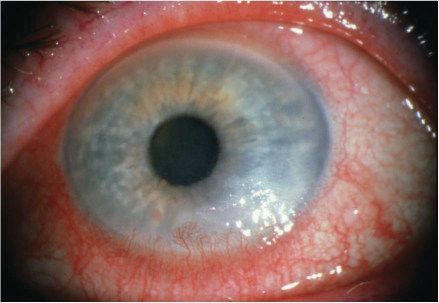
7 Upper eyelid blepharoplasty can have a dramatic restorative affect on the eyes and the face as a whole. However, care must be taken during this delicate operation to prevent its many possible complications. As experience with upper eyelid blepharoplasty has grown over the last century, so has the list of complications. This chapter discusses avoidance and management of complications that may be encountered before, during, and after this surgery. The treatment of complications begins with careful pre-operative assessment of the patient. Certain preexisting conditions are more likely to result in complications or disappointing outcomes. The initial encounter with the patient provides an opportunity to identify and avoid the sources of potential future complications. These conditions do not necessarily prohibit upper eyelid surgery but may need to be addressed before surgery. Determining the patient’s desires, motivations, and expectations of blepharoplasty is an essential component of the initial consultation. Properly motivated patients have a healthy self-esteem and seek restorative changes. The surgeon must determine exactly what bothers the patients about their eyes and whether these conditions can be corrected with surgery. If inappropriate desires, motivations, or expectations exist preoperatively, the procedure is likely to fail to satisfy the patient. A brief psychiatric assessment should be part of every cosmetic preoperative evaluation. Cosmetic surgery patients may have concomitant psychiatric disorders, but this rarely precludes surgery. Body dysmorphic disorder (BDD) is a preoccupation with an imagined or slight defect in appearance that leads to excessive concern and significant impairment in social, occupational, or other areas of functioning.1 In one prospective study, the prevalence of BDD in patients seeking cosmetic eyelid rejuvenation was 13%.2 The authors found that cosmetic surgery patients are no more dissatisfied, critical, or preoccupied with their overall appearance than a nationwide sample of Americans. This contrasts with the common portrayal of cosmetic surgery patients as excessively vain. Most patients seek blepharoplasty to restore their eyes to a previous state and are likely to cope with the postoperative change in appearance. However, patients desiring to dramatically change the shape of the eye must be approached with caution, and a preoperative psychiatric consultation may be indicated.3 When obtaining a past medical history, the surgeon should pay close attention to past bleeding problems and the use of anticoagulant or herbal medications. Those with bleeding disorders or who use anticoagulant medications have an increased risk of bleeding complications following blepharoplasty. Many commonly used herbal medications, such as echinacea, ephedra, garlic, ginkgo, ginseng, kava, St. John’s wort, and valerian, pose a perioperative bleeding risk.4 In particular, garlic,5ginkgo,6 and ginseng7 have been shown to decrease coagulation parameters. The authors request their blepharoplasty patients stop taking all herbal medications 10 days before surgery. During the initial consultation, the surgeon must also inquire about disorders that may lead to poor healing. Diabetes, malnutrition, and immunosuppression constitute relative contraindications for elective surgery. A discussion regarding wound healing preoperatively will help avoid litigation should poor healing lead to a complication postoperatively. A careful medical history allows the surgeon to filter out candidates whose pre-operative health may produce complications and poor outcomes. A meticulous physical examination can identify many potential causes of blepharoplasty complications. While patients commonly present with a desire to remove redundant eyelid skin, close examination often reveals that skin redundancy is caused at least in part by descent of the eyebrows. To make this assessment, it is helpful to understand the anatomic position of the eyebrows in youth. The youthful brow in women lies just above the supraorbital rim and is a gentle arc.8,9 In men, the brow is flatter and lies at the level of the supraorbital rim.10 The surgeon evaluates the contribution of the brow to eyelid skin redundancy by manually elevating the eyebrows to these positions in the office. This often leads to a dramatic decrease in the amount of skin laxity. If the brow position is corrected to the level of the orbital rim, much, if not all, of the skin redundancy is often reduced. After the contribution of the eyebrows to eyelid skin redundancy has been determined, the surgical steps to correct the problem can more accurately be suggested. Excision of the upper eyelid skin without addressing preexisting eyebrow ptosis results in further brow descent and prevents the desired opening of the eyes. Symptoms of soreness, burning, foreign body sensation, or mucoid discharge should raise red flags during an assessment of blepharoplasty patients (Fig. 7.1). Blepharoplasty surgery in those with tear deficiency can aggravate subclinical symptoms into full-blown dry eye syndrome.11 An understanding of the tear film allows the physician to differentiate the causes of dry eye syndrome. The tear film is a trilaminar fluid barrier that bathes the exposed cornea. It contains antibacterial agents, oxygenates the corneal epithelium, maintains a smooth refractive surface, and provides lubrication for eyelid movement.12 The outermost layer of the tear film is a hydrophobic oil layer produced by the meibomian glands and accessory sebaceous glands (the palpebral glands of Zeiss and Moll) that reduces evaporation of the tear film. When this layer is disrupted, evaporative losses may increase 10 to 20 times.13 The middle layer is aqueous and has the largest volume. It is produced by basal secretion from numerous accessory glands (lacrimal exocrine glands of Kraus and Wolfring) plus a stimulated secretion from the lacrimal gland. Basal aqueous secretion decreases with age, leading to a loss in tear volume.11 The deep layer of the tear film is a mucous barrier produced by goblet cells of the conjunctiva. The secretion of mucin by the goblet cells of the conjunctiva increases in response to inflammation. Fig. 7.1 Clinical appearance of a dry eye. Keratoconjunctivitis sicca is the term used to describe eye irritation caused by decreased tear production or increased tear film evaporation. There are many pathophysiologic causes of dry eye, but the most common one is a reduction of the aqueous portion of the tear film. Many systemic disorders are associated with keratoconjunctivitis sicca, including systemic lupus erythematosus, scleroderma, Wegener’s granulomatosis, hyperthyroid states, and rheumatoid arthritis. It is important to identify preoperatively those patients who are likely to develop dry eye symptoms. In one study of blepharoplasty, those more likely to develop postoperative keratoconjunctivitis sicca included men, postmenopausal females, and patients with hypertension.14 The tear deficiency is diagnosed through inquiring about dry eye symptoms and confirming abnormal tear film production. One may be clued into the presence of a dry eye by observing the corneal surface in preoperative photographs: it should appear glass-like. If the light reflex appears rough, as if there is debris on the cornea, further workup should be sought. On exam, an abnormal tear film is recognized by rapid tear evaporation and increased mucus on the eyelid margins. Schirmer testing is perhaps the most useful and easily performed test to establish the diagnosis of keratoconjunctivitis sicca in the preoperative setting.14 The eye is first topically anesthetized to prevent eliciting reflex secretion and the patient is placed in a moderately illuminated room facing away from direct light. Filter paper 35 mm long × 5 mm wide is partially folded at one end and the folded end is placed on the lateral one-third of the lower lid conjunctiva. The patient is then asked to fixate on an object above the direct line of gaze for 5 minutes. Hyposecretion is defined by less than 10 mm of wetting. Normal wetting is between 10 and 30 mm.15 Unfortunately, the results of the Schirmer test in a given patient may vary greatly and it is necessary to perform several tests for each patient. Those who consistently fall below 10 mm of wetting should be suspected of having dry eye syndrome and warrant a complete ophthalmologic workup. Hypothyroidism causes soft-tissue changes throughout the body, including the periorbital soft tissues. In one study, 2.6% of patients seeking a consultation for blepharoplasty were found to have undiagnosed hypothyroidism.16 These patients will attribute the skin changes of their eyelids to aging and excessive fatigue. When examined, they will have characteristic skin laxity and periorbital edema leading to a puffy appearance. Swelling of the periorbital tissues is due to local deposition of mucopolysaccharides. These patients should undergo further evaluation, because the orbital changes generally resolve with adequate treatment of the hypothyroidism.17 Although iodine deficiency is the most common cause of hypothyroidism worldwide, Hashimoto’s thyroiditis, which is caused by anti-thyroid peroxidase (anti-TPO) antibodies, is the most common cause in the United States. If patients suspected of having hypothyroidism have an elevated TSH level on initial screening, a total serum T4 should then be evaluated. Once the diagnosis is made, the patient’s primary care physician may institute treatment. Occasionally, prolapse of the lacrimal gland is encountered on initial examination. This must not be mistaken for fat prolapse and should be evaluated to exclude a malignant, inflammatory, or thyroid hormone-related pathology of the lacrimal gland. Patients with undiagnosed lacrimal gland lymphoma, adenocarcinoma, and metastatic cancer have all presented requesting cosmetic eyelid surgery. The lacrimal gland lies in the superotemporal quadrant of the orbit and is separated into the orbital and palpebral lobes. These lobes are divided by the lateral horn of the levator aponeurosis, through which run the lacrimal ductules. Lacrimal gland prolapse can be diagnosed by everting the upper eyelid and asking the patient to look down. This will accentuate prolapse of the palpebral portion of the lacrimal gland. Comparison between sides and during globe ballottement should also be performed. Repositioning of the lacrimal gland, if necessary, may be performed to elicit a satisfying cosmetic result in upper blepharoplasty. Suturing techniques as well as removal of the orbital fat that surrounds the lacrimal gland have been described.18,19 Poor postoperative results can often be attributed to poor preoperative surgical planning. It is important for both the patient and the surgeon to reach a congruent understanding of the goals for surgery and to share reasonable expectations of the outcome. One of the most common errors in preoperative planning is not taking into account the patient’s ethnicity. The surgeon must respect the patient’s desires for maintaining ethnic traits in the appearance of the upper eyelid Patients are often unaware of asymmetries in their eyelids, and taking standard preoperative blepharoplasty photographs is an important practice. These photographs are reviewed with the patient to demonstrate the small degrees of asymmetry between the upper eyelids. The most important landmark in upper eyelid blepharoplasty is the upper lid crease. When inherent asymmetry exists, attempts to create symmetry between the upper eyelid creases may change the shape and overall appearance of the eyes. It is imperative to identify asymmetries and discuss them with the patient preoperatively to avoid a situation where the patient believes the preexisting condition was caused by the surgery.20 Patients seeking blepharoplasty are often unaware of preexisting upper eyelid ptosis. Blepharoptosis is classified by the extent of superior limbus coverage by the lid margin. It is defined as mild (2 mm or less), moderate (2–4 mm), or severe (4 mm or more).21 Beard classified acquired ptosis by etiology into neurogenic, myogenic, traumatic, and mechanical categories.22 The levator aponeurosis, which normally inserts on the anterior tarsal surface, can become disinserted or dehiscent. Eyelid trauma, ocular surgery, recurrent lid edema of any etiology (i.e., allergic, inflammatory), and idiopathic atrophy of the levator aponeurosis may all lead to upper eyelid ptosis. In the elderly population, acquired ptosis is most often due to senile atrophy of the levator aponeurosis, which is often accompanied by varying amounts of dermatochalasis. Excess skin exaggerates the degree of ptosis and leads the patient to seek surgical correction. In evaluating a patient with eyelid ptosis, the surgeon should inquire about a history of eyelid trauma, recurrent lid edema or inflammation, previous eyelid surgery, or congenital ptosis. The surgeon must also document the onset, duration, and progression of the ptosis. Reviewing old photos of the patient can be useful to illustrate the progress of ptosis. The position of the eyelid relative to the superior limbus in primary gaze should be noted. The superior eyelid margin is normally positioned 1 mm below the superior limbus. If the eyelid falls below this level, the upper eyelid is ptotic.23 The degree of levator aponeurosis function can be documented with a millimeter ruler in front of the eye. Using one or two fingers of pressure over the brow to prevent use of the frontalis muscle, the patient is asked to look down and then upward. The amount of excursion of the eyelid margin is due to levator function. Movement of 4 mm or less is classified as poor function, 6 mm is fair, and 8 mm is considered good levator function.24 In some cases, preexisting ptosis may actually be exaggerated by tightening of the eyelid skin.25 If upper eyelid ptosis is asymmetric, the surgeon should consider Herring’s phenomenon. Herring’s law states that there is equal and symmetric innervation to the frontalis muscle. If asymmetric ptosis is corrected, the stimulus to raise the eyebrows via contraction of the frontalis muscle decreases bilaterally, which then unmasks ptosis on the less affected side. Myasthenia gravis is an autoimmune phenomenon mainly affecting young women that causes upper eyelid ptosis. Ptosis that gets worse as the day progresses is the hallmark of this condition. While the Tensilon test is the standard method for diagnosis, a simple method of testing for myasthenia in the office is to place a few drops of phenylephrine in the eye. Immediate improvement of the ptosis suggests the presence of underlying myasthenia. This finding should prompt a referral to a neurologist for further treatment and work-up. A high upper eyelid crease suggests the most common cause of upper eyelid ptosis, levator aponeurosis dehiscence. Levator aponeurosis dehiscence can have several causes, including senile aging and intraoperative stretching. It is important, therefore, for the surgeon to be careful to avoid manipulation of an atrophic levator aponeurosis.26
Complications of Upper Eyelid Blepharoplasty
 Preoperative Complications
Preoperative Complications
Psychiatric History
Past Medical History
Physical Examination
Dry Eye Syndrome
Hypothyroidism
Lacrimal Gland Prolapse
Surgical Planning
Preexisting Upper Eyelid Ptosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree