This article focuses on chemical peels for darker skin types. All races comprise a range of Fitzpatrick skin color types: light skin types in African Americans, Asians, Middle Easterners, and Latinos and dark skin types in whites. With the focus on Fitzgerald skin types IV to VI, this article discusses chemical peels, providing current information on types of peels, detailed techniques, preoperative and postoperative care, complications, hazards, and nuances of management.
This article focuses on chemical peels for darker skin types. All races comprise a range of Fitzpatrick skin color types ( Table 1 ) : light skin types III and IV in African Americans, Asians, Middle Easterners, and Latinos and dark skin type IV in whites. With the focus on Fitzgerald skin types IV to VI, the article discusses chemical peels, providing current information on types of peels, detailed techniques, preoperative and postoperative care, complications, hazards, and nuances of management. When evaluating a patient for a skin-resurfacing procedure, it is often inaccurately assumed that race and ethnicity equate with skin color. This rainbow of skin tones within any race erodes the notion that all nonwhites are dark skinned, or that all whites are light skinned.
| Type | Color | Reaction to Sun Exposure |
|---|---|---|
| I | Very white or freckled | Always burn |
| II | White | Usually burn |
| III | White to olive | Sometimes burn |
| IV | Brown | Rarely burn |
| V | Dark brown | Very rarely burn |
| VI | Black | Never burn |
In addition to the wide intraracial variation in skin color, the global population is becoming increasingly mixed. Although categorization of race and ethnicity is useful in demographic or socioeconomic evaluation, it has poor predictive value for skin-resurfacing outcomes. The American melting pot (the result of migration, wars, and inter-race relationships) shows why classification systems based on original geographic distributions have become archaic. Although the scientific literature is sparse on this topic, clinicians practicing aesthetic facial surgery and medicine should be aware of the nuances of evaluating and managing patients across the spectrum of Fitzpatrick skin types. This awareness is accentuated by the results of the 2000 US Census, which showed that Latinos are the fastest increasing minority in the United States and Filipino Americans are the fastest increasing group of Asian Americans.
International census reports illustrate similar observations. Mixed race (2 or more races in the heritage) and darker skin types (IV–VI) constitute most of the global population and one-third of the US population. Terms like mestizo, mulato, trigueno, moreno, pardo, Chindian, and Eurasian reflect how widespread and varied the mixed race has become all around the world. Celebrities like Alicia Keys (African American, Irish, Italian) and President Barak Obama (English, Cherokee, Irish, Kenyan, Scottish) reflect this phenomenon.
Histology and function
Skin types and races have key differences other than tone. The darker tone is caused by a higher melanin content within keratinocytes (the number of melanocytes is the same as in lighter skin). Dark skin contains eumelanin, a highly cross-linked dark brown to black pigment. Melanin is synthesized in melanosomes in a pathway controlled by the enzyme tyrosinase. The skin of blacks has a high content of large, singly dispersed melanosomes (stage IV) within melanocytes and keratinocytes. In contrast, pale white skin has few melanosomes in the epidermis. However, the skin of darker-skinned whites, on sun exposure, can temporarily produce melanosomes similar to black skin. Likewise, blacks with a lighter complexion have a combination of large dispersed and smaller aggregated melanosomes like whites. In Asians, skin that has not been exposed to sun has aggregated melanosomes like whites, whereas areas that have been exposed to the sun have predominantly dispersed melanosomes. These similarities and differences suggest significant intraracial and inter-racial variation in pigmentation. Recent work suggests that the activity of the protease-activated receptor-2 correlates with skin color and may influence ethnic skin color phenotypes.
The stratum corneum in skin of color has more layers and more phospholipids than white skin. The dermis tends to be thicker because of the increased number and size of fibroblasts. Because of the photoprotective nature of melanin, aging in dark-skinned individuals is associated with soft tissue and gravitational changes rather than wrinkles. Whereas whites and Asians undergo significant epidermal changes with photodamage, blacks have only marginal changes. Fibroblasts, elastic fibers, mast cells, blood vessels, hair follicles, and other dermal structures also differ in quantity and function between races.
Melanocytes are labile in darker skin, resulting in a high incidence of dyschromia, such aspostinflammatory hyperpigmentation (PIH) following injury or cutaneous surgery. Similarly, melasma is more prevalent in blacks, Hispanics, and Asians, and is attributed to hormonal factors, ultraviolet (UV) and infrared radiation exposure, and lability of melanocytes.
Indications, nuances, and hazards for chemical peeling in skin types IV to VI
Individuals with darker skin typically request correction of conditions such as PIH, melasma, acne vulgaris and scarring, textural changes (fine wrinkles), lentigos, dermatosis papulosa nigra, and seborrheic keratosis (SK). Diagnostic mistakes commonly occur in the initial evaluation of patients of dark skin. Brown lesions are lumped together as pigmented instead of hyperkeratotic-like (eg, SK). This misclassification leads to ineffective ablative treatments that may actually worsen the complexion, whether these peels are from light sources or chemicals. Chung and colleagues assessed Korean patients and found that pigmentary changes are common features of photoaging in Asians, with SK being the major pigmentary lesion in men and lentigo in women. Physicians therefore need to individualize their treatments to different types of lesions. For example, careful electrocautery of individual SK lesions is not only more effective than chemical or laser ablation, it is also safer (associated with lower risk of PIH). Long-pulsed 532-nm neodymium:yttrium-aluminum-garnet laser treatment was similarly found to be more effective and have a lower incidence of PIH for lentigines in darker-skinned patients than other modalities. Intense pulsed light has also been studied extensively in Asians for the treatment of lentigines and freckles but would be ineffective in patients with a misdiagnosis of SK. The novel use of modified phenol formulas for spot peels of lentigines (eg, with Hetter VL) had been routinely practiced for years by 1 of the authors (PPR) ( Fig. 1 ). Benign dermal tumors, such as syringomas, must be identified and treated with techniques that cause less PIH and scarring, such as fine-needle tipped electrocautery.

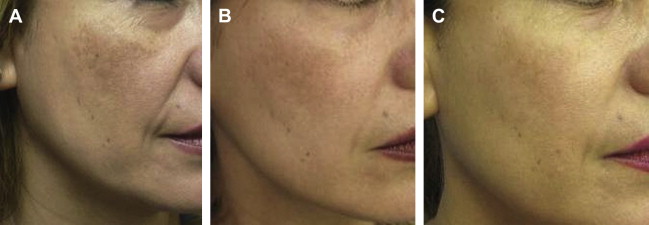
A common mistake is to treat with only 1 modality (eg, chemical peel), and then respond with a stronger peel when the results are unsatisfactory. Melasma and acne scar management are good examples. Melasma is a dysfunction of the pigmentary system, and cannot be cured with any type of peel ; it is commonly worsened by unimodal aggressive peels. These conditions require a multimodal approach. For melasma, prescription creams are recommended that address the existing melanophages, the lability of the melanocytes, the synthesis of melanin, and that promote attempts to increase cellular turnover. Protective measures require blocking of UV-B, UV-A, and infrared (heat) radiation, using physical sunblocks (oxides), cooling measures, and protective clothing and hats. The significance of inflammation as a cofactor in melasma is documented by the effectiveness of applying 0.01% fluocinolone cream twice a day, along with sun and heat protection, in achieving notable improvement ( Fig. 2 ). All resurfacing modalities should be superficial, so as to minimize the risk of PIH or hypopigmentation, because even superficial peels can cause PIH ( Fig. 3 ) if the patient is retinized. Another common condition, macular PIH, is better treated with intralesional injections of dilute triamcinolone (2 mg/mL) or fluocinolone rather than with peels.
Acne scars are categorized as ice-pick, box scar, rolling scar, atrophic, or hypertrophic types. In pigmented skin, correction of ice-pick scars, for example, is better accomplished with precise intralesional injury, which results in negligible PIH. This is achieved with chemical reconstruction of skin scars (CROSS) using a pointed toothpick or paintbrush to apply the acid ( Fig. 4 ). Shallow lesions (eg, box scars) respond to more superficial peels. Rolling scars (eg, atrophic scars with adhesions) require subcision and possible dermal fillers. Hypertrophic scars require treatment with intralesional steroids, occlusion, and pulsed-dye laser therapy.
When performing an ablative procedure on skin of color, deeper ablation, greater thermal effect, and greater inflammation of the injury all increase the risk of PIH. One of the authors (PPR) has performed more than 40,000 chemical peels in a Southern California city 10 miles north of Tijuana, Mexico, where more than 50% of the population is of Hispanic, black, Filipino, or mixed race. In this referral center for correction of acne scars, superficial, medium, and deep chemical peels are frequently combined in the same patient. For example, a stronger solution can be applied for individual ice-pick scars using the CROSS method, medium-depth peels are useful for scarred sebaceous areas, and superficial agents can be used on thinner skin overlying bony prominences ( Fig. 5 ).
As noted by Grimes, retinoids, hydroquinones (HQ), steroids, azelaic acid, and antioxidants (alone or in combinations) are used in the treatment of PIH. When used for 2 to 6 weeks before a peel, these agents provide benefit. However, when PIH occurs as a complication of other treatments, it is usually more responsive to conservative measures (within 2–3 months) (see section on Complications). Correction of PIH is easier than correction of melasma in the same patient.
Indications, nuances, and hazards for chemical peeling in skin types IV to VI
Individuals with darker skin typically request correction of conditions such as PIH, melasma, acne vulgaris and scarring, textural changes (fine wrinkles), lentigos, dermatosis papulosa nigra, and seborrheic keratosis (SK). Diagnostic mistakes commonly occur in the initial evaluation of patients of dark skin. Brown lesions are lumped together as pigmented instead of hyperkeratotic-like (eg, SK). This misclassification leads to ineffective ablative treatments that may actually worsen the complexion, whether these peels are from light sources or chemicals. Chung and colleagues assessed Korean patients and found that pigmentary changes are common features of photoaging in Asians, with SK being the major pigmentary lesion in men and lentigo in women. Physicians therefore need to individualize their treatments to different types of lesions. For example, careful electrocautery of individual SK lesions is not only more effective than chemical or laser ablation, it is also safer (associated with lower risk of PIH). Long-pulsed 532-nm neodymium:yttrium-aluminum-garnet laser treatment was similarly found to be more effective and have a lower incidence of PIH for lentigines in darker-skinned patients than other modalities. Intense pulsed light has also been studied extensively in Asians for the treatment of lentigines and freckles but would be ineffective in patients with a misdiagnosis of SK. The novel use of modified phenol formulas for spot peels of lentigines (eg, with Hetter VL) had been routinely practiced for years by 1 of the authors (PPR) ( Fig. 1 ). Benign dermal tumors, such as syringomas, must be identified and treated with techniques that cause less PIH and scarring, such as fine-needle tipped electrocautery.
A common mistake is to treat with only 1 modality (eg, chemical peel), and then respond with a stronger peel when the results are unsatisfactory. Melasma and acne scar management are good examples. Melasma is a dysfunction of the pigmentary system, and cannot be cured with any type of peel ; it is commonly worsened by unimodal aggressive peels. These conditions require a multimodal approach. For melasma, prescription creams are recommended that address the existing melanophages, the lability of the melanocytes, the synthesis of melanin, and that promote attempts to increase cellular turnover. Protective measures require blocking of UV-B, UV-A, and infrared (heat) radiation, using physical sunblocks (oxides), cooling measures, and protective clothing and hats. The significance of inflammation as a cofactor in melasma is documented by the effectiveness of applying 0.01% fluocinolone cream twice a day, along with sun and heat protection, in achieving notable improvement ( Fig. 2 ). All resurfacing modalities should be superficial, so as to minimize the risk of PIH or hypopigmentation, because even superficial peels can cause PIH ( Fig. 3 ) if the patient is retinized. Another common condition, macular PIH, is better treated with intralesional injections of dilute triamcinolone (2 mg/mL) or fluocinolone rather than with peels.
Acne scars are categorized as ice-pick, box scar, rolling scar, atrophic, or hypertrophic types. In pigmented skin, correction of ice-pick scars, for example, is better accomplished with precise intralesional injury, which results in negligible PIH. This is achieved with chemical reconstruction of skin scars (CROSS) using a pointed toothpick or paintbrush to apply the acid ( Fig. 4 ). Shallow lesions (eg, box scars) respond to more superficial peels. Rolling scars (eg, atrophic scars with adhesions) require subcision and possible dermal fillers. Hypertrophic scars require treatment with intralesional steroids, occlusion, and pulsed-dye laser therapy.
When performing an ablative procedure on skin of color, deeper ablation, greater thermal effect, and greater inflammation of the injury all increase the risk of PIH. One of the authors (PPR) has performed more than 40,000 chemical peels in a Southern California city 10 miles north of Tijuana, Mexico, where more than 50% of the population is of Hispanic, black, Filipino, or mixed race. In this referral center for correction of acne scars, superficial, medium, and deep chemical peels are frequently combined in the same patient. For example, a stronger solution can be applied for individual ice-pick scars using the CROSS method, medium-depth peels are useful for scarred sebaceous areas, and superficial agents can be used on thinner skin overlying bony prominences ( Fig. 5 ).
As noted by Grimes, retinoids, hydroquinones (HQ), steroids, azelaic acid, and antioxidants (alone or in combinations) are used in the treatment of PIH. When used for 2 to 6 weeks before a peel, these agents provide benefit. However, when PIH occurs as a complication of other treatments, it is usually more responsive to conservative measures (within 2–3 months) (see section on Complications). Correction of PIH is easier than correction of melasma in the same patient.
Types of chemical peels and formulas
Each chemical formula or component has specific effects, and can be categorized by the depth of the peel or by the mechanism of the action. Superficial peels target the stratum corneum to the papillary dermis (100 μm); medium peels penetrate to the upper reticular dermis (200 μm); and deep peels penetrate to the midreticular dermis (400 μm) ( Table 2 ). Variables such as pH, concentration, quantity applied, and concomitant use (and duration) of other chemicals modify wounding ability. In general, peels consist of α-hydroxy acids (AHA), β-hydroxy acids (BHA), trichloroacetic acid (TCA), tretinoin, or various phenolic compounds (HQ, resorcinol, and carbolic acid).
| Peel Type | Depth (μm) | Examples |
|---|---|---|
| Superficial | 100 | Glycolic acid (buffered); salicylic acid; Jessner (1 to 2 coats, nonretinized); TCA 10% to 15% (1 coat); combination peels: TCA + salicylic acid; Jessner + salicylic acid; Vi Peel/ApothePeel; Nomelan fenol kh; Melanage |
| Medium | 200 | Glycolic acid unbuffered (time dependent); Jessner (multiple coats on retinized skin); Jessner + 20% to 35% TCA; Hetter VL (phenol) |
| Deep | ≥400 | Hetter all around; Stone 100 (Grade 2); Exoderm-Lift; Baker-Gordon (not recommended) |
AHA Peels
AHA peels, particularly glycolic acid (GA) peels, function by promoting epidermolysis (corneocyte detachment), dispersing basal cell melanin, thinning the epidermis, and increasing collagen synthesis in the dermis. Unbuffered GA with a low pH has the potential to induce greater epidermal and dermal damage. GA peels are available in concentrations ranging from 20% to 99%.
BHA Peels
BHA peels, particularly salicylic acid (SA) peels, are lipophilic compounds that remove intercellular lipids that are covalently linked to the cornified envelope surrounding the epithelial cells. Studies have shown that BHA peels activate basal cells and underlying fibroblasts without directly wounding the dermis or causing inflammation. They also have antiinflammatory and antimicrobial properties. The common formulations have concentrations of 20% and 30% in ethanol.
Jessner Peel
Jessner peel is a keratolytic, which combines SA (14 g), resorcinol (14 g), and lactic acid 85% (14 g) mixed in ethanol for a final volume of 100 mL. Lactic acid is an AHA that causes epidermolysis. Resorcinol is structurally similar to phenol, and disrupts the weak hydrogen bonds of keratin.
TCA
TCA is a protein denaturant that precipitates epidermal proteins, causing sloughing and necrosis, and dermal inflammation. These processes appear as white frosting (coagulation of epidermal keratinocyte proteins) on the skin surface. Common applications combine an AHA, a BHA, or a Jessner peel, followed by TCA. The Blue Peel (Obagi Medical Products, Long Beach, CA, USA) contains a blue-dye indicator that helps the physician recognize the depth of the peel penetration ( Fig. 6 ). The recommended strength of TCA is 20% to 35%. TCA is formulated commercially or in the office as a weight-volume preparation from 10% to 100%. This versatile peel can be used to achieve superficial, medium, or deep peels, depending on the skin conditioning, the strength of the acid, and the number of coats applied. Multiple studies in the past 40 years have shown that TCA can be safely used in nonwhite dark skin types ( Fig. 7 ). Safe use of TCA requires longer preconditioning of the skin, use of the lowest effective strength of TCA, and strategies for dealing with any occurrences of PIH. As shown in the Korean study by Lee and Kim, applying TCA in a smaller area, for example inside an ice-pick scar, significantly reduces the risk of PIH and facilitates correction of PIH when it occurs.
Phenol
Phenol formulas typically consist of 88% phenol (carbolic acid), croton oil, hexachlorophene, olive oil, or distilled water ( Table 3 ). Phenol disrupts sulfide bonds, resulting in keratolysis and protein coagulation. Phenol is also melanotoxic. Hexachlorophene is an antiseptic with surfactant properties, which allows a more uniform penetration by decreasing surface tension. Croton oil is a vesicant (and therefore epidermolytic) that greatly enhances the absorption of phenol. Olive oil is added to slow the cutaneous absorption rate of these agents to reduce any systemic toxicity. Commonly used phenol formulas ( Fig. 8 ) include Hetter VL ( Fig. 9 ), Hetter all around, Stone ( Fig. 10 ), Exoderm, and Baker-Gordon. Phenol peels have the potential to cause cardiotoxicity and renal toxicity. Patients should be hydrated during the peripeel period and monitored for cardiac arrhythmias. To avoid these side effects, the peels should be administered slowly in a subunit approach. Typically, peel administration should span 60 to 90 minutes.
| Formula a | Croton Oil Content (%) | Phenol Content (%) |
|---|---|---|
| Hetter VL neck/eyelid | 0.1 | 30 |
| Stone-2 (Stone 100/Grade II) | 0.2 | 60 |
| Hetter all around | 0.4 | 35 |
| Hetter (range 0.1%–1.0%) | 0.7 | 50 |
| Exoderm-Lift | 0.6–0.7 | 64 |
| Baker-Gordon | 2.1 | 50 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







