8 Complications are an inevitable part of surgery, and eyelid surgery is no exception. Despite the best efforts during preparation, events may not unfold as planned, and unanticipated complications unavoidably occur. A thorough knowledge of potential complications in order of likelihood and importance is paramount for achieving the best possible outcome, not simply to minimize the occurrence of these events but also to provide the best evaluation and management of such events should they arise. A meticulous preoperative evaluation is important, including an appropriate ocular examination and an assessment of the patient’s expectations. The practitioner should assess and document any factors that may affect surgical outcome, such as previous surgery, orbicularis and facial nerve function, lagophthalmos, tear film instability, prominent eye configuration, and preexisting chemosis or edema. If possible, the use of anticoagulation should be discontinued to decrease the risk of intraoperative and postoperative bleeding. Diplopia after blepharoplasty may be a consequence of edema, and it often resolves with time.1 Diplopia may also occur from extraocular muscle injury from anesthesia, intramuscular hemorrhage and edema, and cicatricial changes within the muscle or adjacent connective tissues.1–3 Management of postblepharoplasty diplopia should be conservative, with the use of corticosteroids as appropriate. In rare cases the diplopia may be permanent and require muscle surgery to reduce the symptoms of double vision. Postoperative hemorrhage can occur with blepharoplasty, with sequelae ranging from annoyance to loss of vision. The bleeding is most often from the vessels associated with the orbicularis.4 Only in rares cases are the deep orbital vessels the source of postoperative bleeding. Following cutaneous lower blepharoplasty, bleeding can lift the flap from the underlying septum and orbital fat. This presents as a superficial hemorrhage or organized hematoma. It can be differentiated from orbital hemorrhage by the absence of proptosis, decreased extraocular motility, bloody chemosis, and deep orbital pain. Hemorrhage below the skin flap results in increased postoperative inflammation. If there is substantial inflammation in the plane of the orbicularis and orbital septum, the risk of postoperative fibrosis and of eyelid retraction is increased. Treatment of superficial hematoma is primarily conservative. The use of orticosteroids should be considered to break the cycle of inflammation and decrease the risk of lower eyelid retraction. After five to seven days, eyelid massage with lower eyelid stretch elevation can be employed, and for early chemosis with lower eyelid retraction in the first week, temporary tarsorrhaphy with eyelid suspension sutures to the eyebrow should be considered. A substantial localized hematoma that is organizing should be drained, consistent with surgical principles of any facial flap surgery (Fig. 8.1). The deep orbital hemorrhage is the most worrisome postoperative complication of blepharoplasty: arterial pressure can build up in the closed compartment of the orbit.5 If the orbital pressure rises above the capillary filling pressure of the posterior ciliary arteries (or less likely, the central retinal artery), there is potential for ischemia of the optic nerve and retina, which can lead to loss of vision. Treatment of orbital hemorrhage is emergent. Permanent ischemic damage can occur in 90 minutes or perhaps even less. The symptoms of orbital hemorrhage include severe deep orbital pressure, pain, and nausea; firm orbit with proptosis; limitation of extraocular movement; hemorrhagic chemosis; and decreased or lost vision with unresponsive pupils (afferent pupillary defect). When orbital hemorrhage is causing ischemic optic or retinal changes, urgent treatment to decrease the orbital pressure and restore capillary perfusion is required. Opening the wound and releasing any clots is the first-line treatment and is almost always effective; it may be necessary to spread gently within the orbital tissues to release any loculated hemorrhage. Lateral cantholysis with complete release of the lateral canthal tendon is the next step in the ladder of treatment. In rare cases, bony orbital decompression could be considered. Pericentesis (removing fluid from the anterior chamber) should be considered only as a last resort. Pain and anxiety should be treated. Hypertension should be treated, although an abrupt severe reduction in blood pressure could theoretically compromise arterial filling pressure. Medical treatment of the orbital pressure, including steroids, osmotics such as mannitol, and diuretics such as acetazolamide, can be started, but their use should not delay the implementation of surgical reduction of orbital pressure. Because of the importance of early treatment, both the patient and the staff should understand the significance and urgency of the symptoms of orbital hemorrhage. Fig. 8.1 A superficial hematoma usually resolves spontaneously, but an organized hematoma should be drained. Used with permission from Regents of the University of California, Copyright 2009. Dry eye symptoms are common after blepharoplasty, and chemosis occurs in a significant percentage of patients with dry eye after blepharoplasty.6–8 Risk factors include previous history of dry eye or ocular surface disorders, previous LASIK refractive surgery, and mechanical factors predisposing the patient to poor blink function (prominent eye, lower eyelid laxity, orbicularis weakness, neurologic or myogenic conditions affecting blinking or eye movements, or Graves’ orbitopathy). In this setting, the term dry eye is a misnomer, because these patients usually have adequate tear production. In fact, their eyes are often wet or tearing because of reflex tear production in response to irritation. The mechanism of surface irritation and dry eye symptoms following blepharoplasty relates to dysfunction of the tear-spreading or “windshield wiper” function of the eyelid. Loss of the squeegee effect of the normal blink leads to disruption of the smooth tear film, abnormal evaporation of tears, symptoms of blurred vision (related to loss of the smooth tear film surface), and foreign body sensation or burning pain. The resulting inflammation, potentially combined with generalized postoperative swelling, leads to conjunctival swelling or chemosis. When the conjunctiva becomes chemotic, it creates an additional mechanical impediment to the ability of the eyelid to create a smooth tear film. A vicious cycle of increasing chemosis can occur, leading to mechanical disruption and drying out of the ocular surface (Fig. 8.2). Fig. 8.2 Conjunctival chemosis relates to general edema and also to abnormal eyelid tone with failure of mechanical protection. Used with permission from Regents of the University of California, Copyright 2009. The differential diagnosis of wound granulomata includes foreign body (including sutures), ointment granuloma related to the oily vehicle retained inside the tissues, and atypical infection (including mycobacteria).8,9 Postoperative granulomata can be initially managed conservatively, for example with steroids or 5-FU injections, but persistent or atypical granulomata should be cultured for mycobacteria (Fig. 8.3). Fig. 8.3 Eyelid granulomas appearing two weeks after blepharoplasty surgery; I&D with culture revealed atypical mycobacteria. (Used with permission from Regents of the University of California, Copyright 2009.) Lower eyelid retraction following blepharoplasty is a difficult problem. I am not aware of good data to assess the incidence of this complication accurately, but certainly it is the most frequent postsurgical referral in an urban ophthalmic plastic surgery practice: I see three to five new patients every week for consultation regarding management of eyelid malposition, contour problems, or ocular surface problems after blepharoplasty or mid-face surgery. These patients may be angry, frustrated, or despondent; in my experience, eyelid complications are a particularly difficult type of aesthetic surgery complication, because they not only change the appearance of the critically important periorbital aesthetic unit of the face but also create ophthalmic symptoms that can range from annoying to vision threatening. In approachs to the patient with lower eyelid retraction after blepharoplasty, accurate diagnosis is the prelude to appropriate treatment. Every case must be individualized. The unique anatomy and physiology of every case will dictate a treatment plan that may draw from a wide spectrum of medical and surgical treatment options. There are many variations, but I suggest that the etiology of lower eyelid retraction following blepharoplasty can be divided into seven main categories, each of which should be assessed when the patient is evaluated: 1. Orbicularis paralysis 2. Anterior lamellar tightness 3. Middle lamellar tightness 4. Volume collapse 5. Relationship of the globe to its bony support 6. Horizontal laxity 7. Psychological stability and realistic expectations In this section, I will review each of these mechanisms with particular attention to diagnosis and management. In managing the individual patient, the practitioner should assess the contribution of each of the various factors and then design an individualized treatment plan that treats each factor in proportion to its participation in the problem.
Complications of Lower Eyelid Blepharoplasty
 Diplopia
Diplopia
 Hematoma
Hematoma
 Superficial Hematoma
Superficial Hematoma
 Deep Orbital Hemorrhage and Vision Loss
Deep Orbital Hemorrhage and Vision Loss
 Dry Eye and Chemosis
Dry Eye and Chemosis
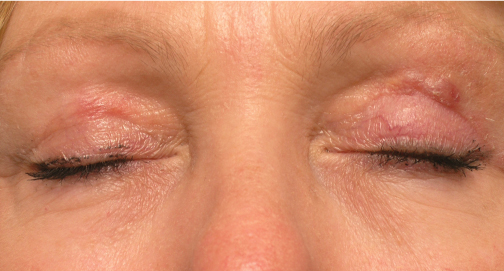
 Wound Granulomata
Wound Granulomata
 Lower Eyelid Retraction
Lower Eyelid Retraction
Orbicularis Paralysis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree