16 Orthognathic surgery is widely used to correct congenital and acquired dentofacial discrepancies. The principles of orthognathic surgery were developed for treatment of facial disharmony and dental malocclusion; however, the techniques are also useful for consideration of maxillofacial tumor resection and as therapy for obstructive sleep apnea syndrome. Orthognathic surgical procedures can produce a high degree of satisfaction for the patient and surgeon, but they remain challenging in both presurgical planning and surgical execution. The benefits of orthognathic surgery include better masticator function, reduced facial pain, and improved facial aesthetics. However, numerous complications have been reported that can be attributed to improper surgical planning, technical errors, or poor wound healing. These can be loosely categorized as (1) vascular or nerve injuries, (2) temporomandibular joint dysfunction, (3) bone or soft-tissue infections, (4) periodontal disease, (5) change in airway (obstructive sleep apnea) or swallowing function, and (6) psychological problems. The bulk of this chapter is organized according to the complications seen in specific procedures. By reviewing the potential pitfalls that may be encountered in each procedure, this chapter should provide insight to those who perform orthognathic surgery, including head and neck surgeons, oral and maxillofacial surgeons, and facial plastic surgeons. Complications commonly associated with the spectrum of orthognathic surgical procedures are listed in Table 16.1. Of these, special attention will be given to infection and relapse as universal complications associated with all procedures. Infection after orthognathic surgery may be acute or chronic, local or general. Endogenous bacteria, most likely a mixture of anaerobic and aerobic bacteria, cause most postoperative infections. Factors contributing to this in orthognathic surgery populations may be the usage of steroids, the duration of the surgical procedure, the patient’s age, interference with the blood supply to the bony segments, dehydration of the wounds, the presence of foreign bodies or sequestrum, hospitalization in large wards, nutrition, hematoma, and smoking. The surgeon’s experience, a good aseptic technique, and gentle tissue handling are also relevant factors.1 In the classical wound classification, normal orthognathic surgery wounds fall into the Class II category (clean contaminated wound). An infection rate of 10% to 15% can be expected without use of antibiotics, in comparison to Class III wounds, with an expected infection rate of 20% to 30%. In a clean wound (Class I), the probability of infection is approximately 2%.1 Studies dealing with infection after mandibular osteotomies report infection rates ranging from 0% to 18%.2 In maxillary osteotomies, infection rates lower than 6% are mostly reported,3 but in the study of Zijderveld et al. (1999),4 a 52.6% infection rate was found in a placebo medication group with bimaxillary surgery. Table 16.1 Orthognathic Surgery Complications
Complications in Orthognathic Surgery
 Common Complications Associated with Orthognathic Surgery
Common Complications Associated with Orthognathic Surgery
Infection
• Infection • Hardware exposure • Unanticipated fractures • Devitalization of teeth • Malunion and/or nonunion • Malocclusion • Injury to teeth • Gingival recession and/or periodontal complications • Respiratory decompensation • Bleeding • Relapse |
There is some controversy concerning the need for prophylactic antibiotics,4 and many different practices exist. The operator must assess dosage, timing, duration of therapy, and side effects when considering the use of antibiotic prophylaxis. Peterson (1990)5 has outlined the following principles for the rational use of antibiotic prophylaxis in orthognathic surgery: (1) The surgical procedure should involve a significant risk for infection; increased risk is seen with both bone grafts and wound class II (10–15%). (2) Proper antibiotics should be selected. (3) Serum concentrations of the antibiotic should be appropriately high. (4) The chosen antibiotic must be administered in a correct time sequence. (5) The shortest effective antibiotic exposure should be used.
Relapse
Relapse is an unpredictable risk of orthognathic surgery. Many studies reporting relapse have limitations of sample size or the duration of follow-up, involve different surgical techniques being applied in the same sample, or suffer from limitations in the application of cephalometric measurements. Relapse may be dental, skeletal, or both.
In general, mandibular advancement appears to be stable if rigid internal fixation is used6–8 and if anterior facial height is maintained or increased.9 Several factors may affect relapse in mandibular advancements: the surgeon’s skills; proximal segment control, including condylar positioning and prevention of proximal segment rotation; prevention of counterclockwise rotation of the distal segment in cases with a high mandibular plane angle; the degree of mandibular advancement; and the stretching of the perimandibular tissues, including skin, connective tissues, muscles and periosteum.10 Mandibular setback is not always stable, and the inclination of the ramus at surgery appears to have an important influence on stability.9
The stability of maxillary osteotomies is affected by the magnitude of the anterior movement and the magnitude of the inferior repositioning of the maxilla, the adequacy of mobilization of the downfractured maxilla at surgery, the extent of bone contact in the newly established position of the maxilla, and the type of fixation.11 On the other hand, Louis et al. (1993)12 did not find any correlation between relapse and the magnitude of maxillary advancement. The most stable maxillary procedure is superior repositioning, and forward movement is also reasonably stable. Inferior repositioning is the least stable, especially if it causes downward rotation of the mandible and stretching of the elevator muscles of the jaw. Proffit et al. reported that the least stable orthognathic procedure is transverse expansion of the maxilla.9
 Complications of Mandibular Surgery
Complications of Mandibular Surgery
Bilateral Sagittal-Split Osteotomy
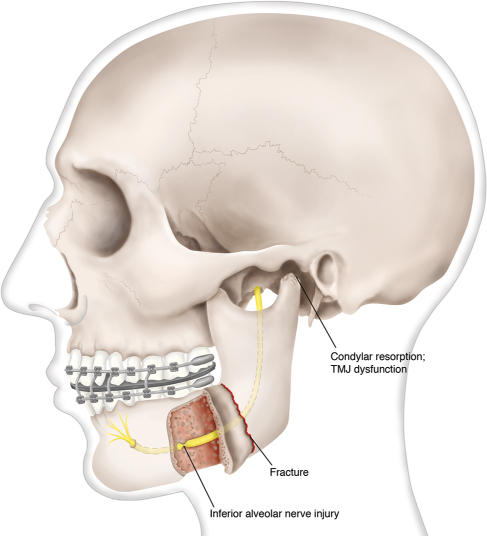
The most common procedure to correct mandibular deformities is the bilateral sagittal-split osteotomy (BSSO), which is useful for both mandibular setback or advancement (Fig. 16.1). The most commonly reported complications for BSSO are listed in Table 16.2.
Fig. 16.1 Illustration of the potential complications that can occur with the bilateral sagittal-split osteotomy procedure. (Illustration by Robert Brown.)
Table 16.2 Bilateral Sagittal-Split Osteotomy (BSSO) Complications
• Unanticipated fracture or unfavorable split • Nerve injury • Bleeding (inferior alveolar artery, masseteric artery) • Proximal segment malpositioning • Temporomandibular joint dysfunction • Condylar resorption • Avascular necrosis • Interfragmentary incompatibilities • Distal segment interference with large setbacks. |
Unanticipated Fracture or Unfavorable Splits
Fractures of the osteotomized segments in BSSO (i.e., bad splits) have been reported to occur in 3 to 23% of cases.13–15 Proper corticotomy technique is the first line of prevention. Many modifications (Hunsuck,16,17 Epker,18 Wolford19) of the initial procedure by Dal Pont20 have lessened the chance of unfavorable splits. Of great importance is the position of the burr or saw blade during the medial ramus cut that must be angled parallel to the mandibular occlusal plane. Likewise, adequate but minimal visualization of the lateral ramus allows for appropriate positioning of the medial cut and avoids risking a horizontal ramus fracture. Removal of a small amount of the internal oblique ridge with a large burr in the area of the proposed medial ramal cut may enhance visualization.21 The vertical lateral corticotomy of the mandibular body should penetrate only the cortex. The corticotomy that connects the medial and lateral corticotomies should be as lateral as possible while still remaining inside the lateral cortex. The inferior border osteotomy must be cut through both cortices to enhance a favorable split. The only time one would not want to cut through both cortices is when an inferior border saw is used.22
Some surgeons remove mandibular third molars during the BSSO,23,24 but most authors routinely recommend this at least six months before BSSO surgery. This allows time for bone healing and helps ensure a favorable split. Often the third molars are not in the center of the buccal and lingual plates, thus increasing the chance of an unfavorable split if they are removed at the time of a BSSO.
Steps to prevent an unfavorable split include careful use of a bibeveled chisel to complete the split after the medial and lateral osteotomies. Another technique uses a Smith spreader to enhance separation of the segments. While inspecting the bone separation, the surgeon adjusts the chisel position to help prevent unfavorable fractures or injury to the inferior alveolar nerve. While the surgeon separates the bone segments, the nerve is carefully released from the proximal segment. A proper split is ensured when the proximal and distal segments have independent movement. A finger on the medial aspect can ensure the proximal (condylar) segment is not moving while minimally moving the distal (tooth-bearing) segment. This technique prevents transmission of heavy prying forces to the proximal and distal segments.
If an unfavorable split occurs, it is most important for the surgeon to decide whether to proceed with the planned procedure or to return the fragments to their native location and abort the surgery. If the surgery is not aborted, the key feature of treatment on an unfavorable fracture is rigid plating. The initial management is to ensure that the osteotomy is completed and that separation of the condylar segment from the distal (tooth-bearing) segment has occurred. The free fractured pieces are fixed to the repositioned mandible with miniplates, making sure the condyle is seated. This can be challenging even in the hands of an experienced surgeon. Depending on the stability of the segments, one may choose to monitor the postoperative occlusion without intermaxillary fixation (MMF) or elect to place the patient in MMF for eight weeks. Counterclockwise rotation of the proximal segment is the most common indicator that healing is delayed and that migration of the fragments has occurred. Periodic radiographs (Panorex) will monitor the condylar and ramal position and bone healing. A second surgery to create osteotomies and bone graft may be warranted if nonunion or malunion is identified.
Nerve Injury
Nerve injuries in orthognathic surgery can be caused by indirect trauma (e.g., from compression by surgical edema), direct trauma with surgical instruments, or stretching during manipulation of the osteotomized bone segments.14 The most common sensory nerve injury with BSSO occurs to the inferior alveolar nerve (IAN) as it courses through the mandibular canal. The risk of injury to the IAN is a significant disadvantage of the sagittal-split osteotomy. The incidence of transection is reportedly 2–3.5%.24 A long-term neurological deficit reportedly occurs to some degree in 10–30% of patients, although not all are symptomatic.25 When a sagittal-split osteotomy is combined with genioplasty, nearly 70% of patients have some degree of neurosensory deficit after one year.26,27 Patients must accept this tradeoff between benefits and risks before undergoing mandibular surgery. Several factors have been identified that may predispose a patient to IAN injury, including age, the magnitude of mandibular movement, position of the inferior alveolar nerve, concomitant genioplasty, the surgeon’s skills, and the degree of manipulation of the IAN.14,28,29 Even with careful manipulation of the IAN, persistent sensation disturbances are possible.30–32 The most dependable way to prevent this complication is a controlled osteotomy under direct vision. The inferior alveolar nerve is particularly vulnerable at the anterior aspect of the split, but it may be damaged anywhere from the pterygomandibular space to the vertical osteotomy site. Errant and aggressive drilling, sawing, or chiseling can damage the nerve at any point along its course.
When the IAN has been injured or transected during a procedure, an immediate attempt should be made to assess and repair the damage. Options include apposition of the nerve segments or primary neurorrhaphy, but proximal and distal nerve segments may need to be released from the bone as far as the mental foramen to provide a tension-free closure. There is no reported correlation between operator-observed partial injury and postoperative neurosensory changes.33 Therefore, extensive dissection must be weighed carefully, and conservative management may be the best choice.
Lingual nerve sensory deficits occur less frequently than IAN sensory disturbances. The initial postoperative incidence has been reported between 1% and 19%;34,35 however, lingual nerve sensory deficits tend to resolve over time. Tissue retraction along the medial mandible and bony fixation methods are the proposed mechanisms of injury.
Facial nerve paralysis is a devastating outcome of BSSO. De Vriese et al. reported a low incidence (0.26%) of facial nerve injuries in a series of 1747 BSSO cases.36 Steps to prevent this complication include careful subperiosteal elevation and chisel orientation. Facial nerve injury is more common in mandibular set-back procedures done for prognathism.37 Damage to the marginal mandibular branch of the facial nerve is a well-known complication of extraoral approaches to the mandibular ramus or angle, but these approaches in orthognathic surgery are rare. The presumed traumatic mechanisms have included compression caused by retractors placed behind the posterior ramus, fracture of the styloid process, and direct pressure as a result of distal segment setback. The prognosis is better if there is incomplete loss of function, and worse if the loss of function is immediate and complete.38
If facial nerve injury is suspected, the surgeon should provide ample time for the effects of local anesthesia to dissipate. If facial paralysis evolves gradually over a period of days, it may be assumed that a complete return of function will occur over time. If, however, complete paralysis is encountered early, standard facial nerve studies are warranted (e.g., nerve excitability testing or electroneuronography. Evoked electromyography (EMG) is an additional test that can help predict return of function.39 Nerve exploration with reanastomosis and possible sural nerve grafting may be considered. Protection of the eye with lubrication, moisture chambers, or eyelid taping should be emphasized to prevent corneal exposure and keratopathy.
Bleeding
Uncontrolled hemorrhage may result from either a mechanical disruption of the blood vessels or a congenital or acquired coagulopathy.40 The most common cause of hemorrhage in orthognathic surgery is a lack of surgical hemostasis.41 Factors contributing to immediate or secondary hemorrhage may include variations in anatomy (bone or vascular), aggressive dissection, tearing of the periosteum during dissection, and hypotensive intraoperative anesthesia with postoperative hypertension. A more rapid recovery by the patient has been reported when major bleeding is avoided.42 Prevention of bleeding begins with the patient history. Reports of prior bleeding experiences or a family history suggestive of coagulopathy warrant preoperative coagulation studies.
The most likely sources of bleeding include the inferior alveolar and the masseteric arteries. The inferior alveolar artery courses with the IAN through the mandibular canal and is contained within the pterygomandibular space. Bleeding from this vessel should be treated by pressure, packing, thrombin spray, and possibly even ligation or cautery once the IAN has been identified and retracted. The masseteric artery is not commonly encountered during a controlled dissection.
The facial artery and retromandibular vein are placed at risk if the lateral mandibular periosteum is violated. Proper dissection for a BSSO should require very little lateral mandibular ramal dissection. Transcervical exposure may be necessary to control hemorrhage if packing, direct control with bipolar cautery, or thrombogenic agents are unsuccessful. A pressure dressing may be warranted if immediate postoperative swelling and hemorrhage are seen. If any signs of airway compromise or of rapid expansion of the oral cavity or neck occur, an immediate return to the operating room is warranted for exploration and evacuation of a hematoma.
Temporomandibular Joint (TMJ) Dysfunction
Temporomandibular joint (TMJ) dysfunction must be carefully assessed and discussed preoperatively. Although some patients have improvement of symptoms after orthognathic surgery, others may develop symptoms. Fibrous ankylosis or joint hypomobility following orthognathic surgery has been proposed to be caused by several factors: immobilization of the TMJ by MMF,43 iatrogenic posterior displacement of the condyle, intra-articular hematoma,44 or excessive stripping of the periosteum and muscle attachments in the ascending ramus, which can result in myofibrotic tissue formation.45 Multiple pharmacologic therapies (e.g., doxycyline, vitamin C) have been suggested to help stabilize the joint and may be helpful.
Condylar Resorption
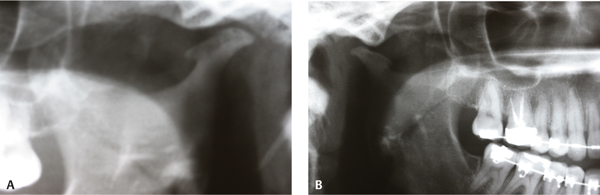
The importance of the preoperative assessment of TMJ health with a detailed history, centric-mounted models, and radiographic exams (lateral cephalogram, baseline tomographs, and Panorex) must be emphasized (Fig. 16.2). The final outcome of the surgery may be altered if the condyles are not seated during the modeling. Several risk factors for condylar resorption after orthognathic surgery have been proposed. Preoperative morphological or functional factors include radiological signs of osteoarthrosis, TMJ dysfunction, a posteriorly inclined condyle, a high mandibular plane angle, and a low posterior-to-anterior facial height ratio.46–51 Contributing surgical factors include major mandibular advancement, counterclockwise rotation of the mandibular proximal fragment, rigid internal fixation with incorrect placement of condylar head, or avascular necrosis of the condyle.46,48,49,51,53–55 Young females (15–30 years) have a higher risk for condylar resorption than males and older females.47,48,50,51,56 The incidence of postoperative condylar resorption has been reported to vary from 1% to 31%. This wide range probably reflects the great variation in the study populations.46,49,57,59 Rigid fixation is the most successful way to avoid osteotomy slippage and condylar resorption. Postoperative recommendations are varied and are not standardized. It may be unwise to reoperate on a patient with condylar resorption, as further revision osteotomies may compound the problem. Mandibular splinting may provide relief from myofascial pain if it is present. If the patients fit a high-risk profile as outlined above, often preoperative splinting by the their orthodontist may help prevent further condylar resorption.
Fig. 16.2 (A) Radiograph of the left mandibular condyle depicting severe condylar resorption prior to orthognathic surgery. (B) Radiograph of same patient showing the resorption of the right condyle.
Proximal Segment Malposition
Prevention of an undesirable proximal mandibular segment rotation or position begins with careful preoperative planning. Intraoperatively, the inferior border of the proximal and distal mandibular segments should be used as a landmark for correct vertical positioning. Introduction of a rotational component makes alignment more difficult. The inferior border of the distal or proximal segment may lie in a different plane if the mandibular segments are rotated clockwise or counterclockwise. Rigid fixation will help to prevent motion and migration of the planned advancement or setback.59 Fixation of the proximal segment may also be achieved with either an inferior border wire or a combined superior border wire and MMF.60
Postoperatively, a physical exam and determination of the patient’s comfort with occlusion are paramount to diagnosing malpositioning. Even when there is an anomaly on a Panorex radiograph, if the patient has no occlusal complaints, observation may be warranted. A more serious problem occurs when shifting of the proximal segment becomes evident. There may be shifting of the mandibular midline or an open bite deformity present that indicates malposition of one or both condyles. This may occur at any time following surgery; however, if it is noted in the first three weeks, it may be reasonable to place the patient in MMF again to allow for additional wound healing and fracture line security. Delayed malalignment often necessitates surgical intervention with osteotomies and bone grafting.
Intraoral Vertical Ramus Osteotomy
Intraoral vertical ramus osteotomy (IVRO) may be used for mandibular setbacks. The operation can be performed more quickly and with less morbidity than BSSO, but it offers less control of the proximal segment and often results in condylar sag, with resultant open bite deformity. IVRO is indicated in cases that require vertical changes between the proximal and distal segments and involve a mandibular setback on at least one side. Hemifacial hyperplasia is one example. The most common complications of IVRO are listed in Table 16.3.
Condylar Sag
Condylar sag is the lack of proper seating of the condylar head in the glenoid fossa. One method that some surgeons use to avoid condylar sag is to overcompensate in the presurgical workup by providing a posterior open bite in the planned postoperative occlusion. During MMF, the posterior space can be built up slightly with an occlusal wafer. If it is removed before complete healing, closure of the open bite may rotate the osteotomy site. On the other hand, if the splint is removed following complete healing, the condyles are seated using light guiding elastics instead of heavy elastics that may place excessive stress on the condylar head.
Table 16.3 Intraoral Vertical Ramus Osteotomy (IVRO) Complications
• Condylar sag • Bleeding • Nerve Injury • Inappropriate osteotomy • Anterior open bite |
Bleeding
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree