CHAPTER 55 Cohesive gel breast augmentation
History
Form-stable cohesive gel implants are currently available in the US only through FDA PMA (premarket approval) clinical trials; however, they have been available internationally since 1993. There has been some confusion regarding what actually is a cohesive gel implant. Although all implant fillers are cohesive in the physical sense (saline or gel) the reality is that the term cohesive gel implant has traditionally meant a form-stable device (i.e. Inamed 410, Mentor CPG). The distinction is cogent as the benefits of form-stable implants that have been realized to date are a direct function of the form stability of the filler. Thus, surgeons and patients must understand these important differences.1–3
Physical evaluation
Breast augmentation is a process, and includes the following important components:
1. Patient education and informed consent.
2. Tissue-based clinical planning.
3. Refined, systematic surgical technique.
The data to support this process include independently published, peer-reviewed series and presented series at national meetings.4–9 All include reoperation rates of 3% or less (compared to the standard 15–20% from PMA studies over the past 15 years).
• Patient education is the most essential of all, and should give patients ample time through written material and patient educator sessions to define on paper what their expectations are.
• This is followed by a surgeon’s consultation, to perform tissue-based implant selection and compare this to the desires which the patient defined during the education portion. Any discrepancies are reconciled and the patient is able to make final choices based on the comprehensive knowledge provided.
• Tissue-based clinical planning is performed with the High 5 Process.10 This is a refinement of previous generation planning systems and allows the surgeon to focus on the five critical decisions that determine outcomes in breast augmentation.
• The five decisions determined are:
• The goal is to have all key decisions made during the consultation and prior to going to the operating room.
Technical steps
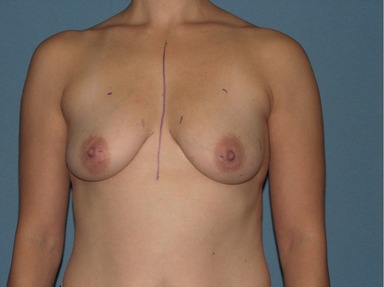
The patient is marked in the preoperative area (Fig. 55.1). The planned width and height of the selected implant are marked on the chest wall skin to facilitate the dissection and the incision is planned. Full general anesthesia with short-acting muscle paralysis is used. After induction, 2–3 mL of 1% lidocaine with epinephrine is injected in each incision to minimize skin bleeding. After standard prep and drape the nipple areolar complexes are covered with a small sterile tegaderm. The paradigm and principles for pocket dissection have changed from non-precise, blunt and bloody to a planned, precise, atraumatic dissection under direct vision. The instruments that facilitate this dissection are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree