Edwin Cortez, Fred Fedok, and Devinder Mangat address questions for discussion and debate. Do you agree or disagree, and why, with the following: “The best method to improve moderate to deep rhytids is the croton oil–phenol peel.” “There are no problems with cardiotoxicity with croton oil–phenol peels if done appropriately.” “Do not do spot testing with chemical peel agents.” How do you handle peels in advanced Fitzpatrick skin types III, IV, V? What is the main factor for rate of reepithelialization: (1) depth of peel, (2) depth of laser, (3) depth of dermabrasion? How has your approach to or technique in chemical peels evolved over the past several years?
Edwin Cortez, Fred Fedok, and Devinder Mangat address questions for discussion and debate:
- 1.
- 2.
- 3.
- 4.
How do you handle peels in advanced Fitzpatrick skin types III, IV, V?
- 5.
- 6.
Do you agree or disagree, and why, with the following: “the best method to improve moderate to deep rhytids is the croton oil–phenol peel.”
Cortez
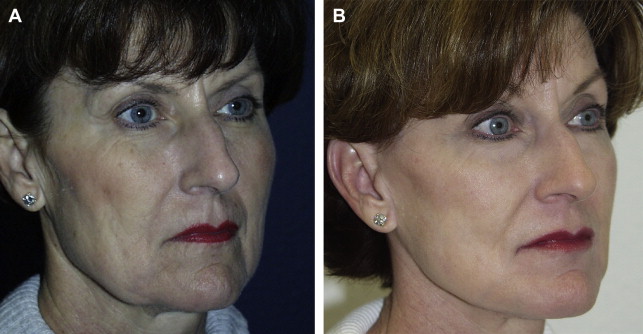
I fully agree with the statement that “the best method to improve moderate to deep rhytids is the croton oil–phenol peel ( [CR] ).” Phenol–croton oil peeling is still the standard against which all other treatment regimens for photodamaged skin are measured. In my practice, this modality is still the most safe, cost-efficient, and long-term treatment for treating medium and coarse facial rhytids. Figs. 1 and 2 show 2 of our patients before and after treatment.

The long-term criticisms of the standard Baker-Gordon peel are no longer valid. Since the elegant studies by Hetter and Stone, the entire spectrum of croton oil–phenol peeling has finally become scientifically validated. For many years, we were very pleased with our results from the Baker-Gordon formula but we have now created our own modification, which will be discussed in response to a different discussion. We have observed patients for over 25 years after being treated with croton oil–phenol preparations, and the long-term results are excellent. We are now seeing patients who we treated in their 50s and are now in their 70s and still have beautiful, firm, non-photodamaged skin. I have used dermabrasion for rhytids in the past, but in this day of problems with infectious diseases, including human immunodeficiency virus, hepatitis C, and so forth, I would prefer not to have aerosolization in my operating suite.
In the early 1990s we saw a dramatic shift to laser ablative resurfacing with the CO 2 laser. This modality was supposed to be free of any serious postoperative sequelae, such as hypopigmentation. However, 2 years after large numbers of cases were performed with the CO 2 laser, many patients were seen who developed severe hypopigmentation and also scarring and texture changes, and so forth. Now, many have put their CO 2 lasers in the garage and a new era of fractional CO 2 laser resurfacing has been born. We all hope that this expensive laser lives up to industries’ promises!
In summary, to date, we still find the croton oil–phenol peel as the best and safest modality for the treatment of moderate and deep rhytids.
Fedok
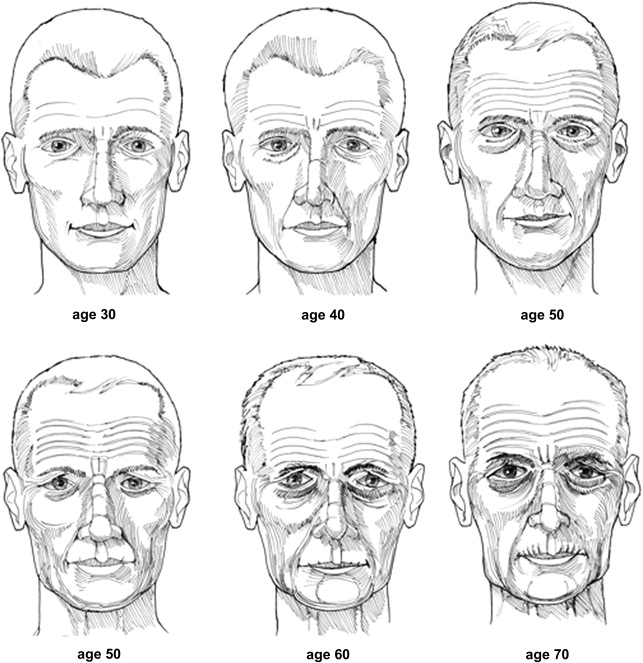
The term “rhytids” describes the wrinkled appearance of the skin caused by the decrease in skin elasticity, decrease in skin water content, and changes in collagen crosslinking that typically occurs with aging. In patients with milder aging effects, the rhytids are fairly superficial and the derangement of the anatomy is isolated to more superficial aspects of the epidermis and dermis, such as might be present in the facial skin of patients in their third decade. With more advanced skin aging the involutional and photoaging changes are more pronounced and involve deeper aspects of the dermis. In the former situation, such as in the younger patient, the rhytids usually make their early appearance around the “crow-feet” area and are largely noticeable with movement, such as smiling. In the latter situation more typical of the older patient, the rhytids may be present at repose and actually produce folds of lax skin with movement ( Fig. 3 ).
Both these situations are manageable through a plethora of resurfacing techniques. The patient with milder aging skin is managed with a variety of less aggressive techniques and modalities. The latter situation of the patient with deeper rhytids is best managed by a combination of techniques including deeper resurfacing, surgery, and possibly the utilization of injected filling material. The extent of improvement of facial skin texture and rhytids can be anticipated depending on the resurfacing technique utilized.
Box 1 displays a classification system for the grading of the severity of photoaging. Deeper rhytids along with a number of other unfavorable skin characteristics are typically encountered in patients with Grade III and IV photoaging. These patients frequently present with rhytids at rest and with readily apparent folds and laxity. These unfavorable skin characteristics are secondary to severe full-thickness skin aging. The improvement of these deep rhytids is dependent on a technique’s ability to cause changes in the deeper portions of the skin.
- •
I. Mild (28–35 years)
- ○
No keratosis, little wrinkling, no scarring, little or no makeup
- ○
- •
II. Moderate (35–50 years)
- ○
Early actinic and wrinkling, parallel smile lines, mild scarring, little makeup
- ○
- •
III. Advanced (50–65 years)
- ○
Actinic keratosis, telangiectasia, wrinkling, present at rest, always wears makeup
- ○
- •
IV. Severe (60–75 years)
- ○
Actinic keratosis, skin cancers, wrinkling, skin laxity, makeup does not cover, “cakes on”
- ○
The deeper peels with formulations based on phenol and croton oil are popularly represented as one of the standards against which all other resurfacing techniques can be compared. In my practice we have used the Baker-Gordon formulation for patients with deeper rhytids. When properly utilized in the appropriate candidate, this phenol-based peel achieves predictable and reproducibly favorable changes in skin texture and rhytids compared to other techniques. There is a wide safety margin when this peel is used by experienced practitioners. This favorable effect is only approximated by full ablative CO 2 resurfacing. In my experience, however, the Baker-Gordon formula chemical peel has produced the most remarkable results in appropriate patients with deeper rhytids, with a minimal occurrence of hyperpigmentation, spotty hypopigmentation, or other problems.
Mangat
The Baker-Gordon phenol-based peel was the gold standard for over 30 years for treating moderate to deep wrinkling on the face. This chemical peel, which was a single-strength peel, was all that was available for all skin types and various degrees of actinic damage other than the lighter and less effective trichloroacetic acid (TCA)-based peels. Between 1989 and 1995, Gregory Hetter MD carried out some groundbreaking clinical research regarding the efficacy and legitimacy of the Baker-Gordon phenol/croton oil formula and proved that it is croton oil and not phenol that is the active ingredient in the “phenol” Baker-Gordon formula. Out of this research, Dr. Hetter came up with varying strengths of chemical peels based on the concentration of croton oil from 0.1% to 1.6% that consequently varies the depth of the peel and the effectiveness of treating actinic damage and, in particular, rhytids.
I would wholeheartedly agree that the best method to improve moderate to deep rhytids is the Hetter formulation of the croton oil–phenol peel, understanding that croton oil is the active ingredient rather than phenol. The varying strength of the chemical peel solution allows one to peel different areas of the face with the appropriate strength of solution based on the thickness of the skin and the extent of rhytids in each respective area. It is no longer necessary to use one-strength chemical peel solution for the entire face. As an example, one could use a 0.4% Hetter peel for the periorbital area, which has thinner skin with mild to moderate rhytids; 0.8% or 1.2% Hetter peel for the perioral area, which has thicker skin and deeper rhytids; and 0.2% Hetter solution for the cheeks, which may demonstrate only dyschromia and no rhytids. For areas that have simply lentigines and dyschromia, one could even use a USP 89% phenol solution with no croton oil and get very effective improvement with rapid reepithelialization and minimal postpeel erythema.
In my experience of performing chemical peels for 30 years and having performed CO 2 laser resurfacing for approximately 5 years, there was no doubt about the superiority of the chemical peel resurfacing technique over the CO 2 laser resurfacing modality, purely from the standpoint of eliminating rhytids and observing the extent of improvement in actinic damage, particularly in Fitzpatrick skin types I and II. That continues to be the case with newer Hetter peel formulations. The advantage now is that one can vary the strength of the chemical peel on different parts of the face, thus reducing healing time, the extent of erythema post peel, and overall morbidity without sacrificing the result. As with the Baker-Gordon peel, the Hetter peel also demonstrates significant postpeel increase and reorganization of collagen in skin.
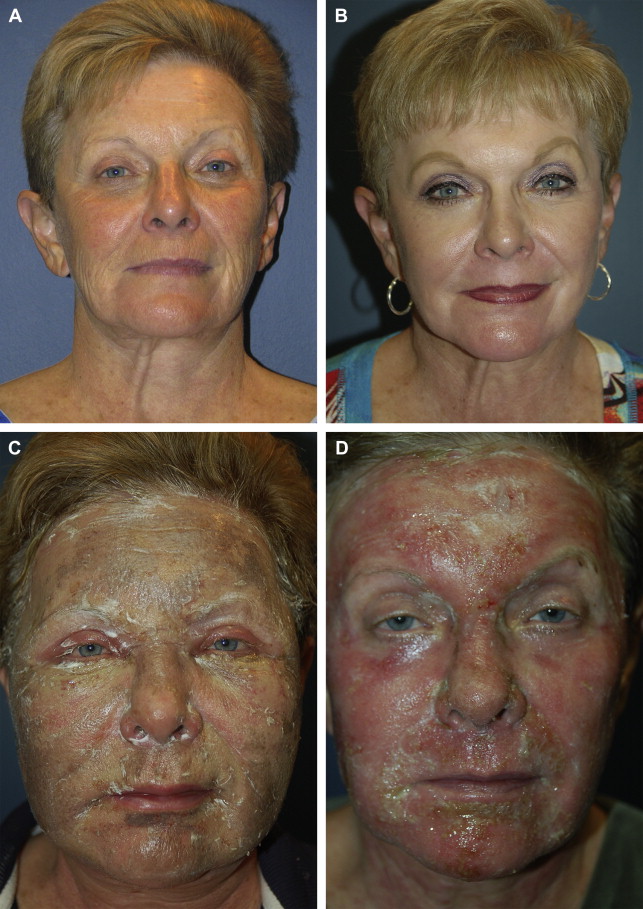
One of the biggest disadvantages of a resurfacing procedure, whether it is the use of a laser or the Baker-Gordon peel, is the extent of erythema seen in the postresurfacing period and the length of time to see a reduction/resolution of the redness.
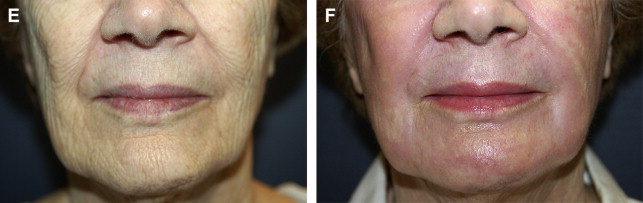
With the Hetter formula and varying the strength of the peel formula used, the amount of erythema observed is significantly diminished and, consequently, the amount of time it takes for the erythema to resolve is likewise reduced to a significant degree. Furthermore, with the Hetter croton peel, the incidence of hypopigmentation has been virtually eliminated, particularly in the Fitzpatrick type I and II skin. In the past 10 years of performing the Hetter peel, I have observed no scarring or deep pigmentation of the skin as long as the patients are carefully selected. Utilizing the 0.1% or the 0.2% croton oil peel, one can easily treat actinic damage in the neck as well as the upper chest in a controlled manner to treat lentigines and dyschromia, with little or no risk of postpeel hypopigmentation or scarring. Until the advent of the Hetter croton oil peel, peeling the neck was extremely risky using any other peeling agents such as TCA or phenol.
See Figs. 4–6 for Dr Mangat’s clinical outcomes with the Hetter croton oil peel.




Do you agree or disagree, and why, with the following: “there are no problems with cardiotoxicity with croton oil–phenol peels if done appropriately.”
Cortez
I completely agree that there are no problems with cardiotoxicity as long as the procedure is done appropriately. In personally performing over 1500 croton oil–phenol based peels, I have never seen any cardiac abnormality with full cardiac monitoring.
Historically, it has been taught that phenol and phenol-based formulas are cardiotoxic. Phenol has been shown to be directly toxic to the myocardium. In patients peeled rapidly, 50% of total surface in 30 minutes or less, tachycardia was noted initially, followed by premature ventricular contractions, premature atrial contractions, bigeminy, trigeminy, atrial tachycardia, and ventricular tachycardia. In contrast, when phenol was applied to 50% of the facial skin surface over 60 minutes, arrhythmias were not observed. Thus, it appears that higher levels of phenol absorption produce myocardial irritability.
To avoid cardiotoxicity when performing croton oil–phenol peels, follow the following regimen:
- 1.
Screen patients for cardiac disease.
- 2.
Have appropriate cardiac monitoring before, during, and after the procedure.
- 3.
Hydrate the patient before, during, and after the peel.
- 4.
Peel in aesthetic units, usually 5 units with a time lapse of 10 to 15 minutes between units. The total time for the peel should be 60 to 90 minutes.
Following this regimen should allow you to avoid any cardiotoxicity when performing croton oil–phenol peel.
Fedok
There are reported instances and concerns about the cardiotoxicity of croton oil–phenol based peels. In contrast, since I entered cosmetic practice in 1991 I have not had a patient experience any significant ectopy or arrhythmia while undergoing a phenol-based chemical peel.
Nevertheless, prevention and precaution is advised. The following is recommended and is consistent with my practice:
- •
Perform full-face phenol-based peels with the patient under cardiac monitoring.
- •
Keep the patient well hydrated.
- •
Provide intravenous access.
- •
Avoid an excess of epinephrine in local anesthetics.
- •
A full-face chemical peel is carried out in a sequence approximating the major aesthetic units of the face, so for instance, the forehead is peeled first, then the periorbital areas, then the cheeks, and so forth, until the entire face is treated. There should be a several minute pause between each area, and the entire face should take approximately 75 to 90 minutes to be treated.
The rationale of the prolonged length of time between segments is to let any absorbed phenol to dilute and dissipate between treated sections to avoid creating an excessive serum level of phenol and resultant ectopy.
Mangat
I would wholeheartedly agree that there are no problems with cardiotoxicity with any of the phenol or croton oil based chemical peels if certain precautions are taken . Cardiotoxicity is directly related to absorption of the phenol because high enough concentrations of phenol in the systemic circulation can cause ventricular extrasystoles and other arrhythmias. The same is certainly not the case with croton oil in any concentration. When we, formerly, performed the Baker-Gordon chemical peel, the following precautions were always taken:
- 1.
Adequate prepeel intravenous hydration of the patient
- 2.
Performing the peel in individual esthetic units, waiting at least 15 minutes between each unit, so that the full-face peel was performed over the course of 60 to 90 minutes
- 3.
Preoperative, intraoperative, and postoperative ECG monitoring of every patient
- 4.
Continue postoperatively intravenous hydration
Since the concentration of phenol in every Hetter solution is a constant 35%, the risk of cardiotoxicity with the Hetter peel is virtually nonexistent, allowing the operator to perform a full-face combination Hetter peel in a much shorter time period of no more than 30 minutes. The relative lack of cardiotoxicity with the Hetter–croton oil peel gives it an added advantage over the old Baker-Gordon peel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






