) compared with Caucasians (1 in 1,400 births)
3. Presentation: May be well developed (type A), or rudimentary and pedunculated (type B)
4. Treatment
a. Operative ablation or excision is preferred rather than bedside ligation in order to minimize long-term deformity.
b. Well-developed accessory digits may require transfer of the ulnar collateral ligament and abductor digiti minimi, and identification and ablation of the accessory neurovascular bundle.
C. Central polydactyly
1. Definition: Duplication of digits within the central aspect of the hand
2. Presentation
a. Ring finger is most commonly duplicated
b. May present in conjunction with syndactyly and can be discerned on radiographs
3. Treatment
a. Functional accessory digit without syndactyly may not require surgical intervention.
b. Accessory digit with stiffness or functional limitation should undergo ray resection. If present with syndactyly, may require only partial resection with reconstruction in order to maintain function.

Figure 45-1. One method of syndactyly reconstruction. There are countless methods of syndactyly reconstruction. Most rely on a dorsal quadrilateral flap, as illustrated in this example. A: A volar zigzag incision is designed to prevent scar contractures over the joints. If a straight line incision were used, then a contracted scar would develop. Some use a triangular flap at the volar base of the release as shown here. Many do not. B: A dorsal quadrilateral flap is designed to provide full thickness coverage in the web. C and D: The zig-zag flaps are raised in a subcutaneous plane. E and F: The digits are fully separated, including the neurovascular bundles. G: The dorsal flap may be split, as shown in this example, by the volar flap. Many authors don’t use a volar flap and thus inset the dorsal flap without splitting it. The zig-zag flaps are inset. H: Following release of the tourniquet, the fingertips have a pink color, indicating adequate circulation. I and J: Areas not covered by the flaps are resurfaced with full thickness skin grafts. (Strickland JW, Graham TJ. Master Techniques in Orthopaedic Surgery: The Hand. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
1. Definition: Symmetric duplication of the hand at the midline
2. Presentation
a. Central digit with three digits along the radial and ulnar aspect (duplicated middle, ring, and small fingers) and an absent thumb.
b. Ulna is duplicated and radius is absent; ulnar carpal elements are duplicated
c. Hand is radially deviated; wrist extensor tendons may be absent and extension is weak. Limited pronation and supination.
3. Pathophysiology: Duplication of the zone of polarizing activity
4. Treatment: Reduce accessory digits to four digits and pollicization to create a thumb
E. Brachydactyly
1. Definition: Shortened digits with all elements present
2. Presentation
a. Often seen in conjunction with other congenital hand anomalies (syndactyly, clinodactyly, and camptodactyly) and syndromes (e.g., *Poland’s syndrome, Apert syndrome, orofaciodigital syndrome).
b. Can be associated with syndactyly (e.g., Poland’s syndrome due disturbance in development of the subclavian artery).
3. Treatment
a. Considered if significant functional limitation is present
i. Lengthening: Osteotomy and bone grafting
ii. Distraction osteogenesis
iii. Syndactyly release if present
b. Common postoperative complications include digital stiffness and joint contracture
F. Central ray deficiency “cleft hand”
1. Definition: Longitudinal deficiency of central hand elements
2. Epidemiology: Autosomal dominant with variable penetrance and expression
3. Presentation
a. A V-shaped deformity is present with or without absence of digits
b. Typical
i. Failure of development of the middle digit and metacarpal leading to a deep V-shaped cleft.
ii. Border digits may have syndactyly
iii. Autosomal dominant
iv. May involve multiple extremities including feet
c. Atypical
i. Broad and flat, U-shaped cleft with missing or shortened central digits
ii. Vestigial remnants may be present
iii. Sporadic
iv. One extremity involved
v. Thumb and ulnar digits are present
vi. Variation of symbrachydactyly
d. Involvement of the first web space is predictive of hand function
4. Treatment
a. Cleft hands frequently function well, despite aesthetic appearance
b. Progressive deformity may result from syndactyly or the presence of transverse bones within the cleft.
i. Removal of transverse bones
ii. Syndactyly release
iii. First web space release
iv. Cleft closure
c. Snow-Littler procedure: First web space is released and the index metacarpal is transposed to the base of the middle finger metacarpal position.
d. Absence of the thumb
i. Second toe transfer
ii. Pollicization of available digit
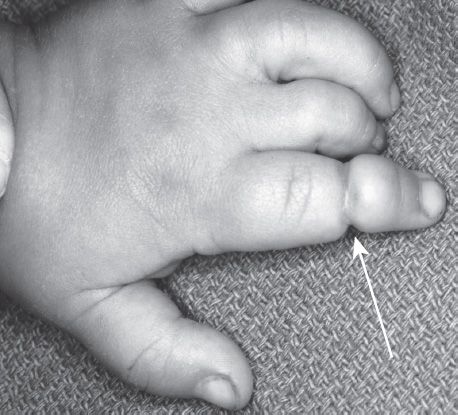
G. Constriction ring syndrome/amniotic band syndrome (Fig. 45-2)
Figure 45-2. Constriction (amnionic) band syndrome. Arrow points to constriction band of the index finger. (From Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
1. Definition: Circumferential constriction of the extremity or digits due to amniotic disruption and band formation
2. Epidemiology
a. 1:1,200 to 1:15,000 births
b. Not
3. Presentation
a. Index, middle, and ring fingers most commonly affected
b. Extremity or digit is hypoplastic or absent distal to the band, and amputation, lymphedema, and acrosyndactyly
4. Treatment
a. Elective release at 1 year of age is indicated to improve function (grip and pinch) and hand appearance; emergent release is indicated for arterial or venous compromise.
b. Constriction ring
i. Z-plasty release of constriction band along the lateral aspect of the digit to minimize scarring.
ii. Advancement of adipofascial flap to recontour irregularities along the aspect of the digit.
c. Acrosyndactyly
i. Digits may be released using syndactyly release techniques to reconstruct the commissure.
H. Thumb duplication
1. Definition: Preaxial polydactyly involving duplication of varying elements of the thumb
2. Epidemiology
a. 1/3,000 live births
b. *Most common in Asian descent (2.2/1,000), Native Americans (0.25/1,000), and African Americans and Caucasians (0.08/1,000)
c. Inheritance: Usually sporadic and does not require genetic counseling with the exception of triphalangeal thumb, which is inherited in an autosomal dominant fashion.
3. Presentation
a. Usually unilateral
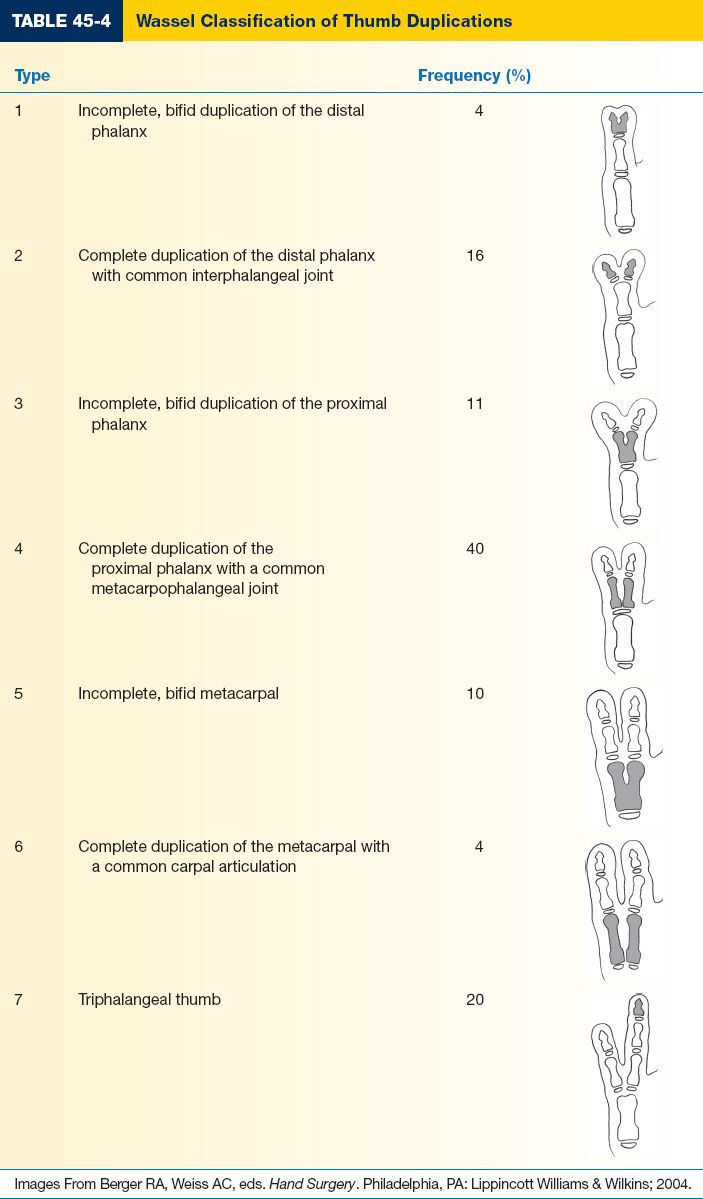
b. Wassel Classification is based on the level of duplication and number of elements (Table 45-4)
4. Treatment
a. Reconstruction usually performed around the ages of 12 to 24 months to correspond with the development of pinch grasp
b. Reconstruction depends on the degree of hypoplasia, joint stability, and thumb alignment.
c. Types 1 and 2
i. Resection of radial duplication
ii. Central resection of bone, soft tissue, and nail and fusion of elements (Bilhaut–Cloquet procedure)
e. Types 3 and 4
i. Ablation of the radial duplicate
ii. *Radial collateral ligament reconstruction
f. Types 5 and 6
i. Ablation of the radial duplicate
ii. *Radial collateral ligament reconstruction
iii. *Intrinsic muscle reattachment
iv. *Corrective osteotomy
g. Type 7
i. Complex, multistage reconstruction
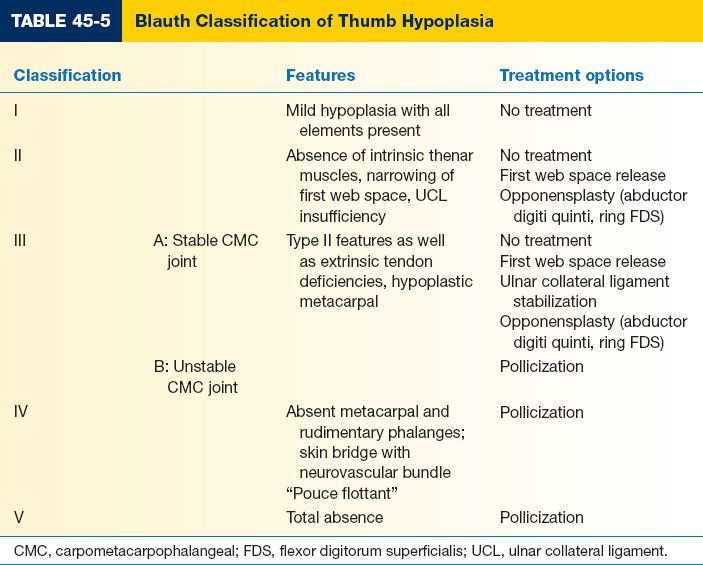
I. Thumb hypoplasia/absence (Fig. 45-3)
1. Definition: Spectrum of thumb abnormalities ranging from mild hypoplasia to complete absence of soft tissue and skeletal elements
2. Epidemiology
a. Often seen in conjunction with radial longitudinal deficiency
b. Associated syndromes include *Holt-Oltram syndrome, Fanconi’s anemia, TAR, and VACTERL
3. Presentation
a. Blauth classification: Five degrees of thumb hypoplasia (Table 45-5)
i. Type 1: Smaller thumb but normal functioning
ii. Type 2 and 3a present with a stable CMC joint
iii. *Types 3b, 4, and 5: CMC joint absent
4. Treatment
a. Consider treatment within 2 years of age as pinch grip and opposition is developing.
b. Type 1: No surgical treatment indicated
c. Type 2 and 3a
1. Deepening first web space with Z-plasty techniques
2. Opponensplasty using abductor digiti minimi (Huber transfer) or flexor digitorum superficialis (FDS) from the ring finger
3. EIP to extensor pollicis longus (EPL) transfer
d. Types 3b, 4, and 5: *Ablation of the remnant thumb if present, and index finger pollicization
1. General pollicization steps
a. Skin is incised as described by Buck-Gramcko or Ezaki taking care to protect the dorsal veins.
b. Pollicization is based on the ulnar digital artery of the index finger, and the radial digital artery to the long finger is ligated.
c. A1 pulley and deep transverse intermetacarpal ligament is divided
d. Juncturae tendinae between the extensor tendons are divided. The first dorsal and palmar interossei are elevated to their origin.
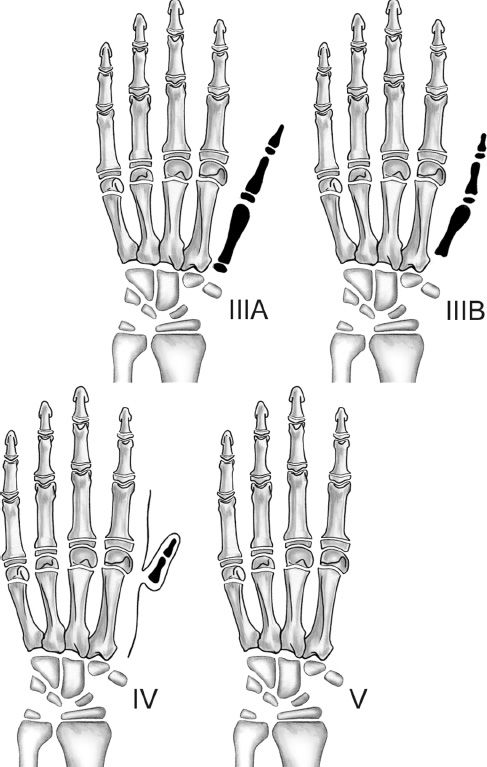
Figure 45-3. Blauth classification of thumb hypoplasia (see Table 45-5). (From Berger RA, Weiss AC, eds. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)
e. Index metacarpal shaft is shortened with a proximal osteotomy at the metacarpal base and a distal osteotomy through the physis distal to the neck of the metacarpal.
f. The index finger is positioned such that the tip is level with the proximal interphalangeal (PIP) joint of the middle finger in 45 degrees of abduction and 100 to 120 degrees of pronation.
g. The first dorsal interosseus tendon is sutured to the radial lateral band, and the first palmar interosseus is attached at the ulnar lateral band to provide abduction and adduction.
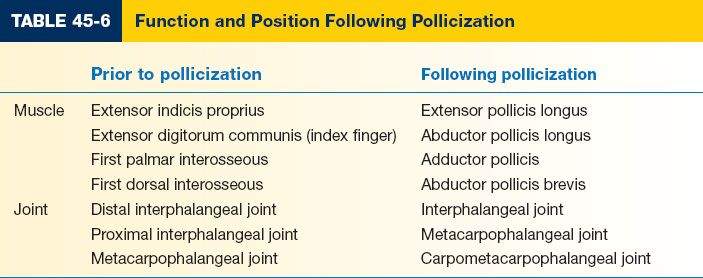
h. Functional elements following pollicization (Table 45-6).
J. Congenital clasped thumb
1. Definition: Lack of passive metacarpophalangeal (MP) joint extension due to soft tissue deficiency, extrinsic tendon hypoplasia or absence, intrinsic muscle contracture, and MP joint contracture.
2. Presentation
a. Type 1: Absence of extensor pollicis brevis (EPB); normal interphalangeal (IP) and CMC motion; treated with splinting and stretching; nonoperative management.
b. Type 2: MP joint flexion contracture with skin deficiency limits MP joint extension and CMC abduction, passive IP joint extension, and active flexion intact.
c. Type 3: Fixed flexion and adduction deformity at the IP, MP, and CMC joints
3. Treatment
a. Intrinsic muscle contracture: Release adductor pollicis, thenar muscles, and palmar fascia.
b. Deficiency of the soft tissue: Z-plasty techniques
c. Extrinsic tendon abnormalities
i. EPL/EPB hypoplasia or absence: Transfer of EIP or FDS to EPL
ii. Flexor pollicis longus (FPL) contracture: Stepwise lengthening of FPL
K. Symphalangism
1. Definition: Failure of IP joint development resulting in fusion of the middle and proximal phalanges
2. Epidemiology
a. 1% of all upper extremity anomalies
b. Inherited in an autosomal dominant
3. Presentation
a. Absence of joint motion at the PIP joint; flexion achieved only through MCP and distal IP joints
b. PIP joint does not develop with upper extremity growth
c. May also present with syndactyly or brachydactyly
4. Treatment
a. Poor results with joint reconstruction
b. Arthrodesis may be performed if poor grasp is present due to deformity
L. Camptodactyly
1. Definition: Congenital flexion contracture at the PIP joint which can be reducible or irreducible
2. Epidemiology: Can be sporadic or inherited in an autosomal dominant fashion with variable penetrance
3. Presentation
a. Majority of patients present with mild or asymptomatic, small finger PIP contractures with minimal functional deficit, usually bilateral.
b. Classification
i. Type 1: Flexion contracture presents in infancy
ii. Type 2: Presents gradually in school age; may progress to severe contractures
iii. Type 3: Bilateral involvement of multiple digits, usually associated with other congenital syndromes
c. FDS is contracted with atrophic or absent muscle belly
d. Anomalous lumbrical origin or insertion
4. Treatment
a. Nonoperative management is indicated for those patients with mild deformity and minimal functional impairment.
b. Operative release of the PIP joint
M. Clinodactyly
1. Definition: Bony deformity resulting in radioulnar angulation of the digit distal to the MP joint greater than 10 degrees.
2. Epidemiology
a. Autosomal dominant with variable penetrance
b. Bilateral
c. Incidence is variable from 1% to 20%
d. More common in males
e. Associated with Down syndrome and Apert syndrome (thumb)
3. Presentation
a. Growth deformity due to insult at the epiphyseal growth plate that restricts growth along one side of the bone: Results in a triangular or “delta” phalanx.
b. Most commonly seen as radial inclination of the small finger due to triangular or trapezoidal shape of the middle phalanx.
c. Deviation may interfere with pinch and grip
4. Treatment
a. Surgical intervention is indicated for severe shortening and angulation, resulting in severe functional limitations (e.g., severe clinodactyly of the thumb or index finger that impairs pinch).
b. Corrective osteotomy with/without bone grafting at skeletal maturity; may combine with Z-plasty or local flaps if there is a deficit of soft tissue.
c. Partial/bracket epiphyseal resection and fat grafting to prevent fusion across the growth plate.
N. Macrodactyly
1. Definition: Overgrowth of all digital structures
2. Epidemiology
a. Most commonly seen in radial digits
b. Majority are sporadic cases, but can be associated with neurofibromatosis and Klippel-Trenaunay-Weber syndrome
3. Presentation
a. Usually progressive, disproportionate growth and stiffness
b. Growth ceases with physeal closure at skeletal maturity
4. Treatment
a. Challenging to recreate normal appearing digit and frequently requires multiple procedures
b. Growth-limiting procedures: Epiphysiodesis
c. Digit reduction: Soft-tissue debulking
d. Amputation
O. Congenital trigger finger
1. Definition: Flexion deformity due to either thickening of the flexor tendon and/or narrowing of the tendon sheath that is most commonly seen in the thumb and more rarely seen in the other digits (in contradistinction to the adult situation).
2. Incidence: Unclear if presents at birth, or shortly after
3. Presentation
a. Most commonly presents as a flexion deformity at the IP joint and rarely with classic triggering.
b. Notta node: Thickening of FPL tendon which may present as a palpable nodule where tendon cannot pass distally through the tight pulley system
4. Treatment
a. A1 pulley release is typically performed if deformity has failed to resolve by 1 to 3 years of age
b. Notta node or FPL thickening does not require resection or debulking
PEARLS
1. Significant congenital anomalies: More than a simple syndactyly or ulnar polydactyly—warrant evaluation by a geneticist.
2. Reconstructions should keep in mind that the extremity is growing and may need multiple procedures for a final outcome.
3. Never release syndactyly on both sides of the same digit at the same operation for fear of devascularization.
4. Almost never excise skin, just rotate with local flaps into better position: As extremity grows, skin is a premium one cannot afford to be short on.
QUESTIONS YOU WILL BE ASKED
1. Incision designs—
a. Syndactyly release incisions, particularly if no full thickness skin graft planned.
b. Pollicization incisions, Buck-Gramcko versus Ezaki.
2. Wassel-type thumb duplications.
See Table 45-4.
3. What is most common location of syndactyly?
Between middle and ring finger, followed by ring and small finger.
4. What is the most important variable when determining treatment of a hypoplastic thumb? Carpometacarpal ligament stability.
Recommended Readings
Bates SJ, Hansen SL, Jones NF. Reconstruction of congenital differences of the hand. Plast Reconstr Surg. 2009;124(1 Suppl):128e-143e. PMID: 19568146.
Kozin SH. Upper-extremity congenital anomalies. J Bone Joint Surg Am. 2003;85-A(8):1564–1576. PMID: 12925640.
Oda T, Pushman AG, Chung KC. Treatment of common congenital hand conditions. Plast Reconstr Surg. 2010;126(3):121e-133e. PMID: 20811188.
< div class='tao-gold-member'>