Thorough preoperative evaluation with meticulous surgical planning to achieve facial aesthetic balance between the forehead, eyelids, and midface is imperative to avoid or decrease potential functional and/or cosmetic complications in cosmetic periocular surgery. Before performing surgery, the physician should be aware of the patient’s history of dry eyes, previous facial trauma, previous injection of Botox Cosmetic, history of previous laser-assisted in situ keratomileusis, and past facial surgery. A full evaluation should be performed on the upper eyelid/brow region to assess for the presence of brow ptosis, brow/eyelid asymmetry, dermatochalasis/pseudodermatochalasis, eyelid ptosis, and deep superior sulcus. On the lower eyelid/cheek examination, special attention should be directed to the diagnosis of underlying negative vector, dry eyes, prominent eyes, lower lid retraction, ectropion, lateral canthal dystopia, lower eyelid laxity, scleral show, and lagophthalmos, with a rejuvenation goal that focuses on obtaining a youthful fullness through repositioning and reinforcing efforts to avoid the negative effects of hollowness. Intraoperative and postoperative medical and surgical management of cosmetic periocular surgery complications focus on decreasing the risk of postoperative ptosis, lagophthalmos, lid retraction, and lid asymmetry, with special attention to limiting the risk of visual loss secondary to orbital hemorrhage.
The ultimate rejuvenation goal of cosmetic periocular surgery is to achieve an aesthetic balance between the forehead, periocular area, and midface. As patients who seek cosmetic surgery are focused on achieving their ultimate aesthetic result, it is imperative that cosmetic surgeons take the time to focus on the importance of educating patients regarding realistic outcomes and possible complications that may result from the planned procedure. This discussion should emphasize the aging changes that occur in the periocular region, including facial volume loss (deflation), volume shifting (descent), and skin, ligament, muscle, and bone changes, which lead to baggy lids, suborbicularis oculi fat descent, subcutaneous fat loss, and other age-related changes. Cosmetic surgeons should strive to restore fullness with avoidance of procedures/surgeries that result in hollowing and skeletonization. This goal can be achieved by efforts to reposition and reinforce, with an individualized surgical plan for each patient to achieve facial aesthetic balance with a youthful, refreshed appearance.
Because blepharoplasty ranks as one of the most popular cosmetic procedures in the United States, with more than 221,000 cases performed in 2008, thorough preoperative evaluation with meticulous surgical planning is imperative to decrease or even avoid the risk of potential complications (cosmetic and functional) that can occur with facial cosmetic surgery in the periocular region. Possible functional issues following periocular surgery include keratopathy/dry eyes, infection, tearing/ocular irritation, lagophthalmos, hemorrhage/hematoma, diplopia, loss of vision, and/or blindness ( Box 1 ). Postoperative cosmetic problems include asymmetry, deep superior sulcus, periorbital hollowing, lateral canthal dystopia, and unnatural appearance. Complications with functional and cosmetic implications include eyelid malposition, retraction, and ptosis ( Box 2 ). It is imperative that the cosmetic surgeon does not focus on the amount of tissue removed in periocular surgery; instead, the surgical goals should focus on the importance of preservation of tissue to retain a youthful symmetric fullness through repositioning and reinforcing to achieve optimal aesthetic results.
- 1.
Asymmetry
- 2.
Lower lid hollowing
- 3.
Deep superior sulcus
- 4.
Suture milia
- 5.
Lid crease/fold asymmetry
- 6.
Lateral canthal dystopia
- 7.
Eyelid malposition
- 8.
Medial canthal webbing
- 9.
Scarring
- 10.
Chemosis
- 11.
Ptosis
- 12.
Unnatural appearance
- 1.
Dry eyes/keratopathy
- 2.
Tearing/ocular irritation
- 3.
Orbital hemorrhage/hematoma
- 4.
Diplopia/strabismus
- 5.
Visual loss/blindness
- 6.
Lagophthalmos
- 7.
Infection
- 8.
Chemosis
- 9.
Retraction
- 10.
Ptosis
- 11.
Eyelid malposition
History
The importance of obtaining a thorough preoperative medical history should be emphasized because it is imperative to recognize patients who may be at an increased risk for complications from procedures to rejuvenate the periocular region. A history of systemic diseases, such as Graves disease, Sjögren syndrome, rheumatoid arthritis, rosacea, Bell palsy, and myasthenia gravis, or other neuromuscular diseases, should be ascertained. Patients should be questioned regarding a past history of ocular allergies, facial trauma, previous facial surgery (including skin cancer excision), or any previous periocular procedures.
Periocular/ocular examination
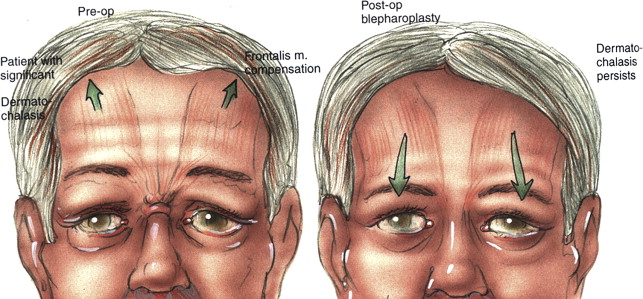
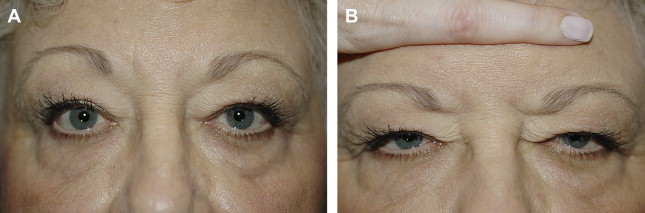
Following the complete review of their history, the prospective surgical candidate should have a complete periocular examination, including the brow, lid, and cheek regions as well as the ocular surface. During the initial consultation it is imperative to document and show any preoperative asymmetry. Patients for upper eyelid/brow rejuvenation surgery should undergo complete evaluation of the periocular area, including documenting the brow position and contour, as both contribute to a person’s expression, whether angry, tired, sad, or happy. The diagnosis of underlying brow ptosis is crucial because patients may have evidence of frontalis muscle contraction to raise the brows secondary to underlying upper eyelid ptosis or significant dermatochalasis ( Fig. 1 ). Because the distance between the brow and lid margin is increased from secondary brow compensation, an aged, tired appearance results. To unmask any underlying brow ptosis, apply manual pressure to the brow region and have the patient look in primary gaze ( Fig. 2 ). In addition to the periocular evaluation, the prospective patient should undergo a complete ocular examination with documentation of best corrected visual acuity, pupil examination, extraocular motility, and a slit lamp examination to evaluate the status of the cornea.
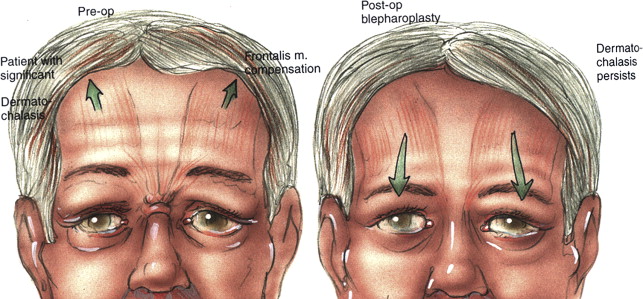
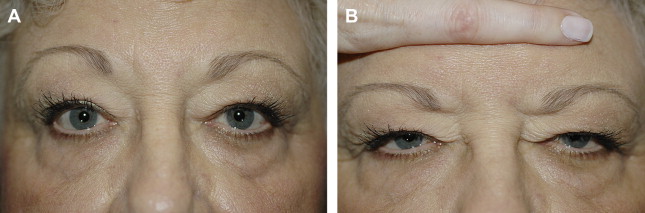
Periocular/ocular examination
Following the complete review of their history, the prospective surgical candidate should have a complete periocular examination, including the brow, lid, and cheek regions as well as the ocular surface. During the initial consultation it is imperative to document and show any preoperative asymmetry. Patients for upper eyelid/brow rejuvenation surgery should undergo complete evaluation of the periocular area, including documenting the brow position and contour, as both contribute to a person’s expression, whether angry, tired, sad, or happy. The diagnosis of underlying brow ptosis is crucial because patients may have evidence of frontalis muscle contraction to raise the brows secondary to underlying upper eyelid ptosis or significant dermatochalasis ( Fig. 1 ). Because the distance between the brow and lid margin is increased from secondary brow compensation, an aged, tired appearance results. To unmask any underlying brow ptosis, apply manual pressure to the brow region and have the patient look in primary gaze ( Fig. 2 ). In addition to the periocular evaluation, the prospective patient should undergo a complete ocular examination with documentation of best corrected visual acuity, pupil examination, extraocular motility, and a slit lamp examination to evaluate the status of the cornea.
Normal eyelid anatomy
In the normal periocular region, the eyelid is shaped like an almond, with the highest point just nasal to the pupil and the brow position higher temporally ( Fig. 3 ). The typical lid crease is around 8 mm, with at least 10 to 12 mm of skin superior to the eyelid crease to allow proper lid excursion and closure. The upper eyelid crease occurs where the uppermost fibers of the levator aponeurosis insert into the overlying lamellae and subcutaneous tissue. The lateral commissure is 1 to 2 mm higher than the medial commissure. The lower lid margin should be in apposition along the entire length of the eye.

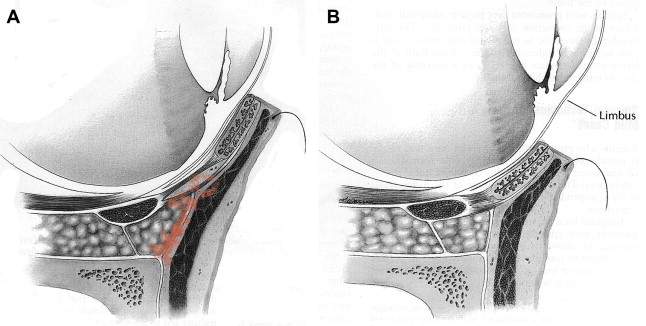
To diagnose pathophysiology of eyelid malposition after lower eyelid blepharoplasty, the surgeon must be familiar with the surgical anatomy. The eyelid is divided into 3 layers: anterior, middle, and posterior lamella. The anterior lamella consists of the skin and orbicularis muscle, the middle lamella is the orbital septum, and the posterior lamella includes tarsus, conjunctiva, and the lower eyelid retractors. Lower eyelid retraction results from inflammation, scarring, shortening, and cicatricial tethering of the middle and posterior lamella ( Fig. 4 ). Patients with a previous history of eyelid/facial surgery or facial trauma are at a higher risk for possible lid retraction. Anatomic factors that can contribute to an increased risk of lower eyelid retraction include prominent eyes, evidence of facial negative vector, midfacial hypoplasia, and scleral show.
Brow/upper eyelid examination
In addition to the evaluation for brow ptosis or asymmetry, the examination for brow/upper eyelid surgery should include the eyelid crease and position, evidence of preexisting lagophthalmos (inability to completely close the eyes), floppy eyelid syndrome, deep superior sulcus, prolapsed lacrimal gland, and/or underlying eyelid ptosis ( Fig. 5 ). The margin reflex distance (MRD1), which represents the distance from the light reflex of the patient’s cornea to the center of the upper eyelid as the patient gazes in primary position, is used to assess the presence of upper eyelid ptosis. The normal MRD1 in an adult is 1 to 2 mm below the superior corneal limbus in primary gaze ( Fig. 6 ).


Assessment of the eyelid-brow complex should occur with the patient in a sitting position, with emphasis on the diagnosis of any brow ptosis, because this may give the false impression of lateral hooding of the upper lids. It is important to emphasize to patients who have evidence of brow ptosis and dermatochalasis that if they decline brow ptosis correction at the time of the blepharoplasty, the final aesthetic results may be compromised. In addition to examining for evidence of brow ptosis, it has been shown that the brow shape has a greater influence than absolute position on perceived expression. It is also important to note the distance from the brow to the upper lid margin because an increased distance, secondary to frontalis muscle compensation, is a characteristic sign of aging in the upper face. It is important to immobilize the brow position during the preoperative evaluation to negate the effects of frontalis muscle compensation, therefore exposing any underlying dermatochalsis or ptosis.
Any signs of ocular surface problems, dry eye syndrome, blepharitis, or eyelid inflammation should be documented in the upper eyelid evaluation. Attention should also be directed to noting any evidence of deep superior sulcus, as the degree of deepness of the superior sulcus is determined by the interplay between the brow fat, preaponeurotic fat pads, orbital septum, and the levator aponeurosis. Many of the issues described earlier can be diagnosed and addressed before or during cosmetic brow or eyelid surgery.
Lower eyelid/cheek examination
With aging, the lower eyelid cheek junction develops an uneven contour secondary to descent of the cheek, with increased prominence of the lower lid fat, resulting in a nasojugal groove with a tear trough deformity. In addition to the evaluation for dry eye syndrome, patients seeking cosmetic lower eyelid surgery should be evaluated for evidence of eyelid malposition, descent of the malar fat pads, poor maxillary bony support with a negative facial vector, stretching of the lateral canthal tendons, eyelid retraction, lagophthalmos, lower lid hollowing, alteration in the tear film/blink reflex, ineffectiveness of the tearing-lacrimal pump, evidence of corneal exposure, eyelid or punctal ectropion, scleral show, and lid laxity. Hester and colleagues found that patients with enophthalmic orbits and significant horizontal lower lid laxity were at an increased risk for postoperative lower lid malposition ( Box 3 ).
- 1.
Dry eye syndrome/Sjögren syndrome
- 2.
Thyroid disease
- 3.
Lower lid laxity
- 4.
Negative vector
- 5.
Scleral show
- 6.
Previous facial trauma
- 7.
Previous facial surgery
- 8.
Psychological issues
- 9.
Unrealistic expectations
The distraction test is performed by pulling the eyelid anteriorly; if the distracted distance is greater than 6 to 8 mm, then lower lid laxity is evident ( Fig. 7 ). The snap back test, which assesses the function of the orbicularis muscle and the amount of lid tone, is performed as the lower lid is pulled toward the inferior orbital rim and released. A fast snap of the lower eyelid to the proper position indicates normal tension, whereas poor snap back shows evidence of poor lid tone ( Fig. 8 ). To examine for lagophthalmos, the patient is instructed to passively close the eyelids as if they were sleeping ( Fig. 9 ).
It is also recommended to check the Bell phenomenon and the amount of lateral canthal tendon laxity. Defined as inferior malposition of the lower eyelid margin without eyelid eversion, lower eyelid retraction is assessed by placing upward traction on the lower eyelid. In normal conditions, the lower eyelid can be raised to at least the midpupil level. If this level is not achieved with raising the lower lid, there is evidence of lower lid retraction ( Fig. 10 ). The development of lower lid retraction from postsurgical manipulation is characterized by inflammation, scarring, shortening, and cicatricial tethering of the middle and posterior lamella. Examination in this region should also include any evidence of lower lid hollowing, which can be managed with the use of dermal soft tissue augmentation; hyaluronic acid is the preferred dermal filler in this region. Many of the issues described earlier can be diagnosed and addressed before or during lower eyelid blepharoplasty.
Dry eye syndrome/ocular irritation
Patients present with ocular irritation from multiple causes, including dry eye syndrome, lower eyelid malposition, lid retraction, lagophthalmos, blepharitis, and alterations in the tear film and/or blink reflex. Dry eye syndrome affects up to 17% of women and up to 12% of men in the general population, and so it is imperative to diagnose and treat this condition before surgery, because the incidence of dry eye syndrome following blepharoplasty is between 8% and 21%.
Ocular surface lubrication can be influenced by quantitative deficiencies such as decreased tear production, qualitative problems in the mucous and lipid layers of the tear film from blepharitis/meibomitis, and also from tear distribution problems secondary to a poor blink mechanism, or from a combination of all of these factors. Dry eye symptoms include discomfort, dryness, burning, stinging, foreign-body sensation, gritty feeling, blurry vision, photophobia, itching, and redness. Risk factors for dry eyes include underlying systemic disease, menopause, previous lid surgery, and history of laser-assisted in situ keratomileusis (LASIK). Preoperatively, patients should be assessed for possible dry eye syndrome with a Schirmer test. The Schirmer strip is inserted in the lower eyelid at the lateral limbus after a topical anesthetic drop has been inserted into the eye ( Fig. 11 ). After 5 minutes, the Schirmer strip is removed and a measurement is recorded; normal measurements are between 10 and 15 mm of wetting. If the measurement is significantly less than 10 mm, then the patient has evidence of hyposecretion of tears with dry eye syndrome. Although the results of Schirmer testing may be inconsistent, the test is beneficial for documenting evidence of severe dry eyes. With cosmetic blepharoplasty, patients with dry eye syndrome may experience worsening of their condition, and in severe cases it may even be a contraindication to surgery.
Saadat and Drenser discussed that by preserving the orbicularis muscle and its innervation, blepharoplasty could be safely performed in patients with dry eyes. The dynamics of eyelid closure, including tear pumping and tear distribution, are not affected with preservation of the orbicularis muscle and its innervation. Fagien noted not only the importance of the preservation of the orbicularis muscle from a functional standpoint but also for improved cosmetic results by retaining a youthful fullness to the upper eyelid region. Cosmetic surgeons must be aware of the long-term implications of lid surgery from an aesthetic and functional standpoint to assure correct lid position and closure for adequate corneal protection and ocular lubrication.
Normal tearing is divided into 3 components:
- 1.
Production and release of tears from the lacrimal gland and accessory glands
- 2.
Blinking and distribution of tears
- 3.
Tear pumping into the lacrimal drainage system.
As discussed earlier, the action of the orbicularis muscle is responsible for the second 2 components. With preservation of the orbicularis muscle and its innervations in transconjunctival lower lid blepharoplasty, there is a decreased incidence of complications of retraction, scleral show, and lacrimal pump problems compared with the external skin-muscle flap technique. Hester and colleagues recommended eliminating trauma to the orbital septum lower lid during blepharoplasty by avoiding the plane between the orbicularis muscle. When performing transconjunctival lower lid blepharoplasty, either a pinch technique or laser resurfacing can be used to address lower lid rhytids.
Orbital hemorrhage
The most feared complication of periocular surgery is loss of vision or even blindness secondary to orbital hemorrhage. The risk of orbital hemorrhage is 1 in 2000 and the risk of orbital hemorrhage with visual loss is 1 in 10,000. During the preoperative evaluation, patients’ risk factors should be identified to decrease the risk of this devastating outcome. Included among risk factors for orbital hemorrhage are antiplatelet or anticoagulant medications (including homeopathic or herbal medications), history of hypertension, and history of abnormal bruising or bleeding or underlying disease that may contribute to bleeding. It is important to obtain a complete history of the patient’s medications, including vitamins and herbs, which affect coagulation. Preoperatively, patients should be instructed to discontinue Coumadin, aspirin, nonsteroidal antiinflammatory drugs (NSAIDs), vitamin E, omega-3 fatty acids, garlic, and other supplements or herbs with blood-thinning effects. The patient should also be provided with a list of medications that affect coagulation; the author’s surgical counselor periodically updates this list ( Fig. 12 ). Many surgeons also recommend having patients take Arnica montana , vitamin K, and bromelain in an attempt to limit postoperative edema and ecchymoses.
Haas and colleagues found comorbidities of orbital hemorrhage included past history of hypertension, preoperative aspirin intake, postoperative vomiting, and postoperative physical activity. These investigators also noted an increased risk of orbital hemorrhage during the first 3 hours following surgery, with the risk decreasing 24 hours after surgery, although Teng and colleagues reported a patient who presented with an orbital hemorrhage 9 days following a cosmetic blepharoplasty that resulted in permanent visual loss.
Intraoperatively, emphasis should be directed to controlling the blood pressure to decrease the risks of bleeding. Secondary to the vasodilation effects from general anesthesia, local anesthesia is preferred. To achieve the maximum vasoconstrictive effects of epinephrine after the administration of local anesthesia, it is important to wait at least 15 minutes before starting surgery. Meticulous dissection of the orbital fat pads is important to avoid traction and decrease the risk of posterior orbital bleeding, with particular attention to cauterization of any pinpoint areas of bleeding from the orbicularis muscle before skin closure.
Orbital hemorrhage in the postoperative period is the leading cause of visual loss from cosmetic eyelid surgery, therefore early detection and treatment are critical. Postoperative checking of vision is recommended and patients should be encouraged to call their physician immediately with any signs of decreased vision, pain, or rapidly increasing edema. Physicians should be available to see patients in a timely fashion if patients experience any of the signs or symptoms described earlier. Patients are encouraged to avoid bending, lifting, and straining; they should rest with their head elevated and ice packs should be applied for 30 minutes every hour while the patient is awake for the initial 2 to 3 days following surgery.
Infection
The risk of postoperative infection following periocular surgery is low secondary to the rich vascular supply of the eyelids. Carter and colleagues reported the infection rate at 0.2% in patients who had undergone upper or lower blepharoplasty without laser resurfacing and slightly higher at 0.4% in patients who had adjunctive laser resurfacing in addition to blepharoplasty. Postoperative infections typically present between 4 and 7 days after surgery. Carter and colleagues recommend the routine use of topical antibiotic ointment as a sufficient postoperative treatment regimen for patients undergoing blepharoplasty without the need for prophylactic systemic antibiotics.
Periocular laser resurfacing
Complications related to periocular laser resurfacing include scarring, hyperpigmentation, hypopigmentation, long-lasting erythema, and infection. A prophylactic antibacterial and antiviral systemic regimen is typically initiated a few days before the procedure and continued for 1 week postoperatively. Intraoperatively, feathering of the laser passes is recommended between treated and untreated areas to limit possible demarcation lines. Conservative treatment with laser resurfacing is also recommended along the angle of the mandible because this area can scar easily.
Postoperative wound care is focused on resolution of erythema, avoiding infections, and limiting postinflammatory hyperpigmentation. Topical applications of Aquaphor or Vaseline combined with hydrocortisone 1% cream and dilute cool solutions vinegar soaks are used during the postoperative period. Sun protection is recommended with sunscreen with a sun protection factor of 30 or greater following the laser treatment, and postoperative hyperpigmentation can be treated with Hydroquinone 4% cream as necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






