CHAPTER 16 Lymphedema in Pediatric Patients
KEY POINTS
Pediatric lymphedema is a chronic, impairing, progressive disorder.
Each age group within the pediatric range has its specific and distinguishing issues and needs.
Comprehensive, multifaceted holistic treatment and management produce the best outcomes.
A constant in the treatment of primary and secondary lymphedemas in pediatric patients is appropriate and adequate vascular rehabilitation.
If a surgical option is considered, the most common one is lymphovenous anastomosis.
Lymphedema, regardless of form and location, is a condition that has a low profile in the literature despite its prevalence; it is an orphan in the medical and pediatric world, even though one third of the lymphedema in the world affects pediatric populations (0 to 14 years). 1 – 9 It is important to note that a primary lymphedema patient may have an expectation of 80-year survival, whereas survival for individuals with secondary lymphedema is estimated to be only approximately 20 years. This means a longer burden on the patient, the family, the health care system, and society if the lymphedema is not recognized, treated, and managed appropriately in the very early stages. Furthermore, serious life-threatening side effects of chronic lymphedema, such as Stewart-Treves syndrome, 9 may occur more frequently in the primary lymphedema group because of its duration and severity, but there are no statistics regarding this.
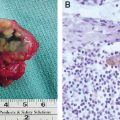
Primary lymphedema is expressed in pediatric patients as congenital, although it is not always known or identified at birth because of a lack of awareness of its possibility or a lack of screening for it. 8 One or both lower limbs are the most frequently involved initially (Fig. 16-1), but the condition may present in any part of the body. It is thought to be the result of underdevelopment of the superficial lymphatic system, which results in the presence of abnormally high levels of proteins and tissue fluids in the interstitial space. Exploration of the underlying genetic causes of certain types of primary lymphedema is helping researchers identify and understand previously unrecognized syndromes.

For primary lymphedemas (as well as secondary ones), distribution around the world is varied not only in terms of incidence and cause but also in the availability of the means for early and accurate diagnosis (sometimes lymphedema is not recognized until a vigilant therapist is consulted), the priority it is given, individual sociocultural status, and access to specialist treatment and management centers.
Diagnosis of Lymphedema in Pediatric Patients
Lymphedema (a swelling of the affected area) in pediatric patients is a sign—not a symptom. It is a sign of a disorder or malformation of some section of the lymphatic system. 10 It indicates the lymphatic system’s inability to evacuate and transport its specific fluid load (and its contents), which a healthy lymphatic system is supposed to return from the interstitial spaces to the truncal venous system.
The interstitial space is where lymph is produced and where all solutes originate that will eventually drain into the venous system. Lymph is an indispensable necessity for vertebrate life. 11 Any incompetence of the venous system for carrying its volume generates a potential overload in the lymphatic system, which is known as phlebolymphedema. The regulating mechanism of lymph formation is an activity that obviously never equals zero: lymph is “lymph” only when it enters the lymphatic system precapillaries; before that it is interstitial fluid with two pathways available for its removal, the lymphatics and the venous system.
All lymphedemas have interstitial but not necessarily lymphatic hypertension. Lymphatic hypertension is common in secondary noninflammatory lymphedemas, but not in primary lymphedemas. This knowledge is very important when making therapeutic decisions, because a surgically created lymphovenous shunt works best if there is no pressure gradient between the venous and lymphatic systems.
The part of the lymphatic system that is very important but which we do not talk about very often is that which transports chyle between the jejunum-ileum and the Pecquet cistern, and then as mixed lymph to the exit of the thoracic duct at the left shoulder (Fig. 16-2).

Primary and Secondary Lymphedema in Pediatric Patients
PRIMARY LYMPHEDEMA
Primary lymphedema is any lymphedema associated with an intrinsic or primary malfunction of the lymphatic system in all or one of the three hemicircuits, as described in Table 16-1. This may be because of interstitial issues such as fibrosis, malformations of the lymphatic vessels or nodes. 12 Interestingly it now seems likely that many apparently secondary lymphedemas may have an underlying primary component. 13 This is something we need to consider in the future in terms of early identification and anticipation of such problems (Fig. 16-3).

Hypoplasia of the lymphatic system, or hyperplasia or agenesis, either canalicular (lymph vessel) or of the lymph nodes (nodal), is not correctly called dysplasia unless it involves a short or regional system segment. In our experience, hypoplasias or hyperplasias occur more frequently than indicated in the literature about primary lymphedema. The same is true for hypotrophy. What is important to note is that the number and/or size of vessels or lymph nodes does not guarantee functionality or functional quality. Many agenesis-induced lymphedemas actually have hyperplasia of many lymph vessels. Not all dysplasias are enough to account for primary lymphedema. What is more, some dysplasias are never associated with lymphedema per se; for example, macrocystic lymphangiomas and cystic hygromas.
Thus lymphedema in pediatric patients is a chronic, impairing, progressive disorder. This chronicity has, as also occurs in secondary lymphedemas, a regional lipogenic effect. 18 , 19 We have much to learn and many problems to solve in terms of our knowledge of the underlying issues of the formation of the lymphatic system and of the treatment of it, especially in pediatric cases.
Syndromes Associated With Primary Lymphedema
There are approximately 144 syndromes associated with primary lymphedema (Fig. 16-4). 20 Among them, 22 are inherited with lymphatic malformations. Box 16-1 lists some of these conditions. 21 – 44
In addition, primary lymphedemas can be caused by malformation (LAD I and II), with or without chylous reflux, and can occur in combined angiodysplastic syndromes, as follows:
Klippel-Trenaunay-Weber syndrome: Nevus, port-wine stain, varicose veins, osteohypertrophy, overgrowth, micro AV shunts 45
Klippel-Trenaunay-Servelle syndrome: Port-wine stain, varicose veins, osteohypertrophy, overgrowth, truncular venous malformation 46 , 47
F.P. Weber syndrome: Port-wine stain, macro AV shunt, osteohypertrophy, overgrowth 48
Proteus syndrome: Tridermal and trisystemic vascular anomalies, overgrowth 49 , 50
CLOVES: Congenital lipomatous overgrowth, vascular malformation, epidermal nevi, primary or secondary scoliosis 51
N1 and N2 syndromes, including Von Recklinghausen syndrome: Neurofibromatosis, Gorrham-Stout-Haferkamp syndrome, 52 – 54 intraosseous lymphangioma
BOX 16-1 Syndromes That Can Occur With Primary Lymphedema
Yellow nail syndrome
Opitz syndrome
Noonan syndrome
Turner syndrome
PEHO syndrome
Aplasia cutis
Bronspiegel syndrome
Carbohydrate-deficient glycoprotein syndrome
Cerebellar hypoplasia
Lissencephaly
Choanal atresia
Cholestasis
Aagenaes syndrome
Lymphangiectasia
Skeletal dysplasia
Wässer syndrome
Persistent Müllerian duct syndrome
Polydactyly
Cerebral AV malformations
Avasthey syndrome
Cleft palate
Figueroa syndrome
Hypoparathyroidism
Dahlberg syndrome
Leukemia-deafness
Emberger syndrome
Microencephaly
Chorioretinopathy
Microcephaly
Cutis gyrata
Mental retardation
Müke syndrome
Facial dysmorphia
Aortic coarctation
Nevo syndrome
Hennekam syndrome
SECONDARY LYMPHEDEMA
Secondary lymphedema in pediatric patients can occur from a range of causes and situations, including the following:
Parasitic lymphedemas (filariasis). The most frequent and aggressive filaria that causes lymphedema is Wuchereria bancrofti. This worm may be as long as 11 cm and may block the lymph node system in any part of the body, but the nodes most affected are those draining the area related to the biting preferences of the mosquito. The host is human; the vector is the female Anopheles mosquito that inoculates microfilaria through its bite and capillary aspiration. Microfilaria larvae are deposited on the skin of the next carrier 24 to 96 hours after the parasite’s metamorphosis. The population at risk is about 1200 million inhabitants, mainly on the Equatorial belt, 30% of whom are children in the 0 to 14 age group. The infected population is more than 120 million, with an estimated 70 million with clinically manifest lymphedema. 55
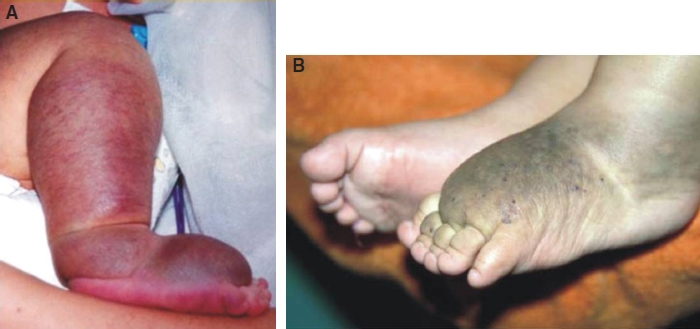
Podoconiosis. 56 , 57 This is a regional disease in tropical volcanic farming areas at elevations lower than 1200 meters (because of the temperature and the conditions of work of the farmers who are most often limited to this area). The most affected country is Ethiopia. 58 Podoconiosis involves the lower limbs as a result of the plantar absorption of volcanic minerals, which are often rich in silica. Most often it involves a nodal block at the groin. 59
Phlebolymphedema. This lymphedema results from a truncular venous malformation 60 , 61 with chronic venous hypertension. It is frequently associated with congenital lymphangioadenodyplasia. This is possibly the most frequent nonparasitic secondary lymphedema presentation in pediatric patients. It may be observed in big angiodysplastic syndromes (BAS) 62 combined, such as Klippel-Trenaunay-Weber 63 , 64 Servelle, 65 Proteo, 66 , 67 and CLOVES 68 syndromes and others.
Trauma-induced lymphedemas.
Direct trauma, generally soft tissue related (but that later form scars) within and around the lymphatic/vascular systems.
Indirect trauma, inadequate vascular access, radiotherapy, surgery.
Infections, mainly specific and chronic infections such as tuberculosis (Koch bacillus), Calmette-Guerin bacillus, and brucellosis or Malta fever (Brucella melitensis).
“Puffy hand” caused by frequent vascular access associated with drug abuse and overuse, which most frequently occurs at the left elbow fold.
Side effects and the interaction of medications (chronic anticonvulsant therapy, hormonal medications).
Hair tourniquet syndrome. 69
Amniotic band syndrome. 70
Collagen disorders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree