New Concepts and Technologies in Reconstructive Hand Surgery
Keywords
• Hand trauma • Tissue engineering • Microvascular anastomosis • Nerve repair
Introduction
In 1944, the pioneer hand surgeon, Sterling Bunnell, described the specialty in these words, “As the problem in hand surgery is composite, the surgeon must also be. There is no shortcut. The surgeon must face the situation and equip himself to handle any and all of the tissues in a limb.”1 Nearly 70 years later, this principle remains the same, but innovations in all composite tissues of the hand have given the hand surgeon advantages that did not previously exist. Concepts and technologies in reconstructive hand surgery continue to evolve, improving patient outcome and surgeon ease. Intelligently designed devices, bioengineered tissues, allografts, and tissue substitutes will soon be available. The systematic method by which perform finger replantation is performed, from bony fixation to skin closure, provides a platform for discussion of the newest innovations available to reconstructive hand surgeons.
Bone
Innovative Solution
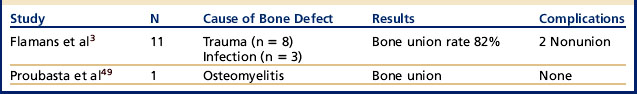
Initially described by Masquelet and Begue2 for large diaphyseal bone defects caused by tumor resection, trauma, or osteoarthritis, the induced membrane technique is a two-stage procedure allowing bone reconstruction. The concept is to place space-maintaining material in the region of the defect. This leads to a foreign body reaction, which creates a membrane mimicking the periosteum. Once this is formed, bone graft can be placed in the periosteal sleeve. Recently, Flamans and colleagues3 applied the Masquelet technique to the hand with promising results.
The results in the hand are from studies with small numbers but are promising. There are over 15 other studies investigating this technique in bone reconstruction outside the hand.4–7
Tendons
Problem: the Need for More Tendon Graft Material
Tendons are essential to hand function and are frequently involved in hand injuries. When tendon deficits exist, the current solution is to harvest expendable autologous tendon grafts (ie, palmaris, plantaris) or use tendon allograft. However, the extrasynovial nature of these tendons increases the resulting adhesions at the repair sites and often leads to a suboptimal functional outcome.8
Innovative Solution
Bioengineered tendon constructs first consist of a scaffold—natural or synthetic.9 Some hand surgeons choose to follow Gillies’ reconstructive principle of replacing “like with like” and use decellularized human tendon scaffolds10 from a donor bank. Other surgeons choose collagen derivatives,11 polysaccharides, small intestine submucosa,12 or human umbilical veins13 as natural scaffolds; whereas the synthetic scaffold uses polymers such as poly(a-hydroxyl acid)s, polylactic acid,14 or polypropylene. The ideal candidate remains to be decided. Natural scaffolds have the advantage of a high affinity to host cells allowing tissue ingrowth, but they theoretically are associated with potential risks such as disease transmission. Synthetic scaffolds have the advantage of being free of disease transmission and are easier to manufacture on a large scale. Being synthetic, however, results in less binding with the host’s cells and, therefore, less tissue proliferation. In addition, both types of scaffolds are subject to rejection (immunologic or foreign body reaction). Considerable research is underway, dedicated to creating the ideal tendon scaffold to meet the requirements of biodegradability, biocompatibility, superior mechanical properties, and optimal processing.
The second aspect of tissue-engineered tendon constructs is the addition of cells with regenerative and differentiation potential that can be used to seed these scaffolds. Several lines of cells have been studied, such as tenocytes,15,16 adipose-derived stem cells,17 bone marrow stromal cells,18,19 and fibroblasts. No significant differences were found between these four cell types in their ability to populate the scaffold.20 To date, it is unclear whether reseeding improves the biomechanical properties of these constructs.
The third area of focus includes strategies to further enhance in vivo regeneration and incorporation of tissue-engineered tendons. The most promising concepts include growth factor supplementation,21,22 mechanical stimuli,17,23,24 and contact guidance.
Nerve
Problem: Peripheral Nerve Repair
Peripheral nerve injuries are common and 60% of these are reported to occur in the upper extremities.25 The current gold standard procedure for managing such injuries is a tensionless end-to-end nerve repair. When the defect is so great that an end-to-end suture will create tension, an autologous nerve graft is performed, creating donor site morbidity and uncertain outcomes depending on the host site vascularization and the level at which the injury occurs. The need for peripheral nerve repair and regeneration strategies is, therefore, high on the priority list in research.
Innovative Solutions
Many strategies have been tested, such as sutureless nerve repair using fibrin glue,26 laser activated chitosan,27 and end-to-side neurorrhaphy.28 Nerve conduits are also a popular solution for segmental nerve defects of up to 3 cm29 and have been studied since as early as the late nineteenth century. Different types of conduits exist from biologic (eg, vein, arteries) to synthetic materials (eg, collagen, caprolactone, polyglycolic acid), giving promising results in small series studies. However, randomized studies of a larger scale are needed. Brooks and colleagues30 report the clinical outcome of 132 nerve injuries in a multicenter study for processed nerve allografts with recovery and safety comparable to autografts and better than nerve conduits.
The latest development in nerve regeneration is molecular and cell therapy. The goal is to augment allografts or conduits by adding cells to lower immunogenicity and increase nerve regeneration. Several types of constructs combining allografts or synthetic conduits with cells have been tested, such as adipose-derived stem cells,31 bone marrow–derived stem cells, Schwann cells, or (more recently) dorsal root ganglion cells.32 However, all of these combinations are still in the early stages of experimentation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree