14 Successful management of facial paralysis requires an experienced understanding of its cause, duration, and the prognosis for facial paralysis recovery. Skills in both reconstructive and aesthetic surgery are required to use contemporary techniques to rehabilitate fully the patient with facial paralysis (Fig. 14.1). It is helpful during the consultation process for the surgeon to divide the face into upper, middle, and lower thirds. In each facial region, reinnervation procedures as well as static resuspension procedures are available for the patient. Procedures to be considered first assist with periorbital rehabilitation—procedures that improve eyelid closure, eye protection, and brow position. Such periorbital procedures include techniques to load the upper eyelid, reposition the denervated lower eyelid, and reposition the brow. Midfacial procedures are then considered to correct nasal obstruction, provide support for the retracted lower eyelid, reduce oral incompetence, and improve facial symmetry. These goals are accomplished with procedures such as midface lifts, static slings, free muscle transfer, local muscle transfer, and nerve transfers. Lower facial procedures address oral incompetence, speech difficulties, facial asymmetry, and the inability to smile, and they include procedures such as facelift, necklift, and oral commissuroplasty. This chapter will address the prevention and management of complications in facial paralysis rehabilitiation by region. The most common complication is failure to achieve the desired improvement. Other complications, such as hematomas, failure of wound healing, and infection may also occur. The diversity of patient presentations and treatment options makes this topic quite complex. Therefore, each surgeon must understand the advantages and disadvantages of the procedures and balance those with their comfort level and the procedures’ application to their individual patients. Fig. 14.1 Contemporary management of facial paralysis. This patient was initially treated with gold weight placement, and subsequently underwent endoscopic browlift, lateral canthal suspension with midface lif t, and temporalis tendon transfer. (Chan JY, Byrne PJ. Management of facial paralysis in the 21st century. Facial Plast Surg Aug 2011;27(4):346–357.) Avoidance of complications with facial reanimation begins with the most fundamental aspects of patient care: careful diagnosis and selection of appropriate treatment. It is crucial to engage in thoughtful planning before entering the operating room and beginning a path of treatment that could be inappropriate. Understanding the causes of facial paralysis and its pathophysiology will guide the surgeon’s assessment. Although the differential diagnosis of facial palsy is very extensive, usually a small number of causes account for most cases that present to the surgeon’s office. Trauma, acoustic neuroma surgery, parotid neoplasms, and Bell’s palsy with incomplete return of function compose the bulk of encountered etiologies. Treatment planning requires taking an extensive history, performing a physical examination, and possible testing to determine what procedures may be beneficial to the patient. Initial consultations are often detailed, because subsequent decisions are complex. The surgeon should consider several questions to help guide the decision-making process (Table 14.1). Table 14.1 Questions to Aid with Facial Paralysis Surgical Planning
Complications of Facial Reanimation
 Preoperative Prevention Strategies
Preoperative Prevention Strategies
General Points
What is the etiology and duration of the paralysis? |
What is the prognosis for recovery? |
What is the patient’s age? |
Is the paralysis complete or incomplete? |
Are there areas of hyperfunction in addition to areas of paresis? What troubles the patient most? |
How much tissue laxity is present? |
How compliant is the patient? |
What are the patient’s expectations with regard to outcome, recovery period, and the time necessary to assess the success of an intervention? |
The answers to these and many other questions will direct the thoughtful surgeon’s choices for the timing of any intervention, medical versus surgical management of the eye, static versus dynamic facial suspension, reanimation versus observation for recovery, free tissue transfer versus local muscle transfer versus nerve crossovers, reversible or nonreversible measures, or concomitant contralateral procedures performed to improve symmetry. This analysis can be extensive, and it is required before operating on the patient. More detailed discussion of these considerations is beyond the scope of this text. Nonetheless, this list highlights the importance of the preoperative consultation.
Diagnostic facial nerve testing may be considered before undertaking a surgical procedure. A thorough evaluation and work-up may require imaging studies (CT or MRI) and electrodiagnostic testing. Well-known tests for prognosis include the maximum stimulation test, the nerve excitability test, electromyography (EMG), and electroneuronography (ENOG). Although most cases do not require such testing, it is appropriate in others. This is a topic beyond the scope of this chapter.1
Nonsurgical options may be chosen for management of the patient’s facial paralysis, depending on the individual’s circumstances. A compliant patient, for example, may do well with aggressive medical eye protection. Facial retraining has a role in many cases, and this form of physical therapy may result in improved outcomes, particularly if it is instituted early.
We suggest allotting an appropriate amount of time in the clinic for such a complex discussion with any new facial paralysis patient. We typically allocate more time for this consultation than any other new facial plastic surgery patient visit. Spending one hour on the initial visit is typical. This is the first step toward prevention of untoward outcomes. The patient needs to be educated about multiple issues and must be able to make an informed decision regarding his or her treatment options. A frank acknowledgment of the realistic potential for improvement must be made early. If there has been a complete facial nerve transection, then the chance for a normal outcome does not exist with the current state of medical knowledge. The patient and family need to be made aware of this. The patient and family also need to be engaged in the decision-making process as they consider their options for reanimation.
The Eye
The first priority for facial paralysis management is eye protection. Visual field preservation and correction of eye or brow asymmetry are important but secondary. Procedures to consider include browlifting (direct, coronal, or endoscopic), upper lid loading (gold or platinum weight), and lower lid tightening or elevation (tarsal strip canthoplasty, transorbital canthopexy, spacer grafts, midface lifts). There are several things to look out for to prevent complications. First, perform a careful physical examination. Attention is directed toward the patient’s current ability to protect the eye and also to be aware of chronic exposure. A useful mnemonic to help identify patients who are especially at risk for exposure keratitis is BAD: Look for the presence or absence of a Bell phenomenon (B); if it is absent, that represents a risk factor for exposure keratitis due to diminished ability to protect the cornea. An absence of corneal reflex (A for anesthesia) indicates that the patient is also at increased risk for exposure keratitis due to a diminished ability to sense the irritation that would normally accompany an exposed cornea. A patient with preexisting dry eye (D) has poor tear production and is a higher-risk patient. The risk for corneal exposure complications in patients with dry eyes, absent Bell phenomenon, and diminished corneal sensation is very real. The mental status and compliance of the patient are also important. Appropriate eye protection and lubrication requires placement of lubricating ointment, use of artificial tears, moisture chambers, and eyelid taping. The physician must realistically assess the patient’s ability to follow a course of treatment and if it is compromised, a more aggressive treatment, such as tarsorrhaphy, may be appropriate in select cases.
A careful preoperative evaluation of the upper eyelid will reduce the chance of ptosis caused by loading techniques. The patient is observed and questioned while trying on several sizes of gold weights. This can be facilitated by securing the weight to the lid with double-sided tape. The goal is to maximize closure while minimizing induced ptosis. Some iatrogenic ptosis is acceptable, but only what remains asymptomatic to the patient.
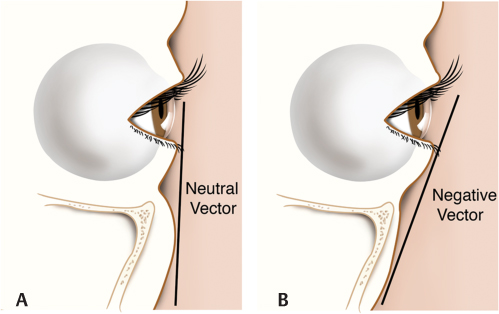
Likewise, the lower eyelid must be carefully examined. Laxity of a paralyzed eyelid may demonstrate ectropion, lid retraction, lacrimal dysfunction, and insufficient globe coverage. Lower eyelid elevation may be accomplished by a variety of methods. The tarsal strip canthopexy is quite commonly performed. However, certain anatomic findings can affect the outcome. For example, patients with maxillary hypoplasia and the so-called negative vector, with relative proptosis, may be done a disservice if canthopexy is performed (Fig. 14.2). Such lower lid tightening may cause the eyelid margin to be pulled under the convexity of the globe, thus worsening lid position and eye protection. Alternative techniques to elevate the lid, such as space grafting and midface lifting, are preferable in such patients.
Midface and Lower Face
The procedures used here include facial nerve grafts, cross face grafts, hypoglossal facial nerve transfers, free muscle transfer, dynamic regional muscle transfer, and static facial slings. Several preoperative considerations are important when the surgeon evaluates a patient for facial reanimation. First, the surgeon must choose a treatment option with a reasonable likelihood of success. Reinnervation techniques of native facial musculature (cross face grafts, hypoglossal nerve (XII)–facial nerve (VII) anastomoses) are unlikely to be successful if they are performed after a prolonged period of denervation. This duration is in most cases approximately one year. Cases of spontaneous reinnervation, as well as successful surgical reanimation, have certainly occurred after delays longer than one year in particular patients; however, this is the exception. The older the patient, the less likely it is that either spontaneous recovery will occur or that reinnervation techniques will be successful.
Fig. 14.2 The negative vector. This refers to an anatomical observation (A) when the cheek tissue at the level of the orbital rim (OR) is posterior to a vertical line drawn from the lower lid margin (LL). A lid tightening procedure (B) could have the undesired result of retraction of the lower lid due to a “sliding” down the globe. (Illustration by Robert Brown.)
Patients who have undergone radiation treatments are more likely to require revisions to static facial slings from descent of the initially suspended soft tissues. Implants may be more likely to extrude after radiation therapy (Fig. 14.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree